Abstract
Purpose
Assessing feasibility and physiological effects of sedation with sevoflurane, administered with the anesthetic conserving device (AnaConDa), in comparison with propofol and remifentanil.
Methods
Seventeen patients undergoing mechanical ventilation underwent sedation with sevoflurane delivered with AnaConDa (phase SevAn), preceded and followed by sedation with propofol and remifentanil (phases ProRe1, ProRe2), with the same sedation targets.
Results
With both strategies it was possible to achieve the sedation targets. Time required to sedate and awake patients was greater during SevAn than ProRe1: respectively, 3.3 ± 3.0 versus 8.9 ± 6.1 and 7.47 ± 5.05 versus 16.3 ± 11.4 min. During SevAn the PaCO2 and minute ventilation increased. Hemodynamics was stable between ProRe1 and SevAn, except for an increase in heart rate in the SevAn phase. Environmental pollution from sevoflurane was within the safety limits.
Conclusions
Sevoflurane can be effectively and safely used for short-term sedation of ICU patients with stable hemodynamic conditions.
Similar content being viewed by others
Introduction
Sedation is an extremely common practice in the intensive care unit (ICU). It is provided to the patients with the aim of reducing their discomfort and anxiety, facilitating medical and nursing procedures, increasing patients’ tolerance to invasive devices (such as endotracheal tube), and to mechanical ventilation [1, 2].
The ideal sedative drug should be effective in providing sedation, should have a rapid onset and resolution of the effect, should not accumulate over time, and have minimal side effects, particularly not hampering hemodynamic stability. Benzodiazepines and propofol, although far from being ideal drugs have a widespread diffusion in the ICU practice [3].
Halogenated gases are powerful anesthetics, daily used in the operating rooms for the maintenance of general anesthetic and also suitable to provide dose-dependent sedation [4]. Among the halogenated gases, sevoflurane has a lower solubility (providing faster induction and recovery and lower accumulation in the tissues) and causes minimal cardiac depression, allowing maintaining more stable hemodynamic conditions; moreover, sevoflurane is a powerful bronchodilator and exerts a protective action on the myocardium [5]. For these characteristics a rationale for its application in the ICU setting appears justified.
In the operating rooms halogenated gases are usually delivered by dedicated anesthesia machines, which, by means of a closed gas circuit, are able to keep a constant inspired gas fraction, with relatively low consumption of fresh gases. The anesthetic conserving device (AnaConDa) is a tool devised to provide sedation with halogenated gases while mechanical ventilation is delivered through ICU mechanical ventilators. The AnaConDa has been used to provide sedation in ICU patients with isoflurane [6] and sevoflurane [7].
The aim of the present study is to assess, in a short-term evaluation, the feasibility of sedation with sevoflurane in a mixed ICU population, and to assess the physiological effect of this approach compared with the intravenous infusion of sedative drugs. Moreover, we aimed at estimating the level of environmental pollution from sevoflurane, a potentially relevant drawback of inhalational sedation.
Methods
Study design
We conducted a prospective cross-over study between January 2005 and August 2006 in our eight-bed general ICU, San Gerardo Hospital, Monza, Italy. The study was approved by the ethical committee of our institution and an informed consent was obtained according to committee’s recommendations (consent was delayed until after the patients had recovered from the effects of sedation).
Anesthetic conserving device (AnaConDa)
AnaConDa® (Hudson RCI®, Uppland Väsby, Sweden) is a small (47-g weight) modified heat-moisture exchanger. We fitted it on each patient between the Y-piece of the respiratory circuit and the endotracheal tube by ISO-standard connectors. AnaConDa allows direct administration of anesthetic gas to the breathing circuit via a syringe pump [8, 9]. In the present study we infused sevoflurane through an evaporator rod in the AnaConDa. Sevoflurane was then inhaled by the patient and its inspiratory and expiratory concentrations were continuously monitored trough a dedicated sampling line and monitor (Scio Module, Dräeger Medical, Lubeck). Approximately 90% of the exhaled gas is absorbed by a lipophilic filter in the AnaConDa and returned to the patient at the next inhalation. Consequently, only a small amount of anesthetic gas passes the filter and is released through the expiratory outlet of the ventilator. Scavenging of sevoflurane not absorbed by the lipophilic filter is performed from the expiratory outlet of the ventilator by a standard evacuation system (Fig. 1).
Ventilatory circuit setting during sedation with the AnaConDa device (7). Sevoflurane is injected in the device by a syringe pump (6). The device (7) is inserted between the circuit Y and the opening of the endotracheal tube. At the same site gas is sampled by a dedicated line (1) and sevoflurane inspiratory and expiratory concentrations monitored (2). A scavenging system (3, 5) collects the exhaled gases, containing only a minimal amount of sevoflurane, as most is retained by the AnaConDa
Sedation level
Sedation in our patients was evaluated by means of two extensively validated clinical scores: Ramsay score [3], which ranges from 1 (anxious, agitated and restless patient) to 6 (asleep and unarousable); and Richmond agitation sedation scale (RASS) [10], which ranges from −6 (unarousable) to 4 (combative). In every study phase (see below), we defined “time-to-action” as the time necessary from the beginning of the phase (characterized by a specific sedation strategy) to reach both a stable (>5 min) Ramsay score ≥4 and a RASS ≤ −3, which were our target sedation values; the 5-min period required to confirm the stability of the sedation was not taken into account in the “time-to-action”, as the set sedation level had to be achieved at the beginning of the 5 min. Analogously, at the end of each sedation phase we defined “time-to-awakening” the time necessary to reach both a stable Ramsay score ≤2 and RASS ≥ 0. Moreover, the level of sedation was continuously monitored by bispectral index (BIS A 2000 XP™, Aspect Medical Systems Inc., Natick, MA). BIS is an electro-encephalogram (EEG)-derived parameter which ranges from 0 (flat EEG) to 100 (awake, responsive patient) [11]; BIS sensors were applied on each patient’s forehead as specified by manufacturer’s instructions.
Study population
Patients admitted to our ICU and mechanically ventilated were enrolled in the study if they were intubated from less than 48 h and were receiving sedation to facilitate their mechanical ventilation. Exclusion criteria were: age under 18 years, pregnancy, end stage renal disease (creatinine clearance <20 ml/min), severe hepatic failure (prothrombin time <50% and/or transaminase >10 U/dl and/or bilirubin >2 mg/dl), past medical history of seizure and/or convulsions, patient unarousable without sedation (RASS ≤−3 and/or GCS ≤ 7) and hemodynamic instability.
Study protocol
Once enrolled, each patient underwent sedation for a period of 6–12 h which was maintained through simultaneous infusion of propofol (Diprivan, Astrazeneca, Basiglio (MI), Italy) and remifentanil (Ultiva, GlaxoSmithkline, Verona, Italy), in order to minimize any influence of prior sedative agents (e.g., benzodiazepines) on the study, titrated to obtain a Ramsay score ≥4 and a RASS ≤−3. After this first period, each patient was awakened (stable RASS ≥0, Ramsay score ≤2, see above) to begin the actual study protocol, which included four phases, lasting 2 h each:
-
1.
ProRe1: 2 h of sedation achieved by propofol (1 mg/kg bolus + continuous infusion titrated to target sedation level) and remifentanil (≤0.2 mcg/kg/min continuous infusion).
-
2.
SevAn: 2 h of sedation by sevoflurane (Sevorane, Abbott, Campoverde di Aprilia (LT), Italy) administered through AnaConDa. After filling the line, the initial infusion rate was set relying on the nomogram provided by the manufacturer, which expresses the suggested initial infusion rate as a function of the minute ventilation, to obtain a 0.5% concentration of the agent. The rate was then adjusted in order to achieve the sedation target.
-
3.
ProRe2: Same as ProRe1.
-
4.
ProReFilter: Same as ProRe1, but a new (thus free of any sevoflurane) AnaConDa® was positioned on the respiratory circuit, without any administration of sevoflurane. This last step was performed to quantify the effect of the increased dead space caused by AnaConDa®.
In each phase the patients were sedated in order to achieve the aforementioned sedation targets. At the end of each step intravenous sedation was stopped or AnaConDa® device was removed from the respiratory circuit and patients were kept awake (stable RASS ≥0, Ramsay score ≤2) until the beginning of the following phase. At the beginning and at the end of each sedation phase we recorded the “time-to-action” and the “time-to-awake”, respectively.
All patients during each phase were ventilated in pressure-adjusted spontaneous mode with a Dräeger Evita 4 (Dräeger Medical, Lubeck, Germany). Suctioning was performed according to standard clinical practice by means of a closed suctioning system currently used in our institution (Ballard Trach-Care 72, Kimberly-Clark, Roswell, GA, USA). Patient’s hemodynamic stability was assured during the 6 h washout phase. Five patients were receiving vasopressors (Table 1). A maximum fluid challenge of 500 ml was allowed throughout the study, but these data have not been recorded.
Data collection
After 2 h from the achievement of the sedation target, in each phase the following parameters were recorded: tidal volume, respiratory rate, minute ventilation, inspiratory oxygen fraction, end tidal CO2, heart rate, invasive arterial blood pressure, central venous pressure, peripheral oxygen saturation, and internal body temperature, respiratory system compliance (C rs), airway resistance (R aw), according to standard formulas [12]. Intrinsic PEEP (PEEPi), was measured by means of a 5-second end expiratory occlusion. Moreover, we measured arterial blood gases and central venous oxygen saturation. In patients who had a pulmonary artery catheter in place we measured cardiac output by means of intermittent bolus thermodilution (three recordings were averaged), pulmonary artery occlusion pressure, and pulmonary artery pressure. Relevant hemodynamic and ventilatory variables were also recorded at the “time-of-action” of each sedation strategy.
Ambient contamination from sevoflurane
Environmental contamination from sevoflurane was measured by passive dosimeter sampling [13]. Three passive dosimeters (3 M gas monitors, Saint Paul, MN) were kept open during SevAn step, since it was the only one involving sevoflurane administration. One dosimeter was placed on the nurse directly caring for the patient (staff exposure), another within 20 cm from patient’s head (maximum contamination zone) and the last one was placed on the room wall, within 2–3 m from patient’s bed (general room contamination). At the end of the SevAn step the three monitors were sealed and later analyzed with gas chromatography at the Unit of Occupational Medicine, Desio Hospital, Desio (MI), Italy. Dosimeter measurements are often used to compare staff exposure to occupational exposure limits; however, as these limits have not been set for sevoflurane yet, we assumed, like other authors [14] did, that limits set (by the National Institute for Occupational Safety and Health, USA) for halogenated agents may be extended to sevoflurane (<2 ppm).
Statistical analysis
For each parameter we compared ProRe1 and SevAn phases to assess the effect of different sedation strategies and we compared ProRe1 and ProRe2 to confirm that patient’s conditions were stable throughout the study period. Finally, we compared SevAn and ProRefilter phases. Paired t-test and Wilcoxon signed rank test were used, respectively, for parametric and non-parametric data. Anova for repeated measures was used to compare the three sampling sites of environmental pollution. Linear regression was used to assess association between variables. A P value < 0.05 was considered statistically significant.
Results
Seventeen patients were enrolled; main characteristics are reported in Table 1.
Feasibility of SevAn sedation
The average dosages of propofol and remifentanil required to achieve the sedation targets were, respectively, 48 ± 29 and 0.14 ± 0.05 μg/kg/min during phase ProRe1 and, during phase ProRe2 40 ± 26 and 0.13 ± 0.05 μg/kg/min (P = n.s.). During the SevAn phase, sevoflurane was injected in the AnaConDa device at an average flow rate of 8.3 ± 2.7 ml/h, yielding inspiratory and expiratory concentrations of 1.06 ± 0.4 and 0.76 ± 0.31%, respectively. We did not disclose a statistically significant correlation between the infusion rate of propofol and either the injection rate or the end-tidal concentration of sevoflurane (data not shown).
During all the study phases we achieved similar levels of sedation, which were, in all cases, within the targets requested by the protocol (see Table 2). Despite the achievement of similar levels of sedation, the BIS score was lower in the SevAn phase than in the ProRe1.
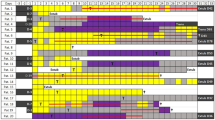
Achievement of sedation targets was significantly faster in the ProRe1 phase as opposed to SevAn. No differences were observed between the two ProRe phases. Analogously, the awakening of the patients was faster after discontinuation of ProRe than after the discontinuation of SevAn (Fig. 2).
Time required to achieve the sedation (Ramsay score ≥ 4, Richmond agitation sedation scale ≤ −3, filled bars) and awakening (Ramsay score ≤2, Richmond agitation sedation scale ≥0, empty bars) of the patients with the different strategies. ProRe 1 and ProRe 2 two phases of sedation achieved by propofol and remifentanil, SevAn sedation by sevoflurane administered trough AnaConDa * P < 0.05 versus ProRe1
Effects on cardiovascular system
At the end of the 2 h, the SevAn phase, in comparison with ProRe1 was associated with a statistically significant increase in the heart rate (Table 3), without significant variations either in arterial or central venous pressure. A similar trend was already present at the “time-of-action”, although it did not reach a statistical significance. Central venous oxygen saturation was higher during the SevAn phase, in comparison with ProRe1.
In the subgroup of patients with a pulmonary artery catheter in place (n = 9), we did not observe any statistically significant variation either in mean pulmonary arterial pressure, pulmonary artery occlusion pressure, or in cardiac output (Table 3). Central venous oxygen saturation was higher during the SevAn phase, in comparison with ProRe1.
None of the hemodynamic parameter showed a difference between ProRe1 and ProRe2.
Effects on respiratory system
Table 4 summarizes the main respiratory variables during the study phases. After 2 h of sedation with SevAn we observed a significant increase in both tidal volume and respiratory rate in comparison with ProRe1. As a consequence the minute ventilation increased, on average by 26 ± 15%. Despite this, PaCO2 increased as well during the SevAn phase, from 46.3 ± 7.9 to 49.4 ± 10.8 mmHg (P < 0.05); PaO2/FiO2 did not change between the different study phases. The differences in tidal volume, respiratory rate and minute ventilation, between the SevAn and ProRe1 phases were already present at the “time-of-action”.
In the attempt of separating the effects of the additional dead space, determined by the presence of the AnaConDa device, and that of the sedation type, we performed, in 12 patients, an additional study phase, with the SevAn device in place, while having the patients undergoing sedation with propofol and remifentanil. Despite similar levels of PaCO2 during the ProRefilter phase and the SevAn phase (48.6 ± 7.2, 49.2 ± 7.3 mmHg), minute ventilation was slightly lower (11.4 ± 2.6 vs. 13.6 ± 2.9 l/min), as a result of a marked reduction in respiratory rate (22.3 ± 5.3 vs. 29.2 ± 9.11 breaths per min, P < 0.05) and a mild increase in tidal volume (538 ± 66 vs. 492 ± 74 ml, P = 0.08).
Ambient contamination from sevoflurane
The concentration of sevoflurane in the ICU environment, averaged 0.36 ± 0.49, 0.32 ± 0.36 and 0.23 ± 0.29 ppm in the room, patient and nurse sampling sites, respectively (P = n.s. among the sites). In none of the seven assessments performed, the value exceeded the maximum level set by the National Institute for Occupational Safety and Health, USA (i.e., 2 ppm), being the two highest 0.61 and 0.99 ppm.
Discussion
The main findings of this work is that it is possible to sedate critically ill patients undergoing mechanical ventilation by administering sevoflurane by the AnaConDa, achieving levels of sedation similar to the ones obtained with propofol and remifentanil. While hemodynamic conditions were comparable among the two sedation strategies, relevant differences were found in respiratory parameters.
Not surprisingly, we did not disclose a correlation between intra-patient equipotent dosages of propofol and sevoflurane, as the drugs have different pharmacokinetic and pharmacodynamic properties.
In this study, we found that both the “time-to-action” and the “time-to-awake”, were longer with sevoflurane in comparison with propofol. Although our evaluation was limited to a short period of time and we did not assess long-term outcomes, such as time to extubation, our results might appear somehow contradictory with data in the literature, showing similar or shorter time to extubate the patient after general anesthesia with sevoflurane in comparison to propofol. Part of this discrepancy could be due to the fact that, while the patients undergoing general anesthesia have, on average, an intact respiratory function, our patients were likely to have abnormalities in regional ventilation/perfusion ratios, with shunting blood flow and/or alveolar dead space (as suggested by the arterial hypoxemia and by the high minute ventilation required to maintain normocapnia). Both these abnormalities can prolong the time required for the plasmatic concentration of a gas to equilibrate with the inspired one. Moreover, while the intravenous sedation begins with a bolus of propofol, in the initial phases of inhalational sedation the AnaConDa device did not contain any sevoflurane: this prolongs the time necessary for the inspired gas concentration to reach a stable value. In any case the values we recorded for “time-to-action” and the “time-to-awake” are absolutely compatible with the requirements of the clinical routine of the ICU.
In our study, we used a relatively short observation period (i.e., lasting 2 h): while this favors the presence of patient’s stable conditions throughout the study period, it is likely that if the study protocol had been prolonged for a longer period, sevoflurane might have offered advantages over propofol, given its low solubility and the low development of tachyphylaxis. Indeed, Sackey et al. [6] demonstrated shorter awaking times in critically ill patients after 96 h of sedation administering isoflurane with Anesthetic Conserving Device in comparison with intravenous sedation with benzodiazepines. Analogous results were recently described by Röhm and coworkers, comparing sevoflurane and propofol sedation in patients recovering from for elective coronary artery bypass graft, showing shorter awakening and extubation times, with the former approach [7].
The inhalational anesthesia provided with sevoflurane allowed maintaining hemodynamic conditions stable and comparable with those obtained with the combination of propofol and remifentanil, except for a higher heart rate in the former condition, probably as a consequence of the well known bradycardic effect of remifentanil. Moreover, tachycardia has been described as a consequence of sevoflurane administration, but at dosages higher than those employed in this study [15]. Another possible reason for tachycardia could be that during the SevAn phase some patients suffered from pain, as no specific analgesic drug was given. However, the purpose of remifentanil infusion in the ProRe phase, rather than providing analgesia, was to enhance the sedation induced by propofol, in order to use lower doses of this drug and minimize the hemodynamic effects. While propofol has no analgesic properties at all, we relied on the analgesic effect of sevoflurane [16] to obtain a similar level of analgesia. Central venous oxygen saturation was higher in the SevAn phase; as neither cardiac output nor arterial oxygenation did show significant variations, the sevoflurane might have depressed oxygen consumption of the patients more than propofol and remifentanil.
More relevant variations were seen with sevoflurane sedation in the ventilatory pattern, namely an increased PaCO2 accompanied by increased minute ventilation (mainly due to an increased respiratory rate). The increased PaCO2 is likely due to the additional anatomical dead space (approximately 100 ml) determined by the presence of the AnaConDa device, which is interposed between the circuit Y and the endotracheal tube, as suggested by the similar PaCO2 levels reached when AnaConDa was in place, independently of the sedation strategy employed (comparison of the SevAn, ProRefilter phases). It should be noted that we did not enroll severe ARDS patients: in such patients the use of the AnaConDa device might not be appropriate for two reasons: the additional dead space further impairs the elimination of CO2 and/or mandates an increase in tidal volume, which should be avoided in such patients [17]. The increased minute ventilation seen during the sedation period with sevoflurane is likely due both to the response to hypercapnia and to the absence of the powerful depressant effect of remifentanil on the respiratory centers; indeed, respiratory rate was lower in the ProRefilter in comparison with the SevAn phase. Finally, sevoflurane per se has been shown to increase respiratory rate [18].
The use of AnaConDa device appeared safe in terms of ICU environment pollution: the average environmental reading was well below the limit set by the National Institute for Occupational Safety and Health and in none of the samples we found levels above this threshold. It should be noted, however, that in our institution we use a closed suctioning system, which, avoiding frequent disconnections of the circuit probably aided in keeping the environmental pollution low. Caution should be used regarding a patient requiring frequent suctioning in the absence of a closed system.
In conclusion, this report shows that sevoflurane can be used to effectively and safely provide sedation in the ICU patients with stable hemodynamic conditions. These observation needs to be confirmed and expanded in a longer evaluation period.
References
Sessler CN, Varney K (2008) Patient-focused sedation and analgesia in the ICU. Chest 133:552–565
Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM, Crippen DW, Fuchs BD, Kelleher RM, Marik PE, Nasraway SA Jr, Murray MJ, Peruzzi WT, Lumb PD (2002) Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 30:119–141
Ostermann ME, Keenan SP, Seiferling RA, Sibbald WJ (2000) Sedation in the intensive care unit: a systematic review. JAMA 283:1451–1459
Ebert TJ (2006) Inhalation Anesthesia. In: Barash PG, Cullen BF, Stoelting RK (eds) Clinical anesthesia. Lippincott Williams & Wilkins, Philadelphia, pp 384–420
Patel SS, Goa KL (1996) Sevoflurane. A review of its pharmacodynamic and pharmacokinetic properties and its clinical use in general anaesthesia. Drugs 51:658–700
Sackey PV, Martling CR, Granath F, Radell PJ (2004) Prolonged isoflurane sedation of intensive care unit patients with the anesthetic conserving device. Crit Care Med 32:2241–2246
Rohm KD, Wolf MW, Schollhorn T, Schellhaass A, Boldt J, Piper SN (2008) Short-term sevoflurane sedation using the anaesthetic conserving device after cardiothoracic surgery. Intensive Care Med 34:1683–1689
Belda JF, Soro M, Badenes R, Meiser A, Garcia ML, Aguilar G, Marti FJ (2008) The predictive performance of a pharmacokinetic model for manually adjusted infusion of liquid sevofluorane for use with the anesthetic-conserving device (AnaConDa): a clinical study. Anesth Analg 106:1207–1214
Meyer JU, Kullik G, Wruck N, Kuck K, Manigel J (2008) Advanced technologies and devices for inhalational anesthetic drug dosing. Handb Exp Pharmacol 182:451–470
Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O’Neal PV, Keane KA, Tesoro EP, Elswick RK (2002) The Richmond agitation-sedation scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med 166:1338–1344
Singh H (1999) Bispectral index (BIS) monitoring during propofol-induced sedation and anaesthesia. Eur J Anaesthesiol 16:31–36
Rossi A, Polese G, Milic-Emili J (1998) Monitoring respiratory mechanics in ventilator-dependent patients. In: Tobin M (ed) Principles and practice of intensive care monitoring. McGraw Hill, New York, pp 553–596
Sackey PV, Martling CR, Nise G, Radell PJ (2005) Ambient isoflurane pollution and isoflurane consumption during intensive care unit sedation with the anesthetic conserving device. Crit Care Med 33:585–590
Accorsi A, Valenti S, Barbieri A, Raffi GB, Violante FS (2003) Proposal for single and mixture biological exposure limits for sevoflurane and nitrous oxide at low occupational exposure levels. Int Arch Occup Environ Health 76:129–136
Malan TP Jr, DiNardo JA, Isner RJ, Frink EJ Jr, Goldberg M, Fenster PE, Brown EA, Depa R, Hammond LC, Mata H (1995) Cardiovascular effects of sevoflurane compared with those of isoflurane in volunteers. Anesthesiology 83:918–928
Yeo ST, Holdcroft A, Yentis SM, Stewart A (2007) Analgesia with sevoflurane during labour: i. Determination of the optimum concentration. Br J Anaesth 98:105–109
Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The acute respiratory distress syndrome network (2000) N Engl J Med 342:1301–1308
Doi M, Ikeda K (1987) Respiratory effects of sevoflurane. Anesth Analg 66:241–244
Acknowledgments
This work was supported by a grant from Abbott S.pA. Campoverde (LT), Italy and by institutional funding. We thank G. Boffi, D. Sangiorgio and A. Arduca, Servizio di Prevenzione e Protezione, A.O. San Gerardo, Monza (MI), Italy for environmental readings.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Migliari, M., Bellani, G., Rona, R. et al. Short-term evaluation of sedation with sevoflurane administered by the anesthetic conserving device in critically ill patients. Intensive Care Med 35, 1240–1246 (2009). https://doi.org/10.1007/s00134-009-1414-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-009-1414-7