Abstract
Study design:
Systematic review
Objectives:
To determine the effect of respiratory muscle training (RMT) on pulmonary function in tetraplegia.
Methods:
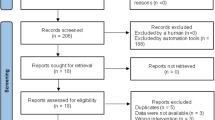
A comprehensive search of the research literature included MEDLINE, EMBASE, CINAHL, ISI Web of Science, PubMed, the relevant Cochrane and clinical trials registers and hand-searching the reference lists of appropriate papers. There was no language restriction. All randomised controlled trials that involved RMT vs control were considered for inclusion. Two reviewers independently selected articles for inclusion, evaluated the methodological quality and extracted data. Additional information was sought from the authors when necessary.
Results:
Eleven studies (212 participants) were included. A significant benefit of RMT was revealed for five outcomes: vital capacity (mean difference (95% confidence interval))=0.41(0.17–0.64) l, maximal inspiratory pressure=10.66(3.59, 17.72) cmH2O, maximal expiratory pressure=10.31(2.80–17.82) cmH2O, maximum voluntary ventilation=17.51(5.20, 29.81) l min−1 and inspiratory capacity=0.35(0.05, 0.65) l. No effect was found for total lung capacity, peak expiratory flow rate, functional residual capacity, residual volume, expiratory reserve volume or forced expiratory volume in 1 second.
Conclusion:
RMT increases respiratory strength, function and endurance during the period of training. Further research is needed to determine optimum dosages and duration of effect. This article is based in part on a Cochrane review published in the Cochrane Database of Systematic Reviews (CDSR) 2013, DOI:10.1002/14651858.CD008507.pub2. Cochrane reviews are regularly updated as new evidence emerges and in response to feedback, and the CDSR should be consulted for the most recent version of the review.
Similar content being viewed by others
Introduction
Respiratory dysfunction remains a significant cause of illness and death for people with tetraplegia.1 Recent research indicates that in the 5 years following acute spinal cord injury (SCI), pulmonary function declines at a rate that exceeds the normal age-related decline.2 Injury to the spinal cord impairs neuronal control of the respiratory muscles, leading to high incidence of respiratory complications, in particular pulmonary secretion retention, atelectasis, pneumonia and respiratory failure.3 Both inspiration and expiration are compromised in tetraplegia. Impaired inspiratory muscle function prevents deep breaths, reduces vital capacity and may lead to atelectasis and/or dyspnoea with exertion.3 Impaired expiratory muscle function impairs cough and secretion clearance and increases the incidence of lower respiratory tract infections.4 As such, respiratory dysfunction secondary to muscle weakness considerably affects the health and health-related quality of life for people with SCI.
The respiratory muscles can be trained in a similar way to the limb muscles by using tasks that increase the load on the muscles.5 Various types of respiratory muscle training (RMT) to improve respiratory strength and endurance have been described for people with tetraplegia. These include the use of both resistive and threshold trainers, which typically involve a one-way valve system that selectively trains either the inspiratory or the expiratory muscles. Normocapnic hyperpnoea6, 7 and singing training8 have also been reported as effective forms of RMT that simultaneously involve the inspiratory and expiratory muscles. Typical training sessions consist of a certain number of exercise repetitions or a particular length of time spent exercising.
Previous attempts at systematically reviewing the research to evaluate the effect of RMT in patients with SCI9, 10, 11 have reported that heterogeneity, in terms of research design, participant characteristics, training techniques used and outcomes measured, has prohibited meta-analysis. We recently published a Cochrane review (including meta-analysis) of RMT in cervical SCI.12 As per the focus of the Cochrane collaborative, the outcomes in that review were selected from a consumer poll of outcomes that were considered meaningful from the perspective of this population. These ‘Cochrane’ outcomes were the frequency of respiratory complications, dyspnoea, vital capacity (VC), maximal inspiratory and expiratory pressures (MIP and MEP), forced expiratory volume in one second (FEV1) and quality of life. This current systematic review and meta-analysis complements those results but specifically addresses the full range of pulmonary function outcomes that have been reported in the literature.
Materials and methods
A comprehensive search of the research literature before March 2013 included electronic databases (MEDLINE, EMBASE, CINAHL, ISI Web of Science, PubMed), the relevant Cochrane and clinical trials registers and hand-searching of the reference lists of relevant papers and literature reviews. We used the following keywords in the search: (1) SCI, tetraplegia and synonyms, and (2) RMT and synonyms (the full Medline search strategy is presented in Appendix 1). There was no language restriction. Inclusion criteria were as follows: (1) participants with any level of acquired cervical SCI, both acute and chronic; (2) an intervention described as RMT; (3) randomised controlled trial design (that is, a randomised comparison group using an alternative intervention, placebo, usual care or no intervention). Studies of RMT for people with inherited or congenital neuromuscular disorders (such as muscular dystrophies, congenital and acquired myopathies and spinal muscular atrophy) or respiratory disorders not caused by spinal injury (such as COPD and asthma) were excluded.
Static lung and spirometric measures analysed for this review included total lung capacity (TLC), forced vital capacity (FVC), VC, functional residual capacity (FRC), residual volume (RV), expiratory reserve volume (ERV), FEV1, FEV1 as a proportion of FVC (FEV1/FVC), inspiratory capacity (IC) and peak expiratory flow rate (PEFR). Measures of respiratory muscle strength (MIP and MEP) and of the maximum voluntary ventilation (MVV) were also extracted.
Two reviewers independently selected articles for inclusion, evaluated the methodological quality and extracted data. Disagreement between reviewers was resolved through discussion, and additional information was sought from trial authors when necessary. Revman (Version 5.2) software was used to analyse the results. Results are presented as mean differences (using post-test scores) and 95% confidence intervals.
The papers were screened and the raw data extracted at the same time as the Cochrane paper. We explicitly performed the Cochrane analyses first, addressing only the selected variables and hypotheses that were to be included in the Cochrane review. Following the acceptance of the Cochrane paper, we performed the analysis on the ‘extended’ outcomes as described in this paper and reached the conclusions as described.
Results
A total of 843 citations were identified from the sources above. After removing duplicates and animal studies, the titles and abstracts of 747 citations were reviewed and the full text for 40 publications retrieved. Of these, 28 were excluded on the basis of design (not randomised, n=26), ineligible populations (n=3) or ineligible intervention (not RMT, n=4). A full list of these excluded studies can be found in the Cochrane review.12
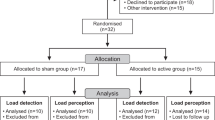
Eleven studies (12 publications) with a total of 212 participants met all the inclusion criteria and were included in the review (Table 1). One study13 had a cross-over design, and in the remaining 10 studies there were four comparisons between RMT and an alternative intervention,6, 8, 14, 15 and seven comparisons against a control condition (three vs a sham treatment6, 7, 16 and four vs 'usual care').17, 18, 19, 20 Sample sizes for the included studies ranged from 9 to 40 participants, and injury level ranged from C4 to C8. Some studies included participants with thoracic-level injuries7, 16 and nontraumatic SCI.15, 19 Testing position was not consistent across the studies. Six studies tested participants in a seated position,6, 7, 8, 15, 16, 19 whereas two studies used a supine testing position.14, 18 Two studies tested in both positions13, 17 and one study did not report the testing position.20 Wearing an abdominal binder during respiratory function testing has been reported to deliver better results for people with tetraplegia, in a similar manner to testing in the supine position.21 Only two of the six studies that used an upright sitting position for testing stated that an abdominal binder was not used.6, 8 A minority of studies demonstrated strong methodological rigor, with few adequately reporting allocation concealment7, 8 and blinding procedures.6, 7, 8, 16 In addition, six studies failed to report outcome data for participants who did not complete the trial.6, 14, 15, 16, 18, 19
Two of the included studies6, 15 compared two different RMT interventions with a control condition. To facilitate clear comparison of interventions in the meta-analysis, the Mueller6 inspiratory resistance training comparison (vs control) is referred to as Mueller 2013 (A) and the isocapnic hyperpnoea comparison as Mueller 2013 (B). Similarly, the Litchke15 flow resistance training comparison is termed Litchke 2010 (A) and the pressure threshold resistance training as Litchke 2010 (B). Eight studies used resistive muscle training devices targeting either inspiratory (n=5)6, 13, 14, 18, 20 or expiratory (n=3)13, 16, 17 muscle resistance. Five studies simultaneously targeted both inspiratory and expiratory muscle function.6, 7, 8, 15, 19 The different interventions ranged in intensity from 10 to 60 min per day, 3 to 7 days per week, and total length of training ranged from 4 to 12 weeks (mean 8 weeks).
Two studies13, 20 presented data as percentages of predicted normal values rather than raw scores, and thus these data could not be pooled with the other studies for meta-analysis. As there were no common outcomes between these two studies, a comparison of the percentage of predicted scores was not possible. We contacted the authors of these studies, but were not able to obtain any raw data. The majority of included studies did not report change score standard deviations. Thus, we conducted the meta-analysis using mean post-test scores, assuming that any baseline differences between groups would be accounted for through random group allocation. Table 2 presents a summary of the results of the meta-analysis for the pulmonary function variables.
Analyses revealed that RMT statistically significantly improved MIP (mean difference (95% confidence interval))=10.66 (3.59, 17.72) cmH2O, MEP=10.31 (2.80, 17.82) cmH2O, MVV=17.51 (5.20, 29.81) l min−1 (Figure 1) and IC 0.35 (0.05, 0.65) l (Figure 2). No significant effect was found for FEV1, TLC, FRC, RV, ERV, PEFR rate or FEV1/FVC. Two included studies reported the VC only,6, 17 three reported only the FVC7, 14, 16 and two reported both the slow and forced vital capacity.8, 18 Where both the FVC and VC were reported in the same papers, only the VC was included in the analyses. RMT increased the VC by 0.40 l (0.12, 0.69) and the FVC by 0.41 l (−0.02, 0.84), giving a combined estimate of benefit of 0.41 l (0.17, 0.64) (Figure 3).
Discussion
This systematic review and meta-analysis focused on the effect of RMT on the full range of pulmonary function measured in tetraplegia. Despite the relatively small number of studies and participants, RMT appears to be particularly effective at increasing vital capacity, inspiratory volumes and strength.
The vital capacity, whether measured as the FVC or the (slow) VC, is a key clinical marker of respiratory health in tetraplegia. In acute injury, a VC below 10 ml per kilogram of body weight predicts the need for intubation,22 and the VC influences both the likelihood of tracheostomy and of weaning success.23 Similarly, in those with chronic SCI, a lower VC is predictive of pulmonary infection24, 25 and mortality risk.26 Separate analyses found a statistically significant benefit on VC for IMT but not on FVC; however, the mean differences for the two comparisons were within 10 ml. As illustrated in Figure 3, when the FVC and (slow) VC data were combined, the magnitude of the mean benefit was essentially unchanged and the precision of the estimate increased. Significant airflow obstruction in the participants from the included studies would reduce the FVC relative to the (slow) VC, but examination of the baseline demographic characteristics from the original papers provides no evidence of airflow obstruction. This observation, coupled with the nearly identical estimate of benefit for the (slow) VC and the FVC, suggests that regardless of the method by which the effect of RMT on vital capacity is measured, the benefit is real. Recently, Postma et al.2 have shown that during the first five years after injury a lower MIP and physical fitness and a higher body mass index are associated with increased pulmonary function decline, as measured by FVC. The current results demonstrate that the vital capacity can be increased with training, and future longitudinal studies should examine whether regular RMT can ameliorate the detrimental effects of ageing with SCI on pulmonary function.
The improvements in MIP, MEP, MVV, VC and IC following RMT that were revealed by the meta-analyses allow us to speculate around causation and mechanisms. The MIP and IC have been directly correlated in previous cross-sectional cohorts27 and the increases observed in this paper are likely to be directly associated with increased strength in the same muscles. Increases in both MIP and IC would likely also result in a larger measured VC despite no change in ‘expiratory’ volumes such as the RV. In people with neuromuscular weakness, MVV can be considered to simultaneously measure respiratory strength, lung capacity and (to a degree) endurance and as such considered as an integrated functional measure of ventilatory capacity. The observed increases in MIP, MEP and VC could thus be considered to have led to the MVV increase. These postulated relationships are obviously associative, but the results of the meta-analysis suggest that RMT overall has proven capacity to improve inspiratory muscle strength and function.
Both the MIP and MEP are very sensitive to the absolute lung volume at which they are measured,28 and this may confound interpretation of the observed results. The meta-analysis did not reveal any systematic effect of RMT on the FRC or RV, and as such it is probable that the MIP was measured at about the same absolute lung volume within subjects in these studies. The MEP, however, may have been affected by the absolute lung volume at which it was measured after training. A higher IC would result in the MEP being measured at a higher absolute lung volume after RMT, and as such lung elastic recoil would contribute to the observed value to a larger degree.27 Further, the absence of any demonstrable increase in ‘expiratory’ measures (PEFR, FEV1 or ERV) despite the observed increase in MEP may suggest that the elastic recoil effect could have predominated. Most participants in these studies had tetraplegia and thus absent or diminished abdominal and other active expiratory muscle function that could have been trained by RMT. Previous research has demonstrated that the clavicular head of the pectoralis major muscle can be trained to increase the ERV;29, 30 however, it is not possible in a systematic review such as this to determine the relative contribution of this particular muscle to the overall results. Invasive, comprehensive measurement of pulmonary mechanics should be considered in future trials of RMT in tetraplegia to understand the relative contribution of lung elastic recoil to any observed improvement in MEP.
The ability to expel air forcefully from the lungs, usually by coughing, is an important determinant of respiratory health and effective pulmonary secretion clearance.31 The current meta-analyses did not demonstrate a significant benefit of RMT on measures associated with an effective cough such as the FEV1 or the PEFR. More direct measures of ‘functional’ cough efficacy have been proposed, such as the ‘peak cough flow’; the PEFR of air expelled during a cough is typically measured using a hand-held ‘asthma’ peak flow meter.31 However, there is little standardization in the literature around peak cough flow measurement. It has been variably measured as unassisted, assisted manually or mechanically and with or without a maximal insufflation to total lung capacity.31, 32 Consideration should be given to the standardization of peak cough flow as an index to enable future comparison and meta-analyses across studies.
An important limitation of this meta-analysis is the inclusion of a few participants with paraplegia in the papers of Van Houtte et al.11 and Litchke et al.15 In any meta-analysis, it is always debatable whether it is better to be broadly inclusive in terms of study selection or to be very selective and specific with the selection of studies to be included. In this paper, we chose to be inclusive to examine the overall question as to whether RMT has a role in tetraplegia. As such, four people with paraplegia were included in the Van Houtte and eight in the Litchke data. It was not possible to separate out the data from the individual participants in these papers, but we performed a sensitivity analysis to examine whether removing these studies affected the conclusions of the meta-analyses. Specifically, if we exclude the Litchke et al.15 paper from analyses, the effect estimate is reduced to 15.94 (3.09, 28.79) but remains statistically significant for MVV. Similarly, if we exclude the Van Houtte et al.11 study, there is no significant change to the findings (revised estimate of VC effect of 0.40 (0.16, 0.64) and a MVV of 16.24 (3.73, 28.75)).
The results of this meta-analysis indicate that RMT is able to increase the functional capacity of the lungs as measured by MVV, which may affect quality-of-life outcomes for people with tetraplegia. Van Houtte et al.11 found that significant improvements in MVV following RMT were coupled with significant improvements in respiratory endurance and health-related quality of life, as measured by the Index of Pulmonary Dysfunction. Litchke et al.15 proposed a similar hypothesis regarding the effect of RMT on overall lung function for wheelchair athletes and the potential subsequent effect on the overall quality of life.
Although 11 studies were included in this review, the meta-analysis relied strongly on the data from five of these.6, 8, 14, 16, 18 The data from three studies were not able to be included,13, 17, 20 and three papers reported data for only one15, 19 or two7 of the meta-analysed outcomes. These low numbers of studies and participants may affect the generalizability of these findings. In addition, many of the included studies grouped the participants as ‘complete’ or ‘incomplete’, with little specific data regarding AIS. Future studies should consider using the published, standardized categories of lesion level and severity.33
Conclusion
Despite the relatively small number of studies included, the meta-analysis revealed that RMT increases inspiratory and VC, inspiratory and expiratory pressures and the MVV in people with tetraplegia. Additional research is needed to determine the optimum dosages and duration of effect and to understand whether RMT confers any longer-term functional benefit.
Data Archiving
There were no data to deposit.
References
DeVivo MJ . Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord 2012; 50: 365–372.
Postma K, Haisma JA, de Groot S, Hopman MT, Bergen MP, Stam HJ et al. Changes in pulmonary function during the early years after inpatient rehabilitation in persons with spinal cord injury: a prospective cohort study. Arch Phys Med Rehabil 2013; 94: 1540–1546.
Cardozo CP . Respiratory complications of spinal cord injury. J Spinal Cord Med 2007; 30: 307–308.
Brown R, DiMarco AF, Hoit JD, Garshick E . Respiratory dysfunction and management in spinal cord injury. Respir Care 2006; 51: 853–868 discussion 869–870.
Sapienza C, Troche M, Pitts T, Davenport P . Respiratory strength training: concept and intervention outcomes. Semin Speech Lang 2011; 32: 21–30.
Mueller G, Hopman MT, Perret C . Comparison of respiratory muscle training methods in individuals with motor and sensory complete tetraplegia: a randomized controlled trial. J Rehabil Med 2013; 45: 248–253.
Van Houtte S, Vanlandewijck Y, Kiekens C, Spengler CM, Gosselink R . Patients with acute spinal cord injury benefit from normocapnic hyperpnoea training. J Rehabil Med 2008; 40: 119–125.
Tamplin J, Baker FA, Grocke D, Brazzale DJ, Pretto JJ, Ruehland WR et al. Effect of singing on respiratory function, voice, and mood after quadriplegia: a randomized controlled trial. Arch Phys Med Rehabil 2013; 94: 426–434.
Brooks D, O'Brien K, Geddes EL, Crowe J, Reid WD . Is inspiratory muscle training effective for individuals with cervical spinal cord injury? A qualitative systematic review. Clinl Rehabil 2005; 19: 237–246.
Sheel AW, Reid WD, Townson AF, Ayas NT, Konnyu KJ . Effects of exercise training and inspiratory muscle training in spinal cord injury: a systematic review. J Spinal Cord Med 2008; 31: 500–508.
Van Houtte S, Vanlandewijck Y, Gosselink R . Respiratory muscle training in persons with spinal cord injury: A systematic review. Respir Med 2006; 100: 1886–1895.
Berlowitz DJ, Tamplin J . Respiratory muscle training for cervical spinal cord injury. Cochrane Database Syst Rev 2013; 7: CD008507.
Zupan A, SÏavrin R, Erjavec T, Kralj A, KarcÏnik T, SÏkorjanc T et al. Effects of respiratory muscle training and electrical stimulation of abdominal muscles on respiratory capabilities in tetraplegic patients. Spinal Cord 1997; 35: 540–545.
Derrickson J, Ciesla N, Simpson N, Imle PC . A comparison of two breathing exercise programs for patients with quadriplegia. Phys Ther 1992; 72: 763–769.
Litchke L, Lloyd L, Schmidt E, Russian C, Reardon R . Comparison of two concurrent respiratory resistance devices on pulmonary function and time trial performance of wheel chair athletes. Ther Recreation J 2010; 44: 51–62.
Roth EJ, Stenson KW, Powley S, Oken J, Primack S, Nussbaum SB et al. Expiratory muscle training in spinal cord injury: a randomized controlled trial. Arch Phys Med Rehabil 2010; 91: 857–861.
Gounden P . Progressive resistive loading on accessory expiratory muscles in tetraplegia. S Afr J Physiother 1990; 46: 4–12.
Liaw MY, Lin MC, Cheng PT, Wong MK, Tang FT . Resistive inspiratory muscle training: its effectiveness in patients with acute complete cervical cord injury. Arch Phys Med Rehabil 2000; 81: 752–756.
Litchke LG, Russian CJ, Lloyd LK, Schmidt EA, Price L, Walker JL . Effects of respiratory resistance training with a concurrent flow device on wheelchair athletes. J Spinal Cord Med 2008; 31: 65–71.
Loveridge B, Badour M, Dubo H . Ventilatory muscle endurance training in quadriplegia: effects on breathing pattern. Paraplegia 1989; 27: 329–339.
Estenne M, De Troyer A . Mechanism of the postural dependence of vital capacity in tetraplegic subjects. Am Rev Respir Dis 1987; 135: 367–371.
Berlly M, Shem K . Respiratory management during the first five days after spinal cord injury. J Spinal Cord Med 2007; 30: 309–318.
Berney SC, Gordon IR, Opdam HI, Denehy L . A classification and regression tree to assist clinical decision making in airway management for patients with cervical spinal cord injury. Spinal Cord 2011; 49: 244–250.
Postma K, Bussmann JB, Haisma JA, van der Woude LH, Bergen MP, Stam HJ . Predicting respiratory infection one year after inpatient rehabilitation with pulmonary function measured at discharge in persons with spinal cord injury. J Rehabil Med 2009; 41: 729–733.
Stolzmann KL, Gagnon DR, Brown R, Tun CG, Garshick E . Risk factors for chest illness in chronic spinal cord injury: a prospective study. Am J Phys Med Rehabil 2010; 89: 576–583.
Garshick E, Kelley A, Cohen SA, Garrison A, Tun CG, Gagnon D et al. A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord. 2005; 43: 408–416.
Kang SW, Shin JC, Park CI, Moon JH, Rha DW, Cho D-h . Relationship between inspiratory muscle strength and cough capacity in cervical spinal cord injured patients. Spinal Cord 2006; 44: 242–248.
ATS/ERS Statement on Respiratory Muscle Testing. Am J Respir Crit Care Med. 2002; 166: 518–624.
Estenne M, Knoop C, Vanvaerenbergh J, Heilporn A, De Troyer A . The effect of pectoralis muscle training in tetraplegic subjects. Am Rev Respir Dis 1989; 139: 1218–1222.
De Troyer A, Estenne M, Heilporn A . Mechanism of active expiration in tetraplegic subjects. N Engl J Med 1986; 314: 740–744.
Chatwin M, Ross E, Hart N, Nickol AH, Polkey MI, Simonds AK . Cough augmentation with mechanical insufflation/exsufflation in patients with neuromuscular weakness. Eur Respir J 2003; 21: 502–508.
Bach JR, Bianchi C, Aufiero E . Oximetry and indications for tracheotomy for amyotrophic lateral sclerosis. Chest 2004; 126: 1502–1507.
DeVivo MJ, Biering-Sorensen F, New P, Chen Y . Standardization of data analysis and reporting of results from the International Spinal Cord Injury Core Data Set. Spinal Cord 2011; 49: 596–599.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Appendix
Appendix
1. exp spinal cord injuries/
2. exp spinal cord ischemia/
3. exp central cord syndrome/
4. (myelopathy adj3 (traumatic or post-traumatic)).ab,ti.
5. ((spine or spinal) adj3 (fracture$ or wound$ or trauma$ or injur$ or damag$)).ab,ti.
6. (spinal cord adj3 (contusion or laceration or transaction or trauma or ischemia)).ab,ti.
7. central cord injury syndrome.ab,ti.
8. central spinal cord syndrome.ab,ti.
9. exp Cervical Vertebrae/in (Injuries)
10. exp spinal cord/
11. SCI.ab,ti.
12. exp paraplegia/
13. exp quadriplegia/
14. (paraplegia* or quadriplegia* or tetraplegia*).ab,ti.
15. or/1–14
16. exp breathing exercises/
17. exp respiratory muscles/
18. exp exercise therapy/
19. (train* or exercis* or endurance or strength* or resistive).ab,ti.
20. 18 or 19
21. 17 and 20
22. normocapnic hyperpnoea training.ab,ti.
23. ((inspiratory or respiratory or breath*) adj5 (endurance or train* or exercis* or resist* or strength*)).ab,ti.
24. RMT.ab,ti.
25. 16 or 21 or 22 or 23 or 24
26. 15 and 25
Rights and permissions
About this article
Cite this article
Tamplin, J., Berlowitz, D. A systematic review and meta-analysis of the effects of respiratory muscle training on pulmonary function in tetraplegia. Spinal Cord 52, 175–180 (2014). https://doi.org/10.1038/sc.2013.162
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2013.162
Keywords
This article is cited by
-
Comparison of two inspiratory muscle training protocols in people with spinal cord injury: a secondary analysis
Spinal Cord Series and Cases (2023)
-
Adherence to and impact of home-based high-intensity IMT in people with spinal cord injury: a pilot study
Spinal Cord Series and Cases (2022)
-
Transcutaneous electrical diaphragmatic stimulation reduces the duration of invasive mechanical ventilation in patients with cervical spinal cord injury: retrospective case series
Spinal Cord Series and Cases (2021)
-
A case for inspiratory muscle training in SCI: potential role as a preventative tool in infectious respiratory diseases like COVID-19
Spinal Cord Series and Cases (2020)
-
The immediate effects of breathing with oscillated inspiratory and expiratory airflows on secretion clearance in intubated patients with cervical spinal cord injury
Spinal Cord (2019)