Abstract
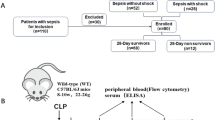
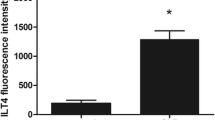
Inflammatory cells, in particular monocytes/macrophages, release pro-inflammatory mediators in response to several infectious and non-infectious stimuli. The excessive release of these mediators, resulting in the development of whole body inflammation, may play an important role in the pathogenesis of sepsis and septic shock. TNF-alpha, acting synergistically with cytokines such as IL-1, GM-CSF and IFN-gamma, is the key mediator in the induction process of septic shock, as shown in several experimental models. Based on this concept and on the encouraging results obtained in several experimental models, a number of clinical sepsis trials targeting the production or action of TNF-alpha or IL-1 have been performed in recent years. Unfortunately, these trials have failed to demonstrate a therapeutic benefit. One reason for this may be the lack of exact immunologic analyses during the course of septic disease. Recently, we demonstrated that there is a biphasic immunologic response in sepsis: an initial hyperinflammatory phase is followed by a hypo-inflammmatory one. The latter is associated with immunodeficiency which is characterized by monocytic deactivation, which we have called “immunoparalysis”. While anti-inflammatory therapy (e.g. anti-TNF antibodies, IL-1 receptor antagonist, IL-10) makes sense during the initial hyperinflammatory phase, immune stimulation by removing inhibitory factors (plasmapheresis) or the administration of monocyte activating cytokines (IFN-gamma, GM-CSF) may be more useful during “immunoparalysis”.
Similar content being viewed by others
References
Center for Disease Control (1990) Increase in national hospital discharge survey rates for septicemia—United States 1979–87. JAMA 263:937–938
Meakins JL (1989) Predisposing factors and the body's own resistance in sepsis and septic shock. In: Reinhart K, Eyrich K (eds) Sepsis. Springer, Berlin Heidelberg New York, pp 135–148
Glauser MP, Zanetti G, Baumgartner JD, Cohen J (1992) Septic shock: pathogenesis. Lancet 338:732–736
Spooner CE, Markowitz NP, Saravolatz LD (1992) The role of tumor necrosis factor in sepsis. Clin Immunol Immunopathol 62:11–17
Beutler B, Milsark IW, Cerami A (1985) Passive immunisation against cachectin/tumor necrosis factor protects mice from lethal effect of endotoxin. Science 229:869–871
Trancey KJ, Fong Y, Hesse DG, Manoque KR, Lee AT, Kuo GC, Lowry SF, Cerami A (1987) Anti-cachectin/TNF monoclonal antibodies prevent septic shock during lethal bacteraemia. Nature 330:662–664
Ohlsson K, Björk P, Bergenfeldt M, Hagemann R, Thompson RC (1990) Interleukin-1 receptor antagonist reduces mortality from endotoxin shock. Nature 348:550–552
Doherty GM, Lange JR, Langstein HN, Alexander HR, Buresh CM, Norton JA (1992) Evidence for IFN-gamma as a mediator of the lethality of endotoxin and tumor necrosis factor-alpha. J Immunol 149:1666–1670
Howard M, Muchamel T, Andrade S, Menon S (1993) Interleukin 10 protects mice from lethal endotoxaemia. J Exp Med 177:1205–1208
Spalding (1993) In shocking synergen, sepsis tallies third victim. Biotechnology 11:428–429
Fisher CJ, Dhainut JF, Opal SM, Pribble JP, Balk RA, Slotman GJ (1994) Recombinant human interleukin-1 receptor antagonist in the treatment of patients with sepsis syndrome: results from a randomized, double-blind, placebo-controlled trial. JAMA 217:1836–1843
Fisher CJ, Opal SM, Dhainut JF, Stephens S, Zimmerman JL, Nightingale P (1993) Influence of an anti-tumor necrosis factor monoclonal antibody on cytokine levels in patients with sepsis. Crit Care Med 21:318–327
Bagby GJ, Plessala KJ, Wilson LA, Thompson JJ, Nelson S (1991) Divergent efficacy of antibody to tumor necrosis factor-alpha in intravascular and peritonitis models of sepsis. J Infect Dis 163:83–88
Zanetti G, Heumann D, Gerain J et al. (1992) Cytokine production after intravenous or peritoneal Gram-negative bacterial challenge in mice—comparative protective efficacy of antibodies to tumor necrosis factor-alpha and to lipopolysaccharide. J Immunol 148:1890–1897
Eskandari MK, Bolgos G, Miller C, Nguyen DT, DeForge LE, Remick DG (1992) Antitumor necrosis factor antibody therapy fails to prevent lethality after cecal ligation and puncture or endotoxemia. J Immunol 148:2724–2730
Deitch EA (1993) Cytokines yes, cytokines no, cytokines maybe? Crit Care Med 21:817–819
Waage A, Halstensen A, Espevick T (1987) Association between TNF in serum and fatal outcome in patients with meningococcal disease. Lancet 328:355–357
Döcke WD, Reinke P, Von Baehr R, Volk HD (1994) Monitoring der monozytären HLA-DR Antigenexpression bei Transplantation und. Sepsis. In: Schmitz G, Rothe G (eds) Durchflusszytometrie in der Klinischen Zelldiagnostik. Schattauer, Stuttgart New York, pp 163–177
Volk HD, Reinke P, Falck P, Staffa G, Briedigkeit H, Von Baehr R (1989) Diagnostic value of an immune monitoring program for the clinical management of immunosuppressed patients with septic complications. Clin Transplant 3:246–252
Döcke WD, Syrbe U, Meinicke A, Platzer C, Makki A, Asadullah K, Klug C, Von Baehr R, Volk HD (1994) Improvement of monocytic function—a new therapeutic approach in sepsis? In: Reinhart et al. (eds) Update in intensive care and emergency medicine. Springer, Berlin Heidelberg New York, pp 473–488
Randow F, Syrbe U, Meisel C, Krausch D, Zuckermann H, Platzer C, Volk HD (1995) Mechanism of endotoxin desensitization: involvement of interleukin 10 and transforming growth factor-beta. J Exp Med 181:1887–1892
Platzer C, Meisel C, Vogt K, Platzer M, Volk HD (1995) Upregulation of monocytic IL-10 by tumor necrosis factor-alpha and cAMP elevating drugs. Int Immunol 7:517–523
Barsig J, Küsters S, Vogt K, Volk HD, Tiegs G, Wendel A (1995) Lipopolysaccaride-induced interleukin-10 in mice: role of endogenous tumor necrosis factor-α. Eur J Immunol 25:2888–2893
Asadullah K, Woiciechowsky C, Döcke WD, Liebenthal C, Kox W, Volk HD, Vogel S, Von Baehr R (1995) Immunodepression following neurosurgical procedures. Crit Care Med 23:1976–1981
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Volk, H.D., Reinke, P., Krausch, D. et al. Monocyte deactivation-rationale for a new therapeutic strategy in sepsis. Intensive Care Med 22 (Suppl 4), S474–S481 (1996). https://doi.org/10.1007/BF01743727
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF01743727