Abstract
Objectives
The American–European consensus conference (AECC) definition for acute respiratory distress syndrome (ARDS) requires a PaO2/FIO2≤200 mmHg, regardless of ventilator settings. We report the results of using standardized ventilator settings to screen and enroll ARDS patients in a clinical trial of high-frequency oscillatory ventilation (HFOV), including the impact on study enrollment, and potential effects on study outcome.
Design
Prospective cohort study.
Setting
Intensive care units in two teaching hospitals.
Participants
A consecutive sample of 41 patients with early ARDS by AECC criteria (baseline PaO2/FIO2≤200) who met all other inclusion/exclusion criteria for the HFOV trial.
Interventions
Patients were placed on standardized ventilator settings (tidal volume 7–8 ml/kg, PEEP 10 cmH2O, FIO2 1.0), and the PaO2/FIO2 was reassessed after 30 min.
Results
Seventeen patients (41.5%) had PaO2/FIO2 ratios that remained ≤200 mmHg [Persistent ARDS; PaO2/FIO2=94±36 (mean±SD)] and went on to inclusion in the HFOV study; however, in 24 patients (58.5%) the PaO2/FIO2 was >200 mmHg [Transient ARDS; PaO2/FIO2=310±74] and these patients were ineligible for the HFOV study. The ICU mortality was significantly greater (52.9 vs 12.5%; p=0.01) in the Persistent ARDS patients.
Conclusions
The use of these standardized ventilatory significantly impacted the PaO2/FIO2 ratio and therefore the ARDS prevalence and trial enrollment. These results have effects on the evaluation of the current ARDS literature and conduct of clinical trials in ARDS and hence consideration should be given to the use of standardized ventilatory settings in future ARDS trials.
Similar content being viewed by others
Introduction
Because there remains no available gold standard for the presence of acute respiratory distress syndrome (ARDS), this clinical entity is commonly diagnosed using the American–European consensus conference (AECC) definition [1, 2]. This definition, developed to lend clarity and uniformity to the diagnosis of ARDS, was designed for use in many settings including research, epidemiology, and individual patient care [1]. The AECC defined ARDS as a syndrome of inflammation and increased permeability that is associated with a constellation of clinical, radiologic, and physiologic abnormalities. Specifically, it stated that ARDS should be diagnosed when there is the acute onset of hypoxemia with bilateral infiltrates on frontal chest radiograph in the absence of left atrial hypertension. The hypoxemia criterion for ARDS is a PaO2/FIO2≤200 mmHg, regardless of positive-end expiratory pressure (PEEP) or other ventilator parameters [1].
The PaO2/FIO2 ratio, however, may be affected by other ventilator settings [3, 4, 5, 6]. Alterations in PEEP and FIO2 can dramatically change the PaO2/FIO2 ratio, and it is well established that total shunt fraction is altered by changes in FIO2. At an FIO2 of 1.0 the effects of ventilation/perfusion mismatch are eliminated and true shunt is measured [5, 6]. Ventilation with 100% oxygen can, however, induce absorption atelectasis and increase true shunt unless PEEP is applied [7, 8]. Recognition of these physiologic phenomena prompted the use of standardized procedures, such as an FIO2 of 1.0 and ≥5 cmH2O PEEP, for measuring hypoxemia and defining severe ARDS in the 1970s [9].
In the context of a clinical trial evaluating the safety and efficacy of high-frequency oscillatory ventilation (HFOV) [10], we prospectively placed consecutive patients meeting the AECC ARDS definition on standardized ventilator settings, including an FIO2 of 1.0. This was performed both to serve as the final inclusion criterion of the HFOV study, gauging the severity of hypoxemia, and to provide a uniform baseline on conventional ventilation prior to transitioning to HFOV. In this article we describe the results of this screening process, its impact on study enrollment, and its potential effects on study outcome.
Methods
The protocol for the HFOV study was approved by the research ethics boards of both participating institutions. The boards waived the need for informed consent for screening with standardized conventional ventilatory settings. Informed consent was obtained from patients (or their surrogates) who remained eligible for the HFOV trial prior to transitioning to HFOV. For this report, we obtained permission from the research ethics boards to publish non-identifying data on patients who were screened but who were not included in the HFOV study.
Patient selection
Patients in the intensive care units of two quaternary teaching hospitals (Mount Sinai Hospital, Toronto, and Cochin Hospital, Paris) who met the following criteria were prospectively screened. Inclusion criteria were: (a) age >18 years; (b) endotracheal intubation and mechanical ventilation; (c) respiratory failure as a result of one or more risk factors for ARDS; (d) bilateral infiltrates on frontal chest X-ray; and (e) hypoxemia defined as a PaO2/FIO2 ≤200 mmHg. Notable exclusion criteria included: (a) anticipated duration of ventilation <48 h; (b) >48 h since all inclusion criteria were met; (c) minimal chance of ICU survival; (d) significant heart disease; and (e) significant chronic lung disease.
Standardized conventional ventilation
During the standardized screening period all patients were ventilated with pressure control ventilation set to achieve a tidal volume of 7–8 ml/kg predicted body weight [11], ensuring peak inspiratory pressures remained <35 cmH2O. FIO2 was set at 1.0 and PEEP at 10 cmH2O or the level required to establish a SpO2 >88%, whichever was higher. The inspiratory:expiratory ratio was set at 1:2 and the respiratory rate adjusted to 15–30 breaths/minute to match previous minute ventilation.
Data gathering and statistics
Baseline data were collected after meeting initial inclusion and exclusion criteria. Physiologic, laboratory, and ventilator data were then collected after 30 min of standardized ventilator settings. All patients were eligible or excluded from the HFOV study based on their PaO2/FIO2 response to the standardized ventilator settings (using a threshold of 200 mmHg).
Student t tests were used for continuous variables and dichotomous outcomes were compared with Fisher’s exact test. All analyses were performed using standard software (Excel 2000, Microsoft, Redmond, Wash.; and SAS version 8.1, The SAS Institute, Cary N.C.). An expanded Methods section with further details on patient selection and data handling is available online in the electronic supplementary material.
Results
From March through August 2000 (Toronto center; n=20) and from March 2001 to June 2002 (Paris center; n=21), 41 consecutive patients were identified who met the inclusion and exclusion criteria in the two participating ICUs. All of these patients were screened using standardized conventional ventilation settings. In 17 patients (41%), hypoxemia was persistent (PaO2/FIO2<200 mmHg, the Persistent ARDS group) and all consented to continue into the HFOV trial; however, in 24 patients (59%; the Transient ARDS group), the PaO2/FIO2 was >200 mmHg after 30 min of standardized ventilator settings and they were thus excluded from the HFOV study.
Table 1 lists the baseline demographic data, which did not differ significantly between Persistent and Transient ARDS patients.
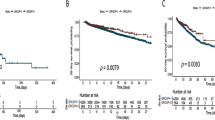
Ventilator, hemodynamic, and gas exchange data for both the Persistent and Transient groups at baseline and after 30 min of standardized ventilator settings are presented in Fig. 1 and Table 2. Baseline differences between the two groups included a higher FIO2, mean airway pressure, respiratory rate, and PEEP in the Persistent group. By design, however, all patients in both groups initially met the AECC criteria for ARDS. Because of the usual practices employed in both study ICUs, tidal volumes and PEEP levels changed only a small amount with the application of the screening settings (Table 2). The major ventilator change due to standardized settings was the use of 100% oxygen.
Baseline and standardized oxygenation and airway pressures. A–C Mean values for PaO2/FIO2, oxygenation index (OI), and mean airway pressure for each group (Persistent vs Transient ARDS) at baseline and after 30 min of standardized ventilator settings (standard). All comparisons made between Persistent and Transient ARDS groups (baseline vs baseline and standard vs standard) have p value <0.05. p value <0.05 for comparisons between baseline and standard settings values
Outcome varied greatly between the Persistent and Transient ARDS groups (Table 3). There was a large difference in mortality, duration of ventilation, and ventilator-free days, favoring the Transient ARDS group (p<0.05). No adverse effects of the standardized conventional mechanical ventilation settings were noted.
Discussion
The primary finding of this paper is that many patients meeting the American–European Consensus Conference (AECC) criteria for ARDS had a substantial alteration in their PaO2/FIO2 ratio following the early application of standardized ventilator settings using 100% oxygen and PEEP of at least 10 cmH2O. The magnitude of this change was sufficient in more than half of the cases to prevent patients from continuing to satisfy the AECC ARDS definition. The observation that ventilator settings not only affect PaO2/FIO2, but do so sufficiently to alter patient enrollment into clinical trials carries substantial implications for the study of ARDS. The possible impact of this finding is highlighted by the fact that recently published clinical trials have employed a wide range of mechanical ventilator settings during the time of enrollment and screening for the presence of ARDS [11, 12, 13, 14, 15]. Our report clearly demonstrates that an individual patient’s eligibility for an ARDS clinical trial may be affected by changes in ventilator settings, which has obvious implications in study validity and generalizability.
The PEEP and mean airway pressure levels decreased by 1 and 2 cmH2O, respectively, in both groups upon switching to standardized settings. This suggests that the improved oxygenation in the Transient ARDS group was not due to improved lung opening but rather to the elimination of the effects of ventilation/perfusion mismatching by breathing 100% oxygen [5, 6, 16]. This probable greater proportion of ventilation/perfusion mismatch relative to shunt seen in the Transient ARDS group may suggest that these patients had less severe lung pathology compared with Persistent ARDS patients.
Wide splits in mortality have been reported both by Villar et al. [17] (68 vs 23%) and the European collaborative study (61 vs 29%) when they divided patients with ARDS by AECC criteria into two groups according to their PaO2/FIO2 ratio (≤150 vs >150 mmHg) on PEEP of 5 cmH2O and an FIO2 of 0.5 [18]. The fact that these investigators studied patients 24 h after ARDS diagnosis (rather than immediately as in our study) implies, however, that their mortality differences were due not only to the findings on standardized settings, but also were related to the patients initial response to treatment. In addition, many ARDS clinical trials require recruitment to take place within a few hours of ARDS diagnosis, and thus this 24-h measurement is less helpful. Nevertheless, the findings of these studies are consistent with our data, demonstrating that patients can be divided into high- and low-risk groups for mortality based on their oxygenation response to standardized ventilator settings [17, 18].
One major concern in examining the outcomes of patients described in this report is the fact that the two groups of patients were treated differently. By design, patients in the Persistent ARDS group were treated with high frequency oscillatory ventilation (HFOV), whereas the others received conventional mechanical ventilation throughout their stay in the ICU. It is possible that HFOV contributed to the increased mortality in the Persistent patients; however, a recently completed randomized trial did not demonstrate increased mortality with HFOV compared with conventional ventilation and suggested, instead, that mortality might be lower with HFOV. In addition, it is important to recognize that the Persistent group had other baseline differences in key prognostic variables compared with the Transient patients (Tables 1, 2); these included a higher APACHE II score, an increased number with pneumonia, a lower PaO2/FIO2 ratio, and a higher oxygenation index, all of which have been independently associated with worse outcome in ARDS patients [19, 20, 21, 22].
The AECC definition was designed for use in many settings including research, epidemiology and individual patient care [1]. While laudable in terms of simplicity and generalizability, this broad set of objectives may put the AECC definition at a disadvantage in certain situations. For example, as a screening tool it would ideally be highly sensitive, but specificity and reliability are demanded in clinical trials. Similarly, ease of use and broad applicability are necessary for routine use in clinical practice, but in clinical trials researchers may need to forgo these properties in exchange for improved operating characteristics. Given the findings and concerns outlined above, the introduction of standardized ventilatory settings into an ARDS definition designed specifically for the use in clinical trials may be desirable.
Conclusion
In conclusion, increases in PaO2/FIO2 of a magnitude great enough to disqualify the diagnosis of ARDS by AECC criteria were seen in more than half of patients studied on standardized ventilatory settings. The importance of this finding to clinical trial design is potentially increased because of observed differences in outcome. Although they were treated differently (one group receiving HFOV), and it is therefore impossible to draw firm conclusions, patients whose PaO2/FIO2 exceeded 200 mmHg after standardized ventilatory settings had lower mortality, a shorter duration of mechanical ventilation, and more ventilator-free days. We propose that uniform standardized ventilator settings for patient enrollment be incorporated into future trials studying ARDS.
References
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy, LeGall JR, Morris A, Spragg R (1994) The American–European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Resp Crit Care Med 149:818–824
Ware LB, Matthay MA (2000) The acute respiratory distress syndrome. N Engl J Med 342:1334–1349
Douglas ME, Downs JB, Dannemiller FJ, Hodges MR, Munson ES (1976) Changes in pulmonary venous admixture with varying inspired oxygen. Anesth Analg 55:688–693
Suter PM, Fairley HB, Schlobohm RM (1975) Shunt, lung volume and perfusion during short periods of ventilation with oxygen. Anesthesiology 43:617–627
Shapiro BA, Crane RD, Harrison RA, Steiner MC (1980) Changes in intrapulmonary shunting with administration of 100 percent oxygen. Chest 77:138–141
McAslan TC, Matiasko-Chiu J, Turney SZ, Cowley RA (1973) Influence of inhalation of 100% oxygen on intrapulmonary shunt in severely traumatized patients. J Trauma 13:811–821
Markello R, Winter P, Olszowka A (1972) Assessment of ventilation–perfusion inequalities by arterial-venous nitrogen difference in intensive care patients. Anesthesiology 37:4–15
Santos C, Ferrer M, Roca J, Torres A, Hernandez C, Rodriguez-Roisin R (2000) Pulmonary gas exchange response to oxygen breathing in acute lung injury. Am J Resp Crit Care Med 161:26–31
Zapol WM, Snider MT, Hill D, Fallat RJ, Bartlett RH, Edmunds LH, Morris AH, Peirce EC, Thomas AN, Proctor HJ, Drinker PA, Pratt PC, Bagniewski A, Miller RG (1979) Extracorporeal membrane oxygenation in severe respiratory failure: a randomized prospective study. J Am Med Assoc 242:2193–2196
Ferguson ND, Kacmarek RM, Mehta S, Granton JT, Chiche JD, Lapinsky SE, Hallett D, Slutsky AS, Stewart TE (2001) Treatment with high-frequency oscillatory ventilation and an open-lung strategy: the TOOLS trial pilot study. Am J Respir Crit Care Med 163:A686
The Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342:1301–1308
Stewart TE, Meade MO, Cook DJ, Granton JT, Hodder RV, Lapinsky SE, Mazer CD, McLean RF, Rogovein TS, Schouten BD, Todd TR, Slutsky AS (1998) Evaluation of a ventilation strategy to prevent barotrauma in patients at high risk for acute respiratory distress syndrome. Pressure- and Volume-Limited Ventilation Strategy Group. N Engl J Med 338:355–361
Brochard L, Roudot-Thoraval F, Roupie E, Delclaux C, Chastre J, Fernandez-Mondejar E, Clementi E, Mancebo J, Factor P, Matamis D, Ranieri M, Blanch L, Rodi G, Mentec H, Dreyfuss D, Ferrer M, Brun-Buisson C, Tobin M, Lemaire F (1998) Tidal volume reduction for prevention of ventilator-induced lung injury in acute respiratory distress syndrome. The Multicenter Trail Group on Tidal Volume reduction in ARDS. Am J Respir Crit Care Med 158:1831–1838
Brower RG, Shanholtz CB, Fessler HE, Shade DM, White PJ, Wiener CM, Teeter JG, Dodd, Almog Y, Piantadosi S (1999) Prospective, randomized, controlled clinical trial comparing traditional versus reduced tidal volume ventilation in acute respiratory distress syndrome patients. Crit Care Med 27:1492–1498
Amato MB, Barbas CS, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi-Filho G, Kairalla RA, Deheinzelin D, Munoz C, Oliveira R, Takagaki TY, Carvalho CR (1998) Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 338:347–354
Gowda MS, Klocke RA (1997) Variability of indices of hypoxemia in adult respiratory distress syndrome. Crit Care Med 25:41–45
Villar J, Perez-Mendez L, Kacmarek RM (1999) Current definitions of acute lung injury and the acute respiratory distress syndrome do not reflect their true severity and outcome. Intensive Care Med 25:930–935
Squara P, Dhainaut JF, Artigas A, Carlet J (1998) Hemodynamic profile in severe ARDS: results of the European Collaborative ARDS Study. Intensive Care Med 24:1018–1028
Monchi M, Bellenfant F, Cariou A, Joly LM, Thebert D, Laurent I, Dhainaut JF, Brunet F (1998) Early predictive factors of survival in the acute respiratory distress syndrome. A multivariate analysis. Am J Respir Crit Care Med 158:1076–1081
Doyle RL, Szaflarski N, Modin GW, Wiener-Kronish JP, Matthay MA (1995) Identification of patients with acute lung injury. Predictors of mortality. Am J Respir Crit Care Med 152:1818–1824
Luhr OR, Antonsen K, Karlsson M, Aardal S, Thorsteinsson A, Frostell CG, Bonde J (1999) Incidence and mortality after acute respiratory failure and acute respiratory distress syndrome in Sweden, Denmark, and Iceland. The ARF Study Group. Am J Respir Crit Care Med 159:1849–1861
Esteban A, Anzueto A, Frutos F, Alia I, Brochard L, Stewart TE, Benito S, Epstein SK, Apezteguia C, Nightingale P, Arroliga AC, Tobin MJ (2002) Characteristics and outcomes in adult patients receiving mechanical ventilation. A 28-day international study. J Am Med Assoc 287:345–355
Acknowledgements
We thank the following individuals who participated in preliminary discussions regarding the design of the multi-center HFOV study: M.B.P. Amato, J.T. Granton, S. Grasso, N.R. MacIntyre, V.M. Ranieri, and A.S. Slutsky. Thanks also to R. MacDonald for his assistance with patient screening and data collection. The Ontario Thoracic Society and Physicians’ Services Incorporated supported this work. N. Ferguson was supported by a Canadian Institutes of Health Research / Canadian Lung Association Post-Doctoral Fellowship.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Ferguson, N.D., Kacmarek, R.M., Chiche, JD. et al. Screening of ARDS patients using standardized ventilator settings: influence on enrollment in a clinical trial. Intensive Care Med 30, 1111–1116 (2004). https://doi.org/10.1007/s00134-004-2163-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-004-2163-2