Abstract
Objective
Evidence that PS may facilitate weaning from mechanical ventilation (MV), although not confirmed by randomized trials, prompted us to investigate whether patients could be weaned with PS after failing a T-tube trial.
Design and setting
This was a prospective, non-randomized study in two French intensive care units.
Patients and participants
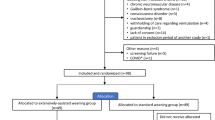
One hundred eighteen patients were enrolled and underwent a T-tube trial, after which 87 were extubated. Thirty-one underwent a further trial with PS, after which 21 were extubated.
Interventions
All patients under MV >24 h meeting the criteria for a weaning test underwent a 30-min T-tube trial. If this was successful, they were immediately extubated. Otherwise, a 30-min trial with +7 cm H2O PS was initiated with an individualized pressurization slope and trigger adjustment. If all weaning criteria were met, the patients were extubated; otherwise, MV was reinstated.
Measurements and Results
The extubation failure rate at 48 h did not differ significantly between the groups: 11/87 (13%) versus 4/21 (19%), P=0.39. The groups were comparable with regard to endotracheal tube diameter, MV duration, the use of non-invasive ventilation (NIV) after extubation, initial severity score, age and underlying pathology, except for COPD. A significantly higher percentage of patients with COPD was extubated after the trial with PS (8/21–38%) than after a single T-tube trial (11/87–13%) (P=0.003).
Conclusions
Of the patients, 21/118 (18%) could be extubated after a trial with PS, despite having failed a T-tube trial. The reintubation rate was not increased. This protocol may particularly benefit patients who are most difficult to wean, notably those with COPD.
Similar content being viewed by others
Introduction
Randomized studies [1, 2] assessing trials of weaning from mechanical ventilation (MV) detected no difference between spontaneous breathing trials with a T-tube (VST) and those with pressure support at 7 cm H2O (PSV). On the basis of these data, the consensus conference of the Francophone Intensive Care Society on weaning from mechanical ventilation [3] judged the two tests to be equally valid when establishing the clinical criteria for weaning. Several published findings [4, 5, 6, 7, 8, 9] demonstrate that the excess workload imposed by breathing through an endotracheal tube can be compensated by the use of 7 cm H20 pressure support. This excess load may be even greater in patients with an already diminished work of breathing [10].
All these data suggest that if the load is balanced by the work of breathing, a T-tube trial may be successful in the patients who are easiest to wean. In other cases (patients failing the T-tube trial), the use of pressure support (7 cm H2O) could provide a means of decreasing the excess load. This might enable certain patients to meet the weaning criteria and benefit from earlier extubation, even when this does not appear to be justified on the basis of a single T-tube trial. This hypothesis led us to investigate the possibility of weaning patients from MV following a spontaneous breathing trial with pressure support at 7 cm H2O after the previous failure of a T-tube trial.
Materials and methods
Study design
This was a prospective, non-randomized study conducted between April 2003 and September 2004 in two French adult medico-surgical intensive care units. The protocol was approved by our institutional ethics committee.
Inclusion criteria
All patients under MV for at least 24 h were included as soon as they met the criteria for a weaning test [3], i.e., they showed improvement in the underlying pathology, required no vasoactive medication or sedation, were capable of responding to a simple positive order and were adequately oxygenated (PaO2 >60 mmHg with FiO2 ≤0.5 and PEEP ≤5 cmH2O). Each subject was included in the study only once. Tracheotomized patients and patients for whom a decision on treatment restriction was pending were excluded. The same type of ventilator (EVITA 4, Dragger) was used for all the patients enrolled in this study.
Protocol
After the patient had been informed about the procedure and had undergone endotracheal aspiration, he or she was placed in a semi-sitting position and subjected to a T-tube trial for 30 min. The following parameters were measured continuously throughout the study: blood pressure (BP), SpO2 (pulse oximetry), heart rate (HR) and respiratory frequency (RF) using a Siemens XL 9000 monitor. The physician responsible for the patient was present at the clinical assessment. No change was made in the patient’s treatment or position during the test.
The weaning criteria were those recommended by the consensus conference [3]: absence of any clinical sign of respiratory distress (retractions, thoraco-abdominal paradox, agitation, perspiration, etc.), SpO2 ≥90% with FiO2 ≤0.5, RF ≤35/min and the absence of a 20% variation in RF or BP. If all these criteria were met, the patient was extubated respecting the standard procedures, including the use of oxygen, respiratory physiotherapy and, if appropriate, aerosol treatment. In the event of a major bronchial obstruction, non-invasive ventilation (NIV) could be employed in addition to short-term corticosteroid treatment if laryngeal dyspnea was suspected.
If the patient met one or more criteria of extubation failure in the T-tube trial, pressure support was initiated immediately and continued for 30 min at 7 cm H2O if a heating humidifier was used or at 10 cm H2O with an antibacterial humidifying filter [11, 12]. The other adjustments consisted in applying a PEEP =0 cm H2O and a FiO2 ≤0.5, setting the trigger at the highest possible sensitivity level to avoid automatic triggering and adapting the pressurization slope individually to each patient. The same parameters were monitored and recorded as in the T-tube trial. If the patient met all weaning criteria, he or she was extubated using the same standard procedures. Otherwise, in the event of persistence (or aggravation) of several criteria denoting extubation failure, invasive ventilation was reinstated and adjusted.
Evaluation
The principal endpoint was the comparison of the rates of extubation failure within the first 48 h between patients extubated after a T-tube trial alone and those extubated after a further trial with pressure support. The decision to reintubate was taken by the physician responsible for the patient. The principal cause of extubation failure was recorded, noting in particular whether the failure was due to a problem of extubation feasibility (upper airway obstruction and bronchial congestion) when NIV was unsuccessful or weaning feasibility in other cases of respiratory distress. The effect of pressure support on the parameters indicating failure of the patient to meet the weaning criteria during the T-tube trial was also evaluated.
Statistics
Demographic and physiological variables are expressed as the means ± SD. Qualitative and quantitative variables were compared using Fisher’s exact test and the Mann-Whitney test, respectively.
Results
A total of 118 consecutive patients were enrolled and underwent an initial T-tube trial. Of these, 87 met all weaning criteria and could be extubated at the end of this first trial (T-tube group). A further 31 subjects presented one or more criteria of weaning failure (mean time to occurrence =14±6.8 min) and therefore underwent a further trial with PS. Of these 31 patients, 21 (68%) then succeeded in meeting all weaning criteria and were extubated (PS group). No difference in the reintubation rate at 48 h was observed between the T-tube (11/87 patients =13%) and PS (4/21=19%) groups (Fig. 1, Table 1). The two groups were comparable in terms of age, severity score (Igs2), duration of MV prior to the weaning test and the use or failure of NIV post-extubation (Table 2). The two groups were also comparable in terms of underlying pathologies with the exception of decompensated COPD. Among the 23 patients with COPD (steady state FEV1 =1.39±0.4 l), 11 could be extubated after a T-tube trial alone and 8 after a further trial with PS (P=0.003), with no difference in the extubation failure rate (3 and 2 subjects respectively, P=0.9).
No difference in the mortality rate was observed between the T-tube group (5/87 patients) and PS (2/21). This result and the outcome of patients who were reintubated or still failed to meet the weaning criteria with the two trials are shown in Table 3.
Of the 31 patients failing the T-tube trial, none presented signs of left ventricular failure, and most (29 patients =94%) presented only one criterion of extubation failure. The values of these extubation failure criteria, and their evolution during the trial with PS, are shown in Table 2. During the trial with PS, the pressurization slope and trigger setting were adjusted individually for each patient, with values ranging from 0 to 0.2 s and from 0.3 to 0.5 l/min, respectively.
Discussion
Despite the data from randomized studies and from the consensus conference of the Francophone Intensive Care Society, the results of our study suggest that an appreciable proportion of patients who appear to be unweanable on the basis of a T-tube trial can be extubated without an increased extubation failure rate after a further trial with PS. Our protocol nevertheless had several limitations, probably the most important of these being the absence of randomization. It cannot be excluded that a patient failing to meet the weaning criteria after an initial test with PS might succeed in meeting these after a further T-tube trial initiated immediately afterwards. However, such a procedure would be contrary to the recommendations of the consensus conference. A second potential limitation is the diagnosis of failure in the T-tube trial, with 94% of the patients presenting only one criterion of failure, but again, this was based on consensual practices. A third limitation is the absence of precise criteria for reintubation, these being appraised by the physician responsible for the patient. Another limitation is the small number of patients: it cannot be excluded that with a larger number the difference in failure rates could have become significant. The final limitation is the homogeneity of the diameters of the endotracheal tubes of small caliber in our study. It cannot be excluded that had larger caliber endotracheal tubes been used, the results might have been different [13].
Published data [14, 15] suggested that T-tube trials most closely approximated the work of extubated breathing. In contrast, our results suggest a high rate of false negatives for successful weaning with the T-tube trial. These results are not explained by disparities in the endotracheal tube diameter or by disparities in the extent of obstruction related to different durations of MV. Our results could suggest that PSs underestimate the work of breathing following extubation. But Esteban’s randomized study [1] detected no difference for extubation failure between the two groups. This suggested that PS does not unload the respiratory muscles sufficiently to make a big difference in a larger cohort of patients.
The systematic individual adjustment of the trigger setting and pressurization slope to each patient during the trial with PS might possibly provide an explanation for our results. This adjustment could have contributed to a better patient-ventilator synchronization [16, 17, 18], which in turn might have increased the number of patients meeting the weaning criteria in the PS group. This could explain the results obtained, particularly with regard to the patients with a marked deterioration in the work of breathing (those with COPD) [19]. Specific adjustment of these parameters is not mentioned in the randomized trials.
Conclusions
Our study, taking into account published data and consensual criteria, evaluated the benefit of weaning patients from MV using PS (with optimized patient-ventilator synchronization) immediately following the failure of a T-tube test. Our results show that 21 out of 118 patients (18%) could be extubated earlier using this procedure, with no increase in the rate of reintubation. This weaning protocol could be applied in particular to the patients most difficult to wean, notably those with COPD. A comparative, randomized study design to confirm these results is needed.
References
Esteban A, Alia I, Gordo F, Fernandez R, F. Solsona J, Vallverdu I, Macias S, M. Allegue J, Blanco J, Carriedo D, Leon M, A. de la Cal M, Taboada F, Gonzales de Velasco J, Palazon E, Carrizosa F, Tomas R, Suarez J, Goldwasser R, for the Spanish Lung Failure Collaborative Group (1997) Extubation utcome after spontaneous breathing trials with T-Tube or pressure support ventilation. Am J Respir Crit Care Med 156:459–465
Farias JA, Retta A, Alia I, Olazarri F, Esteban A, Golubicki A, Allende D, Marliartchuk O, Peltzer C, Ratto ME, Zalazar R, Garea M, Moreno E (2001) A comparison of two methods to perform a breathing trial before extubation in pediatric intensive care patients. Int Care Med 27:1649–1654
Richard C, Beydon L, Cantagrel S, Cuvelier A, Fauroux B, Garo B, Holzapfel L, Lesieur O, Levraut J, Maury E, Polet C, Roche N, Roeseler J (2001) Weaning from mechanical ventilation. Consensus recommendations. Reanimation 10:697–698
Fiastro JF, Habib MP, Quan SF (1988) Pressure support compensation for inspiratory work due to endotracheal tubes and demand continuous positive airway pressure. Chest 93:499–505
Straus C, Louis B, Isabey D, Lemaire F, Harf A, Brochard L (1998) Contribution of the endotracheal tube and the upper airway to breathing workload. Am J Respir Crit Care Med 157:23–30
Brochard L, Rua F, Lorino H, Lemaire F, Harf A (1991) Inspiratory pressure support compensates for the additional work of breathing caused by the endotracheal tube. Anesthesiology 75:739–745
Nathan SD, Ishaaya AM, Koerner SK, Belman MJ (1993) Prediction of minimal pressure support during weanig from mechanical ventilation. Chest 103:1215–1219
Kuhlen R, Max M, Dembinski R, Terbeck S, Jurgens E, Rossaint R (2003) Breathing pattern and workload during automatic tube compensation, pressure support and T-piece trials in weaning patients. Eur J Anaesthesiol 20:10–16
Conti G, De Blasi RA, Lappa A, Ferretti A, Antonelli M, Bufi M, Gasparetto A (1994) Evaluation of respiratory system resistance in mechanically ventilated patients: the role of the endotracheal tube. Int Care Med 20:421–424
Richard J, Clabault K (2001) Modalities of spontaneous breathing trials. Réanimation 10:738–743
Pelosi P, Solca M, Ravagnan I, Tubiolo D, Ferrario L, Gattinoni L (1996) Effects of heat and moisture exchangers on minute ventilation, ventilatory drive, and work of breathing during pressure-support ventilation in acute respiratory failure. Crit Care Med 24:1184–1188
Girault C, Breton L, Richard JC, Tamion F, Vandelet P, Aboab J, Leroy J, Bonmarchand G (2003) Mechanical effects of airway humidification devices in difficult to wean patients. Crit Care Med 31:1306–1311
Shah C, Kollef MH (2004) Endotracheal tube intraluminal volume loss among mechanically ventilated patients. Crit Care Med 32:120–125
Ishaaya AM, Nathan SD, Belman MJ (1995) Work of breathing after extubation. Chest 107:204–209
Swinamer DL, Fedoruk LM, Jones RL, Chin WD, Phang PT, Hamilton SM, King EG (1989) Energy expenditure associated with CPAP and T-piece spontaneous ventilatory trials. Changes following prolonged mechanical ventilation. Chest 96:867–872
Bonmarchand G, Chevron V, Menard JF, Girault C, Moritz-Berthelot F, Pasquis P, Leroy J (1999) Effects of pressure ramp slope values on the work of breathing during pressure support ventilation in restrictive patients. Crit Care Med 27:715–722
Aslanian P, El Atrous S, Isabey D, Valente E, Corsi D, Harf A, Lemaire F, Brochard L (1998) Effects of flow triggering on breathing effort during partial ventilatory support. Am J Respir Crit Care Med 157:135–143
Mancebo J, Amaro P, Mollo JL, Lorino H, Lemaire F, Brochard L (1995) Comparison of the effects of pressure support ventilation delivered by three ventilators during weaning from mechanical ventilation. Int Care Med 21:913–919
Bonmarchand G, Chevron V, Chopin C, Jusserand D, Girault C, Moritz F, Leroy J, Pasquis P (1996) Increased initial flow rate reduces inspiratory work of breathing during pressure support ventilation in patients with exacerbation of chronic obstructive pulmonary disease. Int Care Med 22:1147–1154
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ezingeard, E., Diconne, E., Guyomarc’h, S. et al. Weaning from mechanical ventilation with pressure support in patients failing a T-tube trial of spontaneous breathing. Intensive Care Med 32, 165–169 (2006). https://doi.org/10.1007/s00134-005-2852-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2852-5