Abstract
Objective
We describe a simplified helium dilution technique to measure end-expiratory lung volume (EELV) in mechanically ventilated patients. We assessed both its accuracy in comparison with quantitative computerized tomography (CT) and its precision.
Design and setting
Prospective human study.
Patients
Twenty-one mechanically ventilated ALI/ARDS patients.
Interventions
All patients underwent a spiral CT scan of the thorax during an end-expiratory occlusion. From the CT scan we computed the gas volume of the lungs (EELVCT). Within a few minutes, a rebreathing bag, containing a known amount of helium, was connected to the endotracheal tube, and the gas mixture diluted in the patient’s lungs by delivering at least ten large tidal volumes. From the final helium concentration, EELV could be calculated by a standard formula (EELVHe).
Measurement and results
The results obtained by the two techniques showed a good correlation (EELVHe=208+0.858×EELVCT, r=0.941; P<0.001). Bias between the two techniques was 32.5±202.8 ml (95% limits of agreement were −373 ml and +438 ml), with a mean absolute difference of 15%. The amount of pathological tissue did not affect the difference between the two techniques, while the amount of hyperinflated tissue did. Bias between two repeated helium EELV measurements was −24±83 ml (95% limits of agreement were –191 ml and +141 ml), with a mean absolute difference of 6.3%.
Conclusions
The proposed helium dilution technique is simple and reproducible. The negligible bias and the acceptable level of agreement support its use as a practical alternative to CT for measuring EELV in mechanically ventilated ARDS patients.
Similar content being viewed by others
Introduction
Acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) are commonly associated with alveolar collapse and end-expiratory lung volume (EELV) reduction [1]. Modern ventilatory strategies in ALI/ARDS patients include the use of low tidal volumes, to limit ventilator induced lung injury, and the use of PEEP. Various recruitment maneuvers aimed at re-opening collapsed lung units and improving oxygenation are often recommended [2]. Computed tomography (CT) has been shown to provide accurate measurements of tissue mass and volume of many human organs [3]. Based on the fact that lung tissue has a physical density close to water density, CT allows computation of both tissue mass and gas volume of the lung [4, 5, 6]. Several investigators have used CT to measure changes in EELV, and to quantify alveolar recruitment both in animal [7], and human [8, 9, 10] studies. Nevertheless, the risks associated with the transfer of critically ill patients to the CT suite—and with the radiological exposure—the relatively high costs, and limited availability, limit the possibility to obtain frequent repetitive measurements that would allow close monitoring of the effects of the ventilatory strategy and the evolution of lung injury.
Alternatively, several techniques based on dilution of tracer gases have been proposed in the last 20 years to measure the EELV in mechanically ventilated patients [11, 12, 13, 14, 15, 16, 17, 18, 19, 20]; these include closed circuit helium dilution [11, 12, 13, 14, 15, 16], and multibreaths open-circuit nitrogen [11, 14, 17, 18] or sulphur hexafluoride [11, 19, 20] washout. However, none has gained sufficient popularity, probably because of the complex instrumentation required. Thus, despite its potential relevance, routine measurement of EELV is uncommon, not only in clinical practice, but also in experimental settings [21].
The closed helium dilution method has often been used to measure lung volume [12, 13, 14, 15, 16]. The classical helium dilution technique, used in spontaneously breathing subjects, has been variously modified to adapt it to mechanical ventilation [16, 17]. Some authors used complex systems interposed between patient and ventilator to avoid discontinuation of ventilation preserving baseline ventilatory parameters (respiratory rate, tidal volume, and PEEP) throughout the procedure [16, 17]. Other investigators, disregarding the potential problems related to the disconnection from the ventilator, have used a simplified helium dilution technique, specifically devised for mechanically ventilated patients and which requires very simple instrumentation [22, 23, 24]. Despite its relatively frequent use, the accuracy and reproducibility of this method have never been tested. The aim of the study was to assess the accuracy and precision of this simplified helium dilution method in ALI/ARDS patients. Measurements of EELV were compared to those obtained by CT at the same PEEP level.
Materials and methods
Study population
The study population consisted of 21 non-consecutive ALI/ARDS [25] patients (mean age 57±19 years, 14 males) admitted to our ICU. The study protocol was approved by the Institutional Ethics Committee, and informed consent was obtained from patients’ next of kin. Patients scheduled for a spiral lung CT were enrolled in the study. Exclusion criteria were: organizational reasons (patients undergoing spiral CT before admission in ICU, and/or impossibility to execute the protocol during night-time or week-ends), previous history of chronic obstructive pulmonary disease (COPD), presence of air leaks from bronchopleural fistulae, and inability of the patient to sustain an apnea period during the execution of the CT. During the study period, including the transfer from ICU to the CT scan facility, patients were paralyzed, sedated, and ventilated in volume control mode (Servo 300 Ventilator Siemens, Elema, Sweden). Ventilatory parameters had been set by the attending physician according to clinical criteria. Throughout the study, heart rate, invasive arterial blood pressure, and oxygen saturation were continuously monitored.
Respiratory and hemodynamic parameters were measured less than 2 h before CT. Static compliance (Crs) and resistance (Rrs) of the respiratory system were computed by airway occlusion technique [26].
Experimental protocol
The study protocol consisted of two steps: CT acquisition and EELV measurement by the helium dilution technique (EELVHe). A spiral CT scan of the thorax was acquired by a PHILIPS Tomoscan SR 7000. Ten millimeters collimation scans were obtained at 120 kV, 250 mA, table speed 10 mm/s, and 1:1 pitch. In order to maintain a constant pressure in the airways throughout CT acquisition, the ventilator was switched to CPAP mode maintaining the set PEEP level. Thus, EELV was maintained constant throughout the entire CT scanning. Previous ventilatory settings were promptly restored at the end of the CT acquisition.
After a minimum of 5 min (considered sufficient to standardize lung history) from resuming ventilation, we measured EELVHe (Fig. 1). During an end-expiratory pause at PEEP, a flexible tube, inserted between circuit Y and the patient’s endotracheal tube or tracheostomy, was clamped. The flexible tube was then connected to a balloon filled by means of a 3-l volume calibrating syringe (model 5530, Hans Rudolph, Kansas City, Mo., USA) with 1.5 l of a gas mixture of Helium (13.44%) in oxygen. After releasing the clamp, the operator delivered to the patient at least 10 tidal volumes by rhythmically compressing the balloon to dilute the helium gas mixture with the gas contained in patient’s lungs. At the end of this procedure, the balloon was clamped off the circuit, and the patient was reconnected to the ventilator.
Scheme of helium dilution technique execution. During an end-expiratory pause, a flexible tube, inserted between circuit Y and the patient’s endotracheal tube, is clamped (panel A) and the Y connector is disconnected from it (panel B). The flexible tube is then connected to a balloon containing 1.5 liters of a gas mixture of Helium (13.44%) in Oxygen (panel C). The patient is then ventilated by rhythmical compressions of the balloon, in order to dilute helium mixture (panel D)
The concentration of helium in the balloon was then measured by a previously calibrated heliometer (PK Morgan, Chatham, England). The heliometer was a thermoconductive katharometer with a 0–14% linear measurement range and a precision of ±1% of the full scale, equipped with absorbers for carbon dioxide and humidity. EELV was then computed by the standard formula: EELVHe(ml)=(Vb*Ci/Cf)-Vb, where Vb is the initial gas volume in the bag (1.5 l, corrected from ATPD to BTPS by standard formula [27]), Ci is the initial helium concentration (13.44%), and Cf the final helium concentration [11].
In order to investigate precision of our technique, after at least 5 min of ventilation the procedure was repeated. Furthermore, in seven additional patients, pairs of EELV measurements were obtained, independently from the CT, for a total of 28 paired measurements.
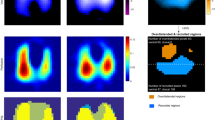
CT numerical data were stored on a PC for further analysis with dedicated software developed by two of the authors (NP and GB) with a commercial programming language (Labview 6.0, National Instruments, Austin, Tex., USA). To identify the lung region of interest (ROI), lungs profile was delineated on each CT scan image (right and left lung separately), by using a manually controlled cursor. The part of pulmonary hila containing trachea, main bronchi, and hilar blood vessels were excluded from the ROI. Each pixel of the 512×512 matrix contains the X-ray attenuation value expressed in Hounsfield units (CT number) corresponding to a volume of tissue (voxel). All voxels in the matrix have the same volume (Vvox) dependent on the size of pixels in the matrix, and thickness of CT scan (1 cm in our study):
From the Vvox and the CT number (CTvox) of each voxel in the ROI, we computed the volume of gas (GVvox) and the weight of tissue (TVvox) as:
if CTvox<0, and as:
if CTvox>0. Gas volume (EELVCT) and weight of tissue (LWCT) for the whole lungs, were computed respectively as the sum of all GVvox and TVvox of both lungs for all sections [8].
Weights of normally aerated (CT values between –500 HU and –900 HU), poorly aerated (between –100 HU and –500 HU), non-aerated (between –100 HU and +100 HU), and hyper-inflated (lower than –900 HU) tissues were computed by sum of TVvox [28]. The relative weight for each tissue class was computed as the ratio between tissue weight of each class and LWCT.
Statistics
To investigate the influence of respiratory mechanics variables, and the distribution of CT tissue classes on the accuracy of EELVHe, we analyzed the relationship between EELVHe and EELVCT by linear regression, with Crs, Rrs, and the relative weight of CT tissue classes. A value of P<0.05 was accepted as statistically significant. Bias and limits of agreement between the two techniques and between two repeated measurements by the helium dilution technique were computed as suggested by Bland and Altman [29].
Results
Table 1 summarizes the major clinical characteristics of the patients. At the time of enrollment, patients PaO2/FiO2 was 148±69 mmHg with FiO2 0.75±0.16, PEEP 12±5 cmH2O; in 11 patients ARDS was pulmonary in origin. Crs was 37.9±13.5 ml/cmH2O; Rrs was 15.6±6.7 cmH2O·l·s.
The apnea period of CT acquisition lasted 32±7 s and the EELVHe procedure lasted 37±4 s. No patient developed significant desaturation or hemodynamic instability during the CT procedure or helium dilution maneuver.
EELVCT (1,253±587 ml) and EELVHe (1,269±577 ml) were linearly correlated (EELVHe=208+0.858×EELVCT, r=0.941; P<0.001, Fig. 2). The intercept was significantly different from 0 (P<0.05, 95% confidence limit 5.2 and 410.4 ml, respectively), while the slope was slightly but not significantly different from the identity (95% confidence limit 0.71 and 1.006, respectively). Bias between the two methods was 32.5±202.8 ml (4.75±15.9%), with a 95% confidence interval limits for agreement of −373 and +438 ml, respectively (Fig. 3). The absolute percent difference computed as (EELVHe-EELVCT)/EELVCT was 14.6±10.1%.
Bland and Altman’s plot of agreement between helium dilution technique (EELVHe) and computed tomography (EELVCT). Differences between two measurements (y-axis) are plotted against their mean (x-axis). Mean difference (32.5±202.8 ml) and 95% Confidence Interval (−373 ml and +438 ml, respectively) are indicated
Bias between two EELVHe repeated measurements was –24±83 ml (−2.1±9.6%), with a 95% confidence interval limits for agreement of –191 and +141 ml, respectively (Fig. 4). The absolute percent difference computed as (EELVHe2–EELVHe1)/EELVHe1 was 6.3±7.4%. The difference between the two methods was not significantly correlated with the amount of non-aerated or poorly aerated tissue, nor with respiratory system compliance or resistance; but it was weakly correlated with the amount of hyperinflated tissue (r=0.488; P<0.05): a higher amount of hyperinflated tissue was associated with higher underestimation of lung volume by the helium dilution method.
Bland and Altman’s plot of agreement between two repeated measurements by the helium dilution technique (EELVHe1 and EELVHe2). Differences between two measurements (y-axis) are plotted against their mean (x-axis). Mean difference (−24±83 ml) and 95% Confidence Interval (−191 ml and +141 ml, respectively) are indicated
Discussion
We assessed the accuracy and precision of a simplified helium dilution method for the measurement of lung volume in mechanically ventilated patients. The technique resulted in an average 14.6% difference from lung volumes measured by CT, and showed good precision with an absolute percentage difference between repeated measurements of 6.3%.
Comparison of helium dilution with CT
Literature data support CT as an accurate estimate of both whole and gas volume of the lungs [30]. Results were obtained in models [4, 31], isolated lung [6], animal studies [5, 7], as well as in healthy subjects, and in patients affected by restrictive or obstructive disease [4, 31, 32]. A relevant aspect of lung volume measurement by CT in mechanically ventilated patients is that it is probably the only method that provides a measurement of the absolute lung volume, without requiring the use of a tracer gas. Thus, despite the fact that CT is not considered as a real gold standard for lung volume measurements, it is probably the EELV measurement method that is least affected by the pathophysiology of mechanically ventilated patients. For this reason we decided to use it as a reference method.
Several studies found that in spite of good correlations between the two methods, CT systematically underestimated the gas dilution technique [33, 34]. However, in these studies, CT measurements were obtained in the supine position, while dilution measurements were obtained in the sitting position. Moreover, in the same studies, the lung parenchyma was outlined using methods different from the one of the present study, which is similar to that used in most ARDS CT studies [7, 8]. For these reasons, it is difficult to compare our results with previous literature, and to our knowledge this is the first study comparing a dilution method with CT in mechanically ventilated ALI/ARDS patients.
Despite a negligible bias, the limits of agreement between the two methods were relatively large in our study. This means that there was not a considerable systematic error between EELVHe and EELVCT, but a substantial difference (up to ±35%) between the two methods may be found on individual measurements. Moreover, the positive intercept and the slope slightly lower than 1 suggest that EELVHe may systematically underestimate EELVCT at higher lung volumes and overestimate EELVCT at lower lung volumes.
Various factors could explain the differences between the two techniques. First, EELVHe can only measure the gas volume accessible to ventilation. Thus, all factors affecting gas mixing, and thus EELVHe accuracy, result in EELV underestimation, and an increased difference between EELVHe and EELVCT. Such factors include the size of the volume to be measured, the number and size of mixing breaths, the length of procedure, and the time constant characteristic of the various lung compartments.
Assuming that no helium mass and/or gas volume are lost during the mixing procedure, the gas volume that is measured by our technique is the gas volume contained in the lung at end expiration, accessible to mixing by manual bagging. During the gas mixing procedure, PEEP is not maintained at baseline level, while ventilation is delivered at higher tidal volumes to improve gas mixing and to decrease equilibration time. Administration of high tidal volumes could promote alveolar recruitment during the mixing procedure. However, this occurrence does not affect the accuracy of our method because the opening or closing of the alveoli will not change the amount of gas present in the lung. In this study gas mixing was obtained by delivering at least ten deep breaths. It has been shown in lung models [35], normal subjects [36, 37], and patients [12] that 95% equilibration is completed in seven to ten breaths. Patients with ARDS present a decrease in EELV, and the volume to be measured even at PEEP, is relatively small compared to normal subjects. CT studies [22] indicate that, although ARDS is an inhomogeneous disease, relatively healthy areas of the lung participate to lung exchange. This finding is also confirmed by Multiple Inert Gas Technique studies showing that hypoxia is mainly due to the presence of shunt rather than ventilation perfusion mismatch [38]. These findings suggest that, in contrast to COPD patients, the presence of slow compartment should not be relevant in ARDS patients. Based on this assumption, some investigators have used the helium rebreathing technique in ARDS patients with just six mixing breaths [15, 16]. More recent studies have shown, however, that ARDS patients may present a clinically significant expiratory flow limitation [39]. In spite of the negligible auto-PEEP (Table 1), we cannot exclude the occurrence of airway closure with distal gas sequestration and some degree of flow limitation when PEEP is removed, though the use of relatively large tidal volumes should have allowed mixing even of flow-limited regions.
A special discussion should be dedicated to the presence of overdistended areas, that receive relatively low ventilation, and that may be present in ARDS patients in association with the use of high PEEP levels. The two patients with the higher relative amount of hyperinflated tissue (2.5% and 5.7% corresponding to the 15% and 33% of all gas volume respectively), showed a higher underestimation of EELV (−410 and −292 ml, respectively), supporting the fact that when this technique is used in ARDS patients with suspected hyperinflation a higher number of mixing breaths should be delivered.
Second, EELVHe includes the anatomical and apparatus dead space, which is only partially included in EELVCT. This factor may partially explain why EELVHe tends to overestimate EELVCT, especially at lower EELV levels.
Third, the difference between the two techniques could also be related to ongoing gas exchange during both maneuvers. Though the apnea time was similar, differences in inspired oxygen fraction (clinical FiO2 during CT and the initial oxygen concentration in the bag during helium dilution), may have contributed to patient inter-individual variability in differences between the two methods.
Fourth, despite its widespread use, many factors may alter the accuracy of volume measurements by CT [40]. Aside from factors inherent to the CT method that may result in different types of image artifacts, structure movements related to heart and blood vessels pulsation, and the subjectivity of the manual procedure to contour the lung, may substantially affect CT accuracy. However, no study, to our knowledge, systematically investigated the reproducibility of CT in ARDS patients. A coefficient of reproducibility of CT measurements similar to or worse than that of the helium technique, would explain the large confidence agreement between the two methods in the absence of a significant bias.
Finally, despite good agreements between different techniques in bench studies, the agreement between techniques in spontaneously breathing [11, 20, 41] and mechanically ventilated [4, 11, 14, 20, 33] subjects are generally poor, even when different dilution methods are compared [11, 14, 20, 41]. The differences we found in our study between CT and helium are comparable to that reported for different techniques.
Helium dilution reproducibility
The helium dilution method showed good precision. The coefficient of reproducibility was comparable to that reported by other studies for different techniques [11, 12, 13, 14, 17, 18, 19, 20]. Importantly, the reproducibility of our methods was similar to that observed by other investigators with the helium dilution method in mechanically ventilated patients but using more complex instrumentation [12, 13].
Differences from other helium dilution methods
Our simplified technique differs, regarding some important features, from other previously described techniques that used the multi-breath helium dilution method in mechanically ventilated patients [12, 13, 14, 15, 16]. Most of such studies used a bag-in-box system, most commonly synchronized to start the measurement at end-expiration. Such a system allows a constant PEEP and mean airway pressure, while mechanical ventilation continues at the same tidal volume and frequency during the measurement. Major impairment of gas exchange and/or respiratory mechanics are therefore avoided. However, it requires adjunctive instrumentation that makes these methods impractical. With our method the patient is disconnected from the ventilator and PEEP is not maintained. Despite the discontinuation of PEEP, we did not observe any significant respiratory or hemodynamic complications during and after the EELV measurement. The use of high tidal volume breaths may have limited a possible decrease in mean airway pressure and impairment of gas exchange due to drops in PEEP level. Moreover, the absence of a systematic difference between repeated measurements, following 5 min at basal ventilation, suggests that the measurement maneuver caused no major losses in lung volume.
Conclusions
We found clinically acceptable limits of agreement, and a negligible bias between the proposed helium dilution technique and CT. The technique described in this study allows reliable, simple, and reproducible measurements of lung volume in mechanically ventilated ALI/ARDS patients. It could be used routinely in mechanically ventilated patients, both in clinical and experimental settings. The high precision encourages the possible use of EELVHe to estimate alveolar recruitment related to different ventilatory strategies.
References
Ware LB, Matthay MA (2000) The Acute Respiratory Distress Syndrome. N Engl J Med 342:1334–1349
Suter PM (2002) Does the advent of (new) low tidal volume bring the (old) sigh back to intensive care unit? Anesthesiology 96:795–802
Mull RT (1984) Mass estimates by computed tomography: physical density from CT numbers. Am J Radiol 143:1101–1104
Denison DM, Morgan MD, Millar AB (1986) Estimation of regional gas and tissue volumes of the lung in supine man using computed tomography. Thorax 41:620–628
Wandtke JC, Hyde RW, Fahey PJ, Utell MJ, Plewes DB, Goske MJ, Fischer HW (1986) Measurement of lung gas volume and regional density by computed tomography in dogs. Invest Radiol 21:108–117
Malbouisson LM, Préteux F, Puybasset L, Grenier P, Coriat P, Rouby JJ (2001) Validation of a software designed for computed tomography (CT) measurement of lung water. Intensive Care Med 27:602–608
Pelosi P, Goldner M, McKibben A, Adams A, Eccher G, Caironi P, Losappio S, Gattinoni L, Marini JJ (2001) Recruitment and derecruitment during acute respiratory failure: an experimental study. Am J Respir Crit Care Med 164:122–130
Malbouisson LM, Muller JC, Constantin JM, Lu Q, Puybasset L, Rouby JJ, and CT Scan ARDS Study Group (2001) Computed tomography assessment of positive end-expiratory pressure-induced alveolar recruitment in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 163:1444–1450
Tothen HU, Sporre B, Engberg G, Wegenius G, Hedenstierna G (1993) Re-expantion of atelectasis during general anaesthesia: a computed tomography study. Br J Anaesth 71:788–795
Gattinoni L, Pesenti A, Bombino M, Baglioni S, Rivolta M, Rossi F, Rossi G, Fumagalli R, Marcolin R, Mascheroni D, Torresin A (1988) Relationships between lung computed tomographic density, gas exchange, and PEEP in acute respiratory failure. Anesthesiology 69:824–832
Kendrick AH (1996) Comparison of methods of measuring static lung volumes. Monaldi Arch Chest Dis 51:431–439
Heldt GP, Peters RM (1978) A simplified method to determine functional residual capacity during mechanical ventilation. Chest 74:492–496
Weaver LJ, Pierson DJ, Kellie R, Bonner B, Craig KC (1981) A practical procedure for measuring functional residual capacity during mechanical ventilation with or without PEEP. Crit Care Med 9:873–877
Ibanez J, Raurich JM, Moris SG (1983) Measurement of Functional Residual Capacity during mechanical ventilation. Comparison of a computerized open nitrogen washout method with a closed helium dilution method. Intensive Care Med 9:91–93
Macnaughton PD, Morgan CJ, Denison DM, Evans TW (1993) Measurement of carbon monoxide transfer and lung volume in ventilated subjects. Eur Respir J 6:231–236
Macnaughton PD, Evans TW (1994) Measurement of lung volume and DLCO in acute respiratory failure. Am J Respir Crit Care Med 150:770–775
Fretshner R, Deusch H, Weitnauer A, Brunner JX (1993) A simple method to estimate functional residual capacity in mechanically ventilated patients. Intensive Care Med 19:372–376
Wrigge H, Sydow M, Zinserling J, Neumann P, Hinz J, Burchardi H (1998) Determination of functional residual capacity (FRC) by multibreath nitrogen washout in a lung model and in mechanically ventilated patients. Intensive Care Med 24:487–493
Jonmarker C, Jansson L, Jonson B, Larsson A, Werner O (1985) Measurement of functional residual capacity by sulfur hexafluoride washout. Anesthesiology 63:89–95
East TD, Wortelboer PJM, Van Ark E, Bloem FH, Peng L, Pace NL, Crapo RO, Drews D, Clemmer TP (1990) Automated sulfur hexafluoride washout functional residual capacity measurement system for any mode of mechanical ventilation as well as spontaneous respiration. Crit Care Med 18:84–91
Hedestierna G (1993) The recording of FRC— is it of importance and can it be made simple? Intensive Care Med 19:365–366
Gattinoni L, Pesenti A, Avalli L, Rossi F, Bombino M (1987) Pressure-volume curve of total respiratory system in acute respiratory failure: computed tomographic scan study. Am Rev Resp Dis 136:730–736
Gattinoni L, Pelosi P, Suter PM, et al (1998) Acute Respiratory Distress Syndrome caused by pumonary and extrapulmonary disease, different syndromes? Am J Respir Crit Care Med 158:3–11
Foti G, Cereda M, Sparacino ME, De Marchi L, Villa F, Pesenti A (2000) Effects of periodic lung recruitment maneuvers on gas exchange and respiratory mechanics in mechanically ventilated acute respiratory distress syndrome (ARDS) patients. Intensive Care Med 26:501–507
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R (1994) The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes and clinical trial coordination. Am J Respir Crit Care Med 149:818–824
Gottfried SB, Higgs BD, Rossi A, Carli F, Mengeot PM, Calverly PM, Zocchi L, Milic-Emili J (1985) Interrupter technique for measurement of respiratory mechanics in anesthetized humans. J Appl Physiol 59:647–652
(2000) Appendix C. In: Lumb (ed) Nunn’s applied respiratory physiology. Butterworth Heinemann, Oxford Auckland Boston Johannesburg Melbourne New Delhi, pp 647–649
Gattinoni L, Pesenti A, Torresin A, Baglioni S, Rivolta M, Rossi F, Scarani F, Marcolin R, Cappelletti G (1986) Adult respiratory distress syndrome profiles by computed tomography. J Thorac Imaging 1:25–30
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement Lancet 8:307–310
Clausen J (1997) Measurement of absolute lung volumes by imaging techniques (1997) Eur Respir J 10:2427–2431
Brenner DE, Whitley NO, Houk TL, Aisner J, Wiernik P, Whitley J (1982) Volume determination in computed tomography. JAMA 247:1299–1302
Brown MS, McNitt-Gray MF, Goldin JG, Greaser LE, Hayward UM, Sayre JW, Arid MK, Aberle DR (1999) Automated measurement of single and total lung volume from CT. J Comput Assist Tomogr 23:632–640
Kauczor HU, Heussel CP, Fischer B, Klamm R, Mildenberger P, Thelen M (1998) Assessment of lung volumes using helical CT at inspiration and expiration: comparison with pulmonary function tests. Am J Roentgenol 171:1091–1095
Kinsella M, Muller NL, Abboud RT, Morrison NJ, DyBuncio A (1990) Quantitation of emphysema by computed tomography using a “density mask” program and correlation with pulmonary function tests Chest 97:315–321
Darling RC, Cournand A, Richards DW Jr (1944) Studies on intrapulmonary mixture of gases: 5. Forms of inadequate ventilation in normal and emphysematous lungs, analyzed by means of breathing pure oxygen. J Clin Invest 23:55–67
Weygandt GR (1976) A sensitive five-breath N2 washout test of distribution of ventilation. J Appl Physiol 40:464–467
Russell NJ, Bagg LR, Dobrzynski J, Hughes DT (1983) Clinical assessment of a rebreathing method for measuring pulmonary gas transfer. Thorax 38:212–215
Dantzker DR, Brook CJ, Dehart P, Lynch JP, Weg JG (1979) Ventilation-perfusion distribution in adult respiratory distress syndrome. Am Rev Respir Dis 120:1039–1052
Koutsoukou A, Armaganidis A, Stavrakaki-Kallergi C, Vassilakopoulos T, Lymberis A, Roussos C, Milic-Emili J (2000) Expiratory flow limitation and intrinsic positive end-expiratory pressure et zero positive end expiratory pressure in patients with adult respiratory distress syndrome. Am J Respir Crit Care Med 161:1590–1596
Drummond GB (1998) Computed tomography and pulmonary measurements. Br J Anaesth 80:665–671
Eichler W, Schumacher J, Roth-Isigkeit A, Braun J, Kuppe H, Klotz KF (2002) Automated evaluation of functional residual capacity by oxygen washout. J Clin Monit 17:195–201
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by: MIUR
Rights and permissions
About this article
Cite this article
Patroniti, N., Bellani, G., Manfio, A. et al. Lung volume in mechanically ventilated patients: measurement by simplified helium dilution compared to quantitative CT scan. Intensive Care Med 30, 282–289 (2004). https://doi.org/10.1007/s00134-003-2109-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-2109-0