Abstract
Objective
To evaluate the feasibility of non-invasive ventilation (NIV) through a new interface—the helmet—in the treatment of acute respiratory failure (ARF) in hematologic children.
Design and setting
Observational, non-randomized report of four consecutive cases. Pediatric Intensive Care Unit in a university hospital.
Patients and methods
Four consecutive females (aged 9–17 years) affected by acute leukemia (3 acute lymphocytic leukemia [ALL], 1 acute myeloid leukemia [AML]) and with hypoxemic ARF (defined by severe dyspnea at rest, respiratory rate >30 breaths/min, PaO2:FiO2 <200 and active contraction of the accessory muscles). Pressure support ventilation was delivered via a helmet (CaStar,Starmed, Italy) by means of an ICU ventilator (Servo 300, Siemens Elema, Sweden).
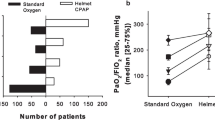
Results
We evaluated the effect of pressure support ventilation delivered by helmet on blood gases, respiratory rate, hemodynamics, patient tolerance, complication rate and outcome. An improvement of oxygenation was uniformly observed within the first 3 h after admission. The helmet was well tolerated by all children. No complication was observed. Two patients were discharged from the PICU in stable clinical conditions, whereas the remaining two children overcame the respiratory distress but had non-respiratory complications and eventually died.
Conclusion
Non-invasive ventilation via the helmet can offer effective ventilatory support and improve gas exchange in the treatment of ARF in pediatric hematologic patients. As already shown in adults, NIV may decrease the risk of life-threatening complications associated with invasive mechanical ventilation (MV), also in children with hematologic malignancies; moreover, it offers the possibility of an earlier approach to respiratory failure in this patient subset.
Similar content being viewed by others
Introduction
Acute respiratory failure (ARF) is a common complication of hematologic malignancy and it is associated with a high mortality rate. Non-invasive ventilation (NIV) should be considered first, given the possibility of avoiding the direct complications of tracheal intubation and conventional ventilation (bleeding, barotrauma, infection), thereby possibly reducing the high mortality rate related to the use of invasive ventilation.
Non-invasive pressure support ventilation (NPSV) represents a safe and effective means of treating conscious and cooperative patients with ARF, improving gas exchange, and reducing the rate of complications related to conventional mechanical ventilation (MV) [1, 2].
The new helmet interface [3] offers important advantages: an improved tolerability compared to other NPSV interfaces, a fixation system with a lower risk of cutaneous injury and the possibility of fitting it to any patient, regardless of the face contour. To our knowledge, this is the first report of helmet-NPSV (h-NPSV) application in pediatric patients.
Methods
The helmet (CaStar, Starmed, Italy) is made of transparent latex-free PVC; it is secured by two armpit braces at two hooks (anterior/posterior) on the metallic ring joining the helmet with a soft collar (Fig. 1). This collar permits neck adhesion, allowing a sealed connection. The pressure increase during ventilation makes the soft collar seal comfortably to the neck and the shoulders, avoiding air leakage. The helmet is available in three adult and one pediatric size to ensure comfort and a proper seal. The whole apparatus is connected to the ventilator by a conventional respiratory circuit. The two ports of the helmet act as inlet (upper) and outlet (lower) of the gas flows. Two seal connections with adjustable diaphragm allow the passage of tubes. The transparency of the device allows the children to see and interact with parents, nurses and their environment. The head of the bed is kept at a 30–45°angle. After helmet positioning, pressure support can be increased in increments of 2–3 cmH2O to improve ventilatory performance, as evidenced by oxygen need and respiratory rate decrease, and the disappearance of accessory muscle activity. PEEP is increased from 5 to 12 cmH2O to assure a peripheral oxygen saturation (SpO2) of at least 92% with the lowest FiO2 possible.
Antonelli et al.[4] recently demonstrated that carbon dioxide re-breathing is similar to face-mask NPSV, provided sufficient levels of pressure support are delivered. Adverse effects are limited to skin lesions when the armpit straps are not sufficiently padded.
Case reports
Case 1
A 12-year-old girl (42 kg) with relapsed acute lymphocytic leukemia (ALL), in remission after the re-induction phase of therapy with vincristine, adriblastine and dexamethasone was referred to our PICU in acute respiratory distress. She presented with a history of high-grade remittent fever, dry coughing and respiratory fatigue. Blood cultures grew Streptococcus pyogenes and ceftriaxon/amikacin therapy was introduced; teicoplanin was added due to a lack of satisfactory clinical response.
Hematologic work-up revealed pancytopenia (WBC 400 mm-3, PLT 20,000 mm-3), severe hypoxia and hypocapnia. The hypoxia responded poorly to oxygen supplementation by Venturi face mask; intercostal and jugular retractions were quite noticeable. On PICU admission, the girl was markedly polypneic (breathing rate [BR] 60–65/min, heart rate [HR] 125/min, blood pressure [BP] 125/78) and fatigued, but alert and reactive. Diffuse subcrepitant rales were present. On echocardiography, the left ventricular ejection fraction (LVEF) was 0.63; no pulmonary hypertension was documented. Helmet-NPSV was started on pressure support (starting parameters PS 12, PEEP 8, flow-triggered, FiO2 0.40). Oxygenation rapidly improved, permitting a reduction in the need for additional oxygen. Procedure discontinuation caused a rapid oxygenation drop in the first 24-36 h [Fig. 2]. Helmet ventilation was performed intermittently for 3 days and discontinued subsequently, when the patient was able to breathe on room air. A pre-admission chest CT scan demonstrated a bilateral postero-basal infiltrate that resolved almost completely on day 4 after PICU entry. The patient was referred to the Pediatric Hematology division in good clinical condition.
Case 2
A 13-year-old girl (55 kg) with ALL and hepato-renal syndrome was referred to PICU with severe respiratory distress. A pulmonary infection was suspected 1 week before the admission (leukocytosis, elevated CRP, increased oxygen need). Because of the failure of clinical response to broad spectrum antibiotics, an amphotericin B therapy was started. The hepato-renal failure lead to a diffuse edematous state and further worsened ventilatory function. Spontaneous diuresis was obtained using i.v. furosemide, dopamine, human plasma and albumin. At PICU admission the girl was hypoxic (with PaO2:FiO2 of 180—FiO2 0.50 on a Venturi oxygen mask), disoriented and restless. SpO2 was 85–88%, BR 45/min, HR 137, BP 137/90. A slight sedation was induced with midazolam (0.05 mg/kg i.v.) and h-NPSV was started on pressure support (initial parameters: PS 15, PEEP 10, FiO2 0.50, flow-trigger). On NPSV, the SpO2 increased and oxygen supplementation could be decreased to 0.25, PaO2:FiO2 increased from 180 (admission) to 360 (3 h after h-NPSV initiation). When treatment was discontinued, her need of oxygen increased again and responded to h-NPSV re-introduction [Fig. 2]. During the following days a clinical and respiratory improvement was noticed and h-NPSV was applied intermittently. On day 3 after admission the patient was taken off the ventilator. A few days later, she went into a hyperosmolar coma associated with severe sepsis. She died in multiple organ system failure (MOSF) on day 18.
Case 3
A 17-year-old female was diagnosed as having acute myeloid leukemia (AML) 4 months before the PICU admission. Following intensive chemotherapy she developed severe respiratory failure due to bilateral pneumonia. On admission anemia and thrombocytopenia were present, with 1250 mm-3 neutrophils; the girl was highly febrile (39.5°C). Chest radiogram and CT demonstrated diffuse bilateral infiltrates. Blood cultures and central venous catheter were positive for Staphylococcus aureus. Diarrhea and vomiting were present, together with a pathologic thickness of the left colic wall segment. She was treated with intravenous teicoplanin, meropenem, methronidazole and amphotericin B. On admission, her respiratory status was very poor (oxygen desaturation on FiO2 100%; PaO2:FiO2 137). She received h-NPSV with initial settings PIP/PEEP 20:8, FiO2 =1, flow-triggered, obtaining SpO2 improvement (FiO2 0.45 at 24 h). Helmet-NPSV was continued until day 4; subsequently, weaning with face-mask and Venturi mask was undertaken. She was discharged from PICU on day 8, on spontaneous breathing without oxygen supplementation. Chest CT showed a great improvement, with an area of persisting infiltration in the left postero-basal zone.
Case 4
A 9-year-old female (38 kg) had been treated for ALL since 1997. Two leukemic relapses developed and a stem cell transplant from compatible cord blood was performed. A severe graft versus host disease occurred, treated by high-dose steroids and cyclosporin A. Seizures from cyclosporin A toxicity occurred, complicated by severe respiratory failure The chest radiogram showed a bilateral, fluffy, diffuse infiltrate. Candida had been grown from previous blood cultures, which responded to intravenous amphotericin B and fluconazole. On admission to PICU, marked tachycardia and tachypnea were present, and SpO2 on FiO2 =1 was less than 80%. Helmet-NPSV was started (initial settings PIP 23, PEEP 7, back-up rate 15, flow-triggered), obtaining an oxygenation improvement and progressive breathing rate reduction; h-NPSV was continued for 36 h, then Venturi-mask periods were interposed. Chest X-ray showed a diffuse alveolar-interstitial involvement. After 3 days of spontaneous breathing on room air without any assistance, her respiratory condition worsened again and chest X-rays revealed a diffuse alveolar involvement. Blood cultures confirmed Candida tropicalis and Staphylococcus epidermidis infection. Helmet-NPSV was reintroduced (FiO2 0.50) with increased settings (PIP 28, PEEP 10, inspiratory time 33–45%).
The clinical picture was complicated by non-oliguric renal failure and thrombotic microangiopathy, which needed serial plasmapheresis. The blood film showed an impressive schistocytosis (20–30%). However, the severe hemolysis and thrombocytopenia remained unchanged, needing daily erythrocyte replacement. The respiratory status was maintained stable with h-NPSV, though her oxygen need increased to 0.70 and PaO2:FiO2 fell to 102. On day 8 tracheal intubation was needed because of sudden airway bleeding. Intensive plasma exchange and high-dose immunoglobulin and steroid pulse therapy failed to control the thrombotic-hemolytic process. Intractable bleeding occurred from both the gastrointestinal tract and airways; the patient suffered MOSF and died on day 15.
Discussion
Non-invasive ventilation through different devices is commonly used in adult patients as a valuable alternative to standard MV in respiratory failure of central or peripheral neurologic origin [5] and for the treatment of acute exacerbations of chronic respiratory failure [6]. Recently, its use has been reported both in immunocompetent and in immunosuppressed patients with hypoxemic ARF [1, 2]. Until now, this technique has also been applied in pediatric patients with mild to moderate hypoxemic ARF, but randomized controlled studies regarding its efficacy and safety are still lacking [7, 8, 9].
Acute respiratory failure is a common and severe complication of hematologic malignancies. It may result from pulmonary localization of the primary disease, infection or cardiogenic pulmonary edema. The clinical condition (frequently complicated by neutropenia and thrombocytopenia) often discourages aggressive procedures, such as invasive ventilatory support, even in the presence of severely compromised lung function. Several studies have described a very high mortality rate (ranging from 67% to 99%) in invasively ventilated patients with hematologic malignancies and bone marrow transplantation (BMT) [10, 11, 12]; even in recent studies on adults/children the combination of invasive MV with renal failure has always been associated with a poor prognosis. MOSF is the major cause of death among hematologic patients undergoing invasive ventilation [13, 14].
The bad prognosis with high mortality rate in children with BMT requiring MV due to pulmonary infection (no survivors if MV >48 h) recently reported by Jacobe et al [15] induced the authors to raise the question of whether invasive ventilation and intensive care are appropriate in these patients. Thus, an alternative approach that avoids tracheal intubation and invasive ventilation in hematologic patients with problems similar to BMT recipients (as in our series) may be an interesting alternative.
Tognet et al. [16] reported a 100% mortality rate in hematologic patients invasively ventilated for ARF versus 55% survival among patients responding to NIV. In a pilot study by Conti et al. [17] 12 out of 16 patients affected by hematologic malignancies complicated by ARF were treated successfully with a bi-level positive airway pressure ventilator (BiPAP, Respironics); NIV was delivered by means of a nasal mask. Reports of children suffering from ALL and successfully treated by face-mask NIV have been published in the past decade [18, 19, 20].
As recently demonstrated in a randomized trial, NIV in immunocompromised adults could avoid the complications of tracheal intubation (bleeding, barotrauma, secondary infections), which are often observed in these patients, with an improvement in prognosis[21]. The importance of the early application of non-invasive methods has been stressed. To summarize, hematologic patients undergoing conventional ventilation through an endotracheal tube can obtain a survival rate rarely exceeding 10% in specialized centers; the mortality derives from a mix of septic and hemorrhagic complications. In this context, NIV could represent an alternative approach and its early application appears to improve prognosis [16, 17, 21].
Non-invasive devices adopted in pediatric patients currently use few interfaces: nasal cannulas, nasal masks or face masks, whereas the BiPAP ventilator was utilized in most cases. It is well accepted that the lack of patient compliance (due to poor tolerance) may really compromise the successful application of these methods. In fact, as for other non-invasive method applications, some points should be emphasized: (1) patient cooperation may be difficult to obtain in pediatrics: in our practice only a minimal sedation with continuous midazolam infusion was performed, to avoid anxiety but also further respiratory depression (2) airway patency may be problematic when dealing with patients with copious tracheal secretions and (3) the presence of airway hemorrhage (frequently recorded in severe thrombocytopenic conditions) makes NIV impossible. The use of the new interface—the helmet—is very interesting because it circumvents the disadvantages of the face mask, though keeping the indications and benefits of a true pressure-support ventilation. In adults with hypoxemic respiratory failure, the helmet has been demonstrated to be as efficient as a face-mask with significantly fewer complications [3].
Early identification and treatment of respiratory impairment in hematologic children is highly recommended. This preliminary report suggests the efficacy and the feasibility of h-NPSV in severe ARF and may represent the basis for future larger studies, assessing its efficacy—as already demonstrated in adults—in reducing the need for intubation in children with hypoxemic ARF, too.
References
Antonelli M, Conti G, Rocco M, Bufi M, DeBlasi RA, Vivino G, Gasparetto A, Meduri GU (1998) A comparison of noninvasive positive-pressure ventilation and conventional mechanical ventilation in patients with acute respiratory failure. N Engl J Med 339:429–435
Martin TJ, Hovis JD, Costantino JP, Bierman MI, Donahoe MP, Rogers RM, Kreit JW, Sciurba FC, Stiller RA, Sanders MH (2000) A randomized, prospective evaluation of noninvasive ventilation for acute respiratory failure. Am J Respir Crit Care Med161(3 Pt 1):807–813
M.Antonelli, G.Conti, P.Pelosi, C.Gregoretti, MA Pennisi, R.Costa, P.Severgnini, M.Chiaranda, R.Proietti (2002) New treatment of acute hypoxemic respiratory failure: noninvasive pressure support ventilation delivered by helmet—a pilot controlled trial. Crit Care Med 30:602–608
Antonelli M, Pennisi MA, Pelosi P, Gregoretti C, Squadrone V, Rocco M, Cecchini L, Chiumello D, Severgnini P, Proietti R, Navalesi P, Conti G (2004) Noninvasive positive pressure ventilation by a helmet in patients with acute exacerbation of COPD—a feasibility study. Anesthesiology (in press)
Vianello A, Bevilacqua M, Arcaro G, Gallan F, Serra E (2000) Non-invasive ventilatory approach to treatment of acute respiratory failure in neuromuscular disorders. A comparison with endotracheal intubation Intensive Care Med 26(4):384–390
Peter JV, Moran JL, Phillips-Hughes J, Warn D (2002) Noninvasive ventilation in acute respiratory failure-a meta-analysis update. Crit Care Med 30(3):555–562
Padman R, Lawless S, Von Nessen S (1994) Use of BiPAP by nasal mask in the treatment of respiratory insufficiency in paediatric patients. Preliminary investigation. Pediatr Pulmonol 17:119–123
Fortenberry JD, Del Toro J, Evey L, Haase D, Jefferson LS (1993) Nasal mask bi-level positive pressure ventilation (BiPAP) in children with mild to moderate hypoxemic respiratory failure. Chest 104:133S
Akingbola OA, Hopkins RL (2001) Pediatric noninvasive positive pressure ventilation. Pediatr Crit Care Med 2:164–169
Denardo SJ, Oye RK, Bellamy PE (1989) Efficacy of intensive care for bone marrow transplant patients with respiratory failure. Crit Care Med 17:4–6
Crawford SW, Schwartz DA, Petersen FB (1988) Mechanical ventilation after bone marrow transplantation: risk factors and clinical outcome. Am Rev Respir Dis 137:682–687
Peters SG, Meadows JA III, Gracey DR (1988) Outcome of respiratory failure in hematologic malignancy. Chest 94:99–102
Kroschinsky F, Weise M, Illmer T, Haenel M, Bornhaeuser M, Hoeffken G, Ehninger F, Schuler U (2002) Outcome and prognostic features of intensive care unit treatment in patients with hematological malignancies. Intensive Care Med 28:1294–1300
Lamas A, Otheo E, Ros P, Vazquez JL, Maldonado MS, Munoz A, Martos I (2003) Prognosis of child recipients of hematopoietic stem cell transplantation requiring intensive care. Intensive Care Med 29:91–96
Jacobe SJ, Hassan A, Veys P, Mok Q (2003) Outcome of children requiring admission to an intensive care unit after bone marrow transplantation. Crit Care Med 31:1299–1305
Tognet E, Mercatello A, Polo P, Coronel B, Bret M, Archimbaud E, Moskovtchenko JF (1994) Treatment of acute respiratory failure with non-invasive intermittent positive pressure ventilation in haematological patients. Clin Intensive Care 5:282–288
Conti G, Marino G, Cogliati A, Dell’Utri D, Lappa A, Rosa G, Gasparetto A (1998) Noninvasive ventilation for the treatment of acute respiratory failure in patients with hematologic malignancies: a pilot study. Intensive Care Med 24(12):1283–1288
Akingbola OA, Servant GM, Custer JR, Palmisano JM (1993) Noninvasive bi-level positive pressure ventilation: management of two pediatric patients. Respir Care 38:1092–1098
Marino P, Rosa G, Conti G, Cogliati AA (1997) Treatment of acute respiratory failure by prolonged non-invasive ventilation in a child. Can J Anaesth 44(7):727–731
Cogliati A, Conti G, Tritapepe L, Canneti A, Rosa G (2002) Noninvasive ventilation in the treatment of acute respiratory failure induced by all-trans retinoic acid (retinoic acid syndrome) in children with acute promyelocytic leukemia. Pediatr Crit Care Med 3:70–73
Hilbert G, Gruson D, Vargas F, Valentino R, Gbikpi-Benissan G, Dupon M, Reiffers J, Cardinaud JP (2001) Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever and acute respiratory failure. N Engl J Med 344(7):481–487
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Piastra, M., Antonelli, M., Chiaretti, A. et al. Treatment of acute respiratory failure by helmet-delivered non-invasive pressure support ventilation in children with acute leukemia: a pilot study. Intensive Care Med 30, 472–476 (2004). https://doi.org/10.1007/s00134-003-2103-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-2103-6