Abstract
The feasibility of using mobile health applications to conduct observational clinical studies requires rigorous validation. Here, we report initial findings from the Asthma Mobile Health Study, a research study, including recruitment, consent, and enrollment, conducted entirely remotely by smartphone. We achieved secure bidirectional data flow between investigators and 7,593 participants from across the United States, including many with severe asthma. Our platform enabled prospective collection of longitudinal, multidimensional data (e.g., surveys, devices, geolocation, and air quality) in a subset of users over the 6-month study period. Consistent trending and correlation of interrelated variables support the quality of data obtained via this method. We detected increased reporting of asthma symptoms in regions affected by heat, pollen, and wildfires. Potential challenges with this technology include selection bias, low retention rates, reporting bias, and data security. These issues require attention to realize the full potential of mobile platforms in research and patient care.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Topol, E.J., Steinhubl, S.R. & Torkamani, A. Digital medical tools and sensors. J. Am. Med. Assoc. 313, 353–354 (2015).
Ritter, S. Apple's research kit development framework for iPhone apps enables innovative approaches to medical research data collection. J. Clin. Trials 5, 2–3 (2015).
Jardine, J., Fisher, J. & Carrick, B. Apple's ResearchKit: smart data collection for the smartphone era? J. R. Soc. Med. 108, 294–296 (2015).
Morgan, A., Mooney, S., Aronow, B. & Brenner, S. Precision Medicine: Data and Discovery for Improved Health and Therapy”. Pacific Symposium on Biocomputing. Accessed May 7, 2016. http://psb.stanford.edu/psb-online/proceedings/psb16/intro-pm.pdf (2016).
Savage, N. Mobile data: Made to measure. Nature 527, S12–S13 (2015).
Akinbami, O.J., Moorman, J.E. & Liu, X. Asthma prevalence, health care use, and mortality: United States, 2005–2009. (US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics Washington, DC, 2011).
Dorsey, E.R. et al. The use of smartphones for health research. Acad. Med. 92, 157–160 (2017).
Menne, M.J. et al. Global historical climatology network-daily (GHCN-Daily), Version 3. (NOAA National Climatic Data Center, 2012).
Gul, R.B. & Ali, P.A. Clinical trials: the challenge of recruitment and retention of participants. J. Clin. Nurs. 19, 227–233 (2010).
Lovato, L.C., Hill, K., Hertert, S., Hunninghake, D.B. & Probstfield, J.L. Recruitment for controlled clinical trials: literature summary and annotated bibliography. Control. Clin. Trials 18, 328–352 (1997).
Lovejoy, B. ResearchKit did in 24 hours what would normally take 50 medical centers a year—Stanford University. 9to5 Mac. Accessed Aug 15, 2016. https://9to5mac.com/2015/03/12/researchkit-usage/ (2015).
Smith, A. US Smartphone use in 2015. Accessed September 5 2016: http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/ (Pew Research Center, 2015).
Arora, S. et al. Describing the evolution of mobile technology usage for Latino patients and comparing findings to national mHealth estimates. J. Am. Med. Inform. Assoc. 23, 979–983 (2016).
Wei, J., Hollin, I. & Kachnowski, S. A review of the use of mobile phone text messaging in clinical and healthy behaviour interventions. J. Telemed. Telecare 17, 41–48 (2011).
Dolan, B. How mobiles make clinical trials bigger, faster and more efficient. Mobile Health News. Accessed June 11, 2016. http://www.mobihealthnews.com/28198/how-mobiles-make-clinical-trials-bigger-faster-and-more-efficient (2013).
Miseta, E. Mobile devices in clinical trials: tested, effective, proven!. Clinical Leader. Accessed on May 5, 2016. https://www.clinicalleader.com/doc/mobile-devices-in-clinical-trials-tested-effective-proven-0002 (2016).
Henderson, L. Cell phone key to REMOTE data collection. Applied Clinical Trials. Accessed on May 3, 2016. http://www.appliedclinicaltrialsonline.com/cell-phone-key-remote-data-collection (2011).
Coons, S.J. et al. Capturing patient-reported outcome (PRO) data electronically: the past, present, and promise of ePRO measurement in clinical trials. Patient 8, 301–309 (2015).
Podsakoff, P.M. & Organ, D.W. Self-reports in organizational research: problems and perspectives. J. Manage. 12, 531–544 (1986).
Murphy, K.R. et al. Asthma management and control in the United States: results of the 2009 asthma insight and management survey. Allergy Asthma Proc. 33, 54–64 (2012).
Halpern, S.D., Karlawish, J.H., Casarett, D., Berlin, J.A. & Asch, D.A. Empirical assessment of whether moderate payments are undue or unjust inducements for participation in clinical trials. Arch. Intern. Med. 164, 801–803 (2004).
Russell, M.L., Moralejo, D.G. & Burgess, E.D. Paying research subjects: participants' perspectives. J. Med. Ethics 26, 126–130 (2000).
King, D., Greaves, F., Exeter, C. & Darzi, A. 'Gamification': influencing health behaviours with games. J. R. Soc. Med. 106, 76–78 (2013).
Miller, A.S., Cafazzo, J.A. & Seto, E. A game plan: Gamification design principles in mHealth applications for chronic disease management. Health Informatics J. 22, 184–193 (2016).
Centers for Disease Control and Prevention. Behavioral risk factor surveillance system: summary data quality report. Accessed Aug. 14, 2016. https://www.cdc.gov/brfss/annual_data/2013/pdf/2013_dqr.pdf (CDC, 2013).
Alkhaldi, G. et al. The effectiveness of technology-based strategies to promote engagement with digital interventions: a systematic review protocol. JMIR Res. Protoc. 4, e47 (2015).
Wantland, D.J., Portillo, C.J., Holzemer, W.L., Slaughter, R. & McGhee, E.M. The effectiveness of Web-based vs. non-Web-based interventions: a meta-analysis of behavioral change outcomes. J. Med. Internet Res. 6, e40 (2004).
Ryan, D. et al. Clinical and cost effectiveness of mobile phone supported self monitoring of asthma: multicentre randomised controlled trial. Br. Med. J. 344, e1756 (2012).
Bloss, C.S. et al. A prospective randomized trial examining health care utilization in individuals using multiple smartphone-enabled biosensors. PeerJ 4, e1554 (2016).
D'Arcy, S. et al. A method to assess adherence in inhaler use through analysis of acoustic recordings of inhaler events. PLoS ONE 9, e98701 (2014).
Su, J.G. et al. Feasibility of deploying inhaler sensors to identify the impacts of environmental triggers and built environment factors on asthma short-acting bronchodilator use. Environ. Health Perspect. 125, 254–261 (2017).
Hai, A. et al. Adherence monitoring and E-health: how clinicians and researchers can use technology to promote inhaler adherence for asthma. J. Allergy Clin. Immunol. Pract. 1, 446–454 (2013).
van Boven, J.F., Trappenburg, J.C., van der Molen, T. & Chavannes, N.H. Towards tailored and targeted adherence assessment to optimise asthma management. NPJ Prim. Care Respir. Med. 25, 15046 (2015).
Howard, S., Lang, A., Patel, M., Sharples, S. & Shaw, D. Electronic monitoring of adherence to inhaled medication in asthma. Curr. Respir. Med. Rev. 10, 50–63 (2014).
Merchant, R.K., Inamdar, R. & Quade, R.C. Effectiveness of population health management using the propeller health asthma platform: a randomized clinical trial. J. Allergy Clin. Immunol. Pract. 4, 455–463 (2016).
Bot, B.M. et al. The mPower study, Parkinson disease mobile data collected using ResearchKit. Sci. Data 3, 160011 (2016).
Wilbanks, J. & Friend, S.H. First, design for data sharing. Nat. Biotechnol. 34, 377–379 (2016).
Trister, A.D., Dorsey, E.R. & Friend, S. Smartphones as New Tools in the Management and Understanding of Parkinson's Disease. 2016NJP-Parkinson's Disease. Accessed Aug 1 2016. http://www.nature.com/articles/npjparkd20166.
Acknowledgements
The study is funded by the Icahn School of Medicine at Mount Sinai, UL1TR001433-01, and with technology support from LifeMap Solutions.
Author information
Authors and Affiliations
Contributions
Y.-F.Y.C. developed the initial study design/protocol, including electronic informed consent and the statistical plan, IRB submission and approval, app design and implementation, and budget management, ensured proper study execution, provided clinical support, refined surveys, and assisted in data interpretation, manuscript writing and revision and preparation for submission. P.W. contributed to study design and survey refinement, led statistical support and provided oversight for all data analysis and interpretation, generated figures and tables, and was a major contributor to manuscript writing and revision. L.R. assisted in the initial study design/protocol and IRB preparation and submission, led in the design of surveys, provided clinical support, participated in manuscript writing, and served as NJH liaison. N.T. provided statistical support, including data analysis and interpretation, generated figures and tables, participated in study design and survey refinement, provided major contributions to manuscript writing and revision, and served as a graphic artist liaison. M.Z. assisted in electronic informed consent design, led subsequent IRB submission and provided support, refined surveys, and was a major contributor to manuscript writing and preparation for submission. S.G.H. served as LifeMap Solutions scientific lead and provided support for AHA design, implementation, and functionality, served as a liaison to other technology partners, refined surveys, and assisted in data interpretation and manuscript writing. N.G. led the latter part of the study execution, provided subsequent IRB support, provided clinical support, refined surveys, and assisted in data interpretation and manuscript writing. E.R.S. provided statistical support and data analysis and interpretation, assisted in generating figures and tables, provided subsequent IRB support, and participated in manuscript writing. S.V. was involved in study execution and manuscript writing. M.B. assisted in data analysis and interpretation, and generated figures and tables. E.K. contributed to app design and implementation, as well as initial IRB document preparation. R.E. was the LifeMap Solutions technical lead, participated in app design and implementation, and helped ensure data integrity. R.W. assisted in study design and data interpretation. C.A.P. contributed to study design and data interpretation. J.T.D. contributed to study design input and manuscript revision. E.E.S. participated in study design, oversaw study execution, interpreted data, and participated in manuscript writing and revision.
Corresponding authors
Ethics declarations
Competing interests
E.E.S. (a co-investigator in this study, Chair of the Department of Genetics and Genomics Sciences, and Director of the Icahn Institute for Genomics and Multiscale Biology) and J.T.D. (a co-Investigator in this study and the Director of Biomedical Informatics at the Icahn School of Medicine at Mount Sinai (ISMMS) both hold equity in the form of stock options in LifeMap Solutions, a privately held company. In addition E.E.S. serves as an uncompensated advisory board member and is administratively responsible for the medical school's collaboration with LifeMap Solutions.
Integrated supplementary information
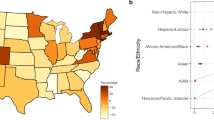
Supplementary Figure 1 Geographic distribution of asthma prevalence.
a) Based on location data from 4,612 Baseline users from 49 states, the log10 transformed percent distribution of asthma prevalence for asthma health app users is compared to 2013 national asthma prevalence statistics. SOURCE: 2013 Behavioral Risk Factor Surveillance System (BRFSS) http://www.cdc.gov/asthma/brfss/2013/tableC1.htm, Downloaded on 1/19/16. (b) The heatmap illustrates 37 features derived from the median of the maximum daily temperature over 5-day intervals for 3,646 user-linked zip codes (see Online Methods for details of the clustering method). (c) Northern (blue) and southern (red) regions of Contiguous US as determined by clustering of maximum median temperature (see methods). Figure shows the overlay of the county map on top of the state map, where color coding (North, blue and South, red) is based, in each case, on majority rule of user location clustering assignment.
Supplementary Figure 2 Retention analysis: correlations among covariates and the distribution of response rates.
Both (a) and (b) are based on n=537 Robust users who enrolled between March 9 2015 and June 8 2015. (a) Heatmap of the Pearson’s correlation matrix of the predictors for retention time in the Cox Proportional Hazards model. Lower diagonal cells in (a) represent the Pearson’s correlation coefficients; the upper diagonal cells indicate the p-values for testing zero correlation. (b) Histogram of individual response rates of daily surveys.
Supplementary Figure 3 Heat maps of daily survey response by baseline GINA control category.
Heatmaps of self-reported day symptoms, night symptoms, and quick relief inhaler usage were plotted for participants (y-axis) stratified by baseline GINA classification across 180 days of study enrollment (x-axis). Only participants enrolled for at least 180 days by 9/9/2015 were plotted. Participants were sorted according to the number of non-missing responses for each plot. Responses to these questions were: True (red), False (yellow), or missing (black).
Supplementary Figure 4 Concordance within time-series.
Pair-wise comparisons of correlation based on self-reported peakflow, day symptoms, night symptoms, and number of quick relief puffs. Each plot shows a histogram of correlation coefficients evaluated for each user based on his or her daily survey response time series. Total number of Robust users, average number of surveys per Robust user, and summary statistics for each comparison are shown in the lower diagonal.
Supplementary Figure 5 Distributions of self-reported asthma triggers at the start of enrollment and throughout the study period.
Based on data from 545 Robust users, barplots (left) show trigger distributions ordered by percentage rank of each asthma trigger for northern (top) and southern regions (bottom). Trigger distribution curves (right) are based on daily asthma trigger reports for robust users ordered by percentage rank at the start of enrollment for northern (top) and southern (bottom) regions respectively (see online Methods).
Supplementary Figure 6 iPhone versus Android users.
(a) Potential Asthma Health app audience by iPhone, Android and other smart devices. (b) Targeted demographics for the Asthma Health app.
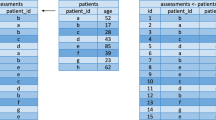
Supplementary Figure 7 A simplified layout of the initialization, the data flow and security measures in the Asthma Mobile Health Application study.
(a) The initialization process in the Asthma Mobile Health Application study. (b) The data flow and security measures in the Asthma Mobile Health Application study.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–7, Supplementary Tables 1–6 and Supplementary Note (PDF 1456 kb)
Supplementary Software
Code used in this study. (ZIP 3158 kb)
Rights and permissions
About this article
Cite this article
Chan, YF., Wang, P., Rogers, L. et al. The Asthma Mobile Health Study, a large-scale clinical observational study using ResearchKit. Nat Biotechnol 35, 354–362 (2017). https://doi.org/10.1038/nbt.3826
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nbt.3826
This article is cited by
-
Precise management system for chronic intractable pain patients implanted with spinal cord stimulation based on a remote programming platform: study protocol for a randomized controlled trial (PreMaSy study)
Trials (2023)
-
Home monitoring with connected mobile devices for asthma attack prediction with machine learning
Scientific Data (2023)
-
Mobile health applications for health-care delivery: trends, opportunities, and challenges
Journal of Public Health (2023)
-
A systematic review of smartphone applications for cancer survivors
Journal of Cancer Survivorship (2023)
-
A Real-World Effectiveness Study Using a Mobile Application to Evaluate Early Outcomes with Upadacitinib in Rheumatoid Arthritis
Rheumatology and Therapy (2023)