Abstract
The aim of this study was to evaluate procalcitonin as an adjunct to diagnose bacterial infections in older patients. One hundred seventy-two patients admitted to an acute-care geriatric unit during a 6-month period were prospectively included, 39 of them with an invasive bacterial infection. The best cut-off value to rule in a bacterial infection was 0.51 µg/l with sensitivity 64% and specificity 94%. The best cut-off value to rule out a bacterial infection was 0.08 µg/l with sensitivity 97% and specificity 20%. Procalcitonin was inconclusive (between 0.08 and 0.51 µg/l) for 112 admissions. Procalcitonin over 0.51 µg/l was useless 22 times out of 33 (infection already ruled in on clinical grounds) and misleading in eight of the 11 remaining cases (no infection). Procalcitonin below 0.08 µg/l was useless 23 times out of 27 (infection already ruled out on clinical grounds) and misleading in one of the four remaining cases (infection). Despite a good overall diagnostic accuracy, the clinical usefulness of PCT to diagnose invasive bacterial infections in elderly patients hospitalized in an acute geriatric ward appears to be very limited.
Similar content being viewed by others
Introduction
Reaching the diagnosis of bacterial infection is difficult in elderly patients. Medical history is often hard to get and unreliable due to sensory loss, cognitive impairment, and social isolation. Comorbidity interferes with physical examination, and cardinal features of infection like fever are often missing. Microbiological samples are difficult to collect, e.g. sputum samples, and may be false positives, e.g. urine samples. Due to age-related changes, imaging studies are not easy to interpret. Underdiagnosis of bacterial infections leads to therapeutic delay and worse outcomes. By contrast, overdiagnosis exposes patients with viral infection or non-infectious inflammatory processes to unnecessary and potentially harmful antibiotics, and increases bacterial resistance in institutions and geriatric units.
A specific and easy to get biological marker of infection would help improve antibiotics prescription in older patients. Inflammation markers, such as C-reactive protein (CRP) and procalcitonin (PCT), have been extensively studied in children and adults, but not in elderly subjects. Studies in this age group have shown a lack of accuracy when cut-off values determined in children and younger adults were used [1].
Our aims were (i) to evaluate the overall diagnostic accuracy of an ultra sensitive PCT assay for invasive bacterial infections in acutely hospitalized elderly patients, (ii) to find the best cut-off values to sort low- and high-probability patients, and (iii) to evaluate the added value of PCT over clinical history and routine biological and radiological studies.
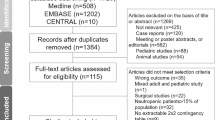
Patients and methods
Patients
All consecutive admissions in a single 14-bed acute-care geriatric unit were prospectively considered for inclusion from May 15, 2007. Patients had to be 75 years old or over to be admitted in the geriatric unit. The only exclusion criterion was antibiotic treatment for more than one day before admission, since PCT levels rapidly decrease following successful antibiotic therapy [2].
Data and biological assays
Clinical data were recorded at admission and blood tests were performed within 24 hours. The Charlson score was used to account for comorbidity [3]. Samples were collected on heparin lithium tubes for biochemical tests and EDTA for hematological tests (Becton Dickinson, Le Pont de Claix, France). PCT was measured in the blood sample drawn for other biochemical tests; no additional sample was drawn for this study. All biochemical tests except PCT were routinely performed with Architect ci8000 (Abbott Laboratories, Rungis, France), according to the manufacturers’ instructions. CRP assays were determined by an immuno-turbidimetric method. For CRP, the detection limit was 0.02 mg/l and the inter-assay coefficients of variation were 1.7% and 1.3% for values varying from 9.1 to 27 mg/l, respectively. PCT was assayed with an automated Kryptor analyzer at ultrasensitive level (B.R.A.H.M.S., Saint-Ouen, France) using TRACE technology [4]. The detection limit was 0.02 µg/l, and the inter-assay coefficients of variation were 6.0 and 5.5% for values ranging from 0.20 to 9.70 µg/l, respectively. PCT results were concealed until the end of the study enrollment, data collection and final diagnosis assessment.
Definitions
Systemic inflammatory response syndrome (SIRS) was diagnosed according to the American College of Chest Physicians/Society of Critical Care Medicine consensus classification if two or more of the following were found: body temperature >38°C (100.4°F) or <36°C (96.8°F), heart rate >90/min, respiratory frequency >20/min, and leukocyte count >12 G/l or <4 G/l [5].
At the end of their hospitalization and without knowledge of procalcitonin results, patients were classified as having suffered from an invasive bacterial infection at admission or not. For the sake of clinical relevance, non-invasive bacterial infections, such as cystitis or bronchitis, were counted as non-diseased. Pyelonephritis and prostatitis were defined as fever or systemic inflammatory response syndrome (SIRS) with urinary tract infections (WBC and bacterial CFU >105/ml) and either (i) blood cultures growing with the same pathogen, (ii) provoked loin or prostate pain, or (iii) no other obvious infection and fast clinical improvement under antibiotics. Pneumonia was defined as the association of fever or SIRS with at least one acute thoracic physical sign (dyspnea, cough, chest pain, purulent sputum, lung crackles) and a new radiographic pulmonary infiltrate on X-ray or CT-scan. Peritonitis was defined as fever or SIRS with acute abdominal pain (or tenderness) and guarding, and an underlying cause ascertained by radiological imaging or surgical intervention. Biliary infection was defined as fever or SIRS with acute abdominal pain or tenderness, and radiological features of cholecystitis or cholangitis (ultrasound or CT-scan). Intestinal infection was defined as fever or SIRS with acute abdominal pain and either growth of a bacterial pathogen (including C. difficile) in a stool sample or features of diverticulitis on CT-scan. Endocarditis was defined as fever or SIRS with positive blood-cultures and evidence of endocardial involvement on transthoracic echocardiography. Cellulitis was defined as fever or SIRS with acute redness and tenderness over a skin area.
Outcomes
The primary outcome was the area under the receiving operator characteristic (ROC) curve of PCT for the diagnosis of invasive bacterial infection. Secondary outcomes were the comparisons between the area under the ROC curve of PCT and CRP, and the diagnostic accuracy of these variables. Since it was unlikely for a single cut-off value to perfectly distinguish between the presence and the absence of invasive bacterial infection, we chose to define two cut-off values for each PCT and CRP: a sensitive cut-off to rule out an invasive bacterial infection and a specific cut-off to rule it in. When a result is in the “gray zone” between these two cut-off values, it does not impact significantly the probability of invasive bacterial infection [6]. The number of patients in the gray zone was also considered among secondary outcomes, because the more patients there are, the less useful the diagnostic test is.
While making these primary analyses, it appeared that even when PCT or CRP levels were outside the gray zone, they were of little added value if the diagnosis of invasive bacterial infection was already obviously ruled in or ruled out on clinical grounds. Patients with levels of PCT or CRP below the sensitive cut-off who were obviously not suffering from an invasive bacterial infection were post hoc identified and counted. Similarly, patients with levels of PCT or CRP over the specific cut-off who were obviously suffering from an invasive bacterial infection were post hoc identified and counted. After review of their charts, patients were independently classified by two physicians as obviously infected, obviously non-infected or neither one. Disagreements were solved by consensus.
Statistical methods
Sample size computation was performed in order to achieve a standard error less than 0.05 for the area under the PCT ROC curve for the diagnosis of invasive bacterial infection, as proposed by Hanley and McNeil [7]. For this computation, the area was expected to be about 0.70 [1] and the first 40 admissions were used to evaluate the prevalence of invasive bacterial infection in the study population.
Descriptive statistics are reported as median (interquartile range) or number (percentage), as appropriate, and differences were evaluated by the Mann-Whitney and the Chi-square tests, respectively. Area under the ROC curve for the diagnosis of invasive bacterial infection were computed for PCT and CRP and compared as proposed by Hanley and McNeil [8].
Sensitivity, specificity, positive and negative likelihood ratios, and diagnostic odds ratios were computed for the chosen cut-off values. The sensitive cut-off was defined in order to rule out an invasive bacterial infection, as the highest value for which the negative likelihood ratio was less than 0.1 or, if this first criterion could not be satisfied, for which the sensitivity was over 95%. The specific cut-off was defined as the lowest value for which the positive likelihood ratio was over ten or, if this first criterion could not be satisfied, for which the specificity was over 95%. The specificities of PCT and CRP were compared at the sensitive cut-off values and their sensitivities at the specific cut-off values with the exact McNemar test for paired proportions. All statistical analyses were done with Stata 8.2 (StataCorp, Texas, USA).
Results
Admissions features
The prevalence of invasive bacterial infection among the first 40 admissions was 25%. Accordingly, a total number of 168 admissions were needed to ensure a standard error less than 0.05 for the area under the PCT ROC curve for the diagnosis of invasive bacterial infection, assuming an area of at least 0.70. Recruitment lasted from May 15, 2007 to November 16, 2007 in order to achieve the required sample size. No viral epidemic (influenza, rotavirus, etc.) occurred during this time period.
There were 195 admissions during the enrollment period but 23 of them were excluded because of antibiotics use for more than 24 hours. Features of the 172 admissions are reported in Table 1. Eight patients were admitted twice during the study period. Thirty-nine admissions (23%) were related to an invasive bacterial infection: 19 (46%) pneumonia, 13 (33%) pyelonephritis or prostatitis, three cellulitis (8%), one diverticulitis (3%), one cholecystitis (3%), one angiocholitis (3%), one endocarditis (3%), and one peritonitis without etiological diagnosis (3%). The main other reasons for admission were: 25 falls (14%), 16 left ventricular failures (9%), 16 cancer complications (9%) and nine strokes (5%). No etiological diagnosis was reached for two patients admitted for acute fever that resolved quickly without antibiotics. These patients were classified in the group without invasive bacterial infection. Twenty-four hospitalizations (14%) ended with the death of the patient.
Diagnostic accuracy
ROC curves of PCT and CRP for the diagnosis of bacterial infection are displayed in Fig. 1. The areas under the ROC curve were 0.85 (95% confidence interval 0.77–0.92) for PCT and 0.84 (0.77–0.91) for CRP. These areas did not differ significantly (p = 0.89).
The best cut-off values to exclude bacterial infection were 0.08 µg/l for PCT and 10 mg/l for CRP (Table 2). By construction, PCT and CRP had similar sensitivities for these cut-off values and the specificity of CRP was not significantly better (p = 0.09).
The best cut-off values to affirm bacterial infection were 0.51 µg/l for PCT and 175 mg/l for CRP (Table 2). By construction, PCT and CRP had similar specificities for these cut-off values, but the sensitivity of PCT was significantly better (p = 0.006).
Diagnostic gain
The number of patients in the gray zone was 112 (65%) for PCT, whereas 27 (16%) patients were below the sensitive cut-off (0.08 µg/l) and 33 (19%) above the specific cut-off (0.51 µg/l). PCT below 0.08 µg/l was useless 23 out of 27 times (infection already ruled out on clinical grounds) and misleading in one of the four remaining cases (invasive infection: pyelonephritis). Likewise, PCT over 0.51 µg/l was useless 22 out of 33 times (infection already ruled in on clinical grounds) and misleading in eight of the 11 remaining cases (no invasive infection: four traumas, three cancers, and one self-resolving fever). Overall, PCT was uninformative (gray zone or clinical examination already conclusive) for 157/172 (91%) patients and misleading in nine (60%) of the 15 remaining.
For CRP, the number of patients in the gray zone was 112 (65%), whereas 40 (23%) patients were below the sensitive cut-off (10 mg/l) and 20 (12%) above the specific cut-off (175 mg/l). CRP below 10 mg/l was useless 36 out of 40 times (infection already ruled out on clinical grounds) and misleading in one of the four remaining cases (invasive infection: pneumonia). Likewise, CRP over 175 mg/l was useless 13 out of 20 times (infection already ruled in on clinical grounds) and misleading in five of the seven remaining cases (no invasive infection: three cancers, two traumas). Overall, CRP was uninformative (gray zone or clinical examination already conclusive) for 161/172 (94%) patients and misleading in six (55%) of the 11 remaining.
Discussion
Principal findings
In this study, PCT had a high overall accuracy for the diagnosis of invasive bacterial sepsis. However, when PCT was sufficiently high or low to be conclusive, infection could often be ruled in or out on clinical grounds alone. In a significant proportion of the remaining cases, procalcitonin results were misleading.
Strengths and weaknesses of the study
There were no other exclusion criteria than previous antibiotic treatment for more than 24 hours. The study population is therefore representative of the everyday recruitment of a geriatric unit. However, internal validity is hindered by some methodological limitations. First, there is no gold standard for the diagnosis of invasive bacterial infection and the definition of each type of invasive bacterial infection is controversial [9]. Nonetheless, initial and follow-up findings allow a robust diagnosis in most cases. Second, the classification of patients as obviously infected or obviously non-infected at their admission was done retrospectively. We tried to minimize the risk of bias by making two clinicians independently look at the files to classify patients and then resolve their disagreements by consensus.
Comparison with previous studies
PCT is a marker of severe bacterial but not viral infections [10]. Localized and non-severe bacterial infections fail to induce important increases of PCT levels [11, 12]. Since PCT assays are not standardized, it is difficult to compare results from different studies. Two tests have been extensively assessed: the LUMItest and the more recent Kryptor assay. We used the latter, which belongs to the ultrasensitive assays [13].
Only three studies assessed the diagnostic value of PCT in older patients (Table 3). All these studies assessed a cut-off level of 0.5 µg/l but none used an ultrasensitive assay as we did. Two of these studies included patients hospitalized in geriatric wards [1, 14]. The first one found a similar specificity of PCT (94%) in patients with no bacterial infection but sensitivity was much lower (24%) [1]. This lower sensitivity may be due to the assay that was used, since the proportion, site and severity of infections were very close to those found in our study. The second study found a similar sensitivity of PCT (63%) in patients hospitalized for acute bacterial infections, but specificity was not reported [14]. The last study was done in an emergency department and assessed the accuracy of PCT to distinguish bacteremic from non-infected patients over 65 years old in whom blood culture were ordered [15]. Despite these major design differences with our work, the reported sensitivity and specificity were quite close. Overall, the authors of these three studies are very cautious and warn against reliance on PCT results to establish or exclude invasive bacterial infections in older patients.
We found two other studies assessing the diagnostic value of PCT for bacterial infections in hospitalized adults outside intensive care units, including some elderly patients [16, 17]. The first one was done in an internal medicine department in patients with fever or biological inflammation [16]. Mean age of the patients was 68 years and a LUMItest assay was assessed with a 0.5 µg/l cut-off to distinguish bacterial infections from non-infectious inflammatory processes. The reported sensitivity and specificity were 65 and 96%, respectively, which was very close to our findings. The second study was done in younger patients (mean age 62 years) hospitalized in an infectious diseases department [17]. A LUMItest assay was used with a 0.1 µg/l cut-off to diagnose bacterial infection in febrile patients. The sensitivity of PCT in patients with documented bacterial infections was only 54% and the specificity in non-infected patients was 70%. Why PCT performed so poorly in this study is not clear. However, this is in keeping with a limited clinical usefulness of this test in patients hospitalized outside intensive care units.
Conclusion
Despite a good overall accuracy, when PCT was sufficiently high or low to be conclusive, infection could often be ruled in or out on clinical grounds alone. In a significant proportion of the remaining cases, PCT results were misleading. The clinical usefulness of PCT to diagnose invasive bacterial infections in elderly patients hospitalized in an acute geriatric ward appears to be very limited.
References
Stucker F, Herrmann F, Graf JD, Michel JP, Krause KH, Gavazzi G (2005) Procalcitonin and infection in elderly patients. J Am Geriatr Soc 53:1392–1395
Briel M, Schuetz P, Mueller B, Schild U, Nusbaumer C, Périat P, Bucher HC, Christ-Crain M (2008) Procalcitonin-guided antibiotic use vs a standard approach for acute respiratory tract infections in primary care. Arch Intern Med 168:2000–2007
Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47:1245–1251
Hubl W, Krassler J, Zingler C, Pertschy A, Hentschel J, Gerhards-Reich C, Mack M, Demant T (2003) Evaluation of a fully automated procalcitonin chemiluminescence immunoassay. Clin Lab 49:319–327
The ACCP/SCCM American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20:864–874
Coste J, Pouchot J (2003) A grey zone for quantitative diagnostic and screening tests. Int J Epidemiol 32:304–313
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143:29–36
Hanley JA, McNeil BJ (1983) A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 148:839–843
Christ-Crain M, Müller B (2006) Procalcitonin: you only find what you look for, and you only look for what you know. J Am Geriatr Soc 54:546
Mitaka C (2005) Clinical laboratory differentiation of infectious versus non-infectious systemic inflammatory response syndrome. Clin Chim Acta 351:17–29
Rothenburger M, Markewitz A, Lenz T, Kaulbach HG, Marohl K, Kuhlmann WD, Weinhold C (1999) Detection of acute phase response and infection. The role of procalcitonin and C-reactive protein. Clin Chem Lab Med 37:275–279
Giamarellos-Bourboulis EJ, Mega A, Grecka P, Scarpa N, Koratzanis G, Thomopoulos G, Giamarellou H (2002) Procalcitonin: a marker to clearly differentiate systemic inflammatory response syndrome and sepsis in the critically ill patient? Intensive Care Med 28:1351–1356
Steinbach G, Rau B, Debard AL, Javourez JF, Bienvenu J, Ponzio A, Bonfà A, Hubl W, Demant T, Külpmann WR, Buchholz J, Schumann G (2004) Multicenter evaluation of a new immunoassay for procalcitonin measurement on the Kryptor System. Clin Chem Lab Med 42:440–449
Dwolatzky T, Olshtain-Pops K, Yinnon AM, Raveh D, Rogowski O, Shapira I, Rotstein R, Berliner S, Rudensky B (2005) Procalcitonin in the elderly: normal plasma concentrations and response to bacterial infections. Eur J Clin Microbiol Infect Dis 24:763–765
Caterino JM, Scheatzle MD, Forbes ML, D'Antonio JA (2004) Bacteremic elder emergency department patients: procalcitonin and white count. Acad Emerg Med 11:393–396
Delèvaux I, André M, Colombier M, Albuisson E, Meylheuc F, Bègue RJ, Piette JC, Aumaître O (2003) Can procalcitonin measurement help in differentiating between bacterial infection and other kinds of inflammatory processes? Ann Rheum Dis 62:337–340
Muñoz P, Simarro N, Rivera M, Alonso R, Alcalá L, Bouza E (2004) Evaluation of procalcitonin as a marker of infection in a nonselected sample of febrile hospitalized patients. Diagn Microbiol Infect Dis 49:237–241
Author information
Authors and Affiliations
Corresponding author
Additional information
Both Olivier Steichen and Eric Bouvard contributed equally to this work.
Rights and permissions
About this article
Cite this article
Steichen, O., Bouvard, E., Grateau, G. et al. Diagnostic value of procalcitonin in acutely hospitalized elderly patients. Eur J Clin Microbiol Infect Dis 28, 1471–1476 (2009). https://doi.org/10.1007/s10096-009-0807-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-009-0807-4