Abstract
Background and aim Chronic infection with Pseudomonas aeruginosa in patients with cystic fibrosis (CF) causes progressive deterioration in lung function. The purpose of this trial was to assess the efficacy and tolerability of a tobramycin highly concentrated solution for inhalation (TSI) [300mg/4mL; Bramitob®] when added to other antipseudomonal therapies in CF patients with chronic P. aeruginosa infection.
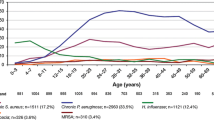
Methods In a multinational, double-blind, multicenter study, CF patients with chronic P. aeruginosa infection were randomized to receive nebulized tobramycin or placebo over a 24-week study period in which 4-week treatment periods (‘on’ cycles) were followed by 4-week periods without treatment (‘off’ cycles). Forced expiratory volume in 1 second (FEV1) percentage of predicted normal was used as the primary efficacy outcome parameter. Forced vital capacity (FVC), forced expiratory flow at 25–75% of FVC (FEF25–75%), P. aeruginosa susceptibility, minimum concentration required to inhibit 90% of strains (MIC90), rates of P. aeruginosa-negative culture, P. aeruginosa persistence and superinfection, need for hospitalization and parenteral antipseudomonal antibiotics, loss of school/working days due to the disease, and nutritional status (bodyweight and body mass index) were considered as secondary efficacy outcome parameters. Adverse events reporting, audiometry, and renal function were monitored to evaluate the tolerability and safety of TSI.
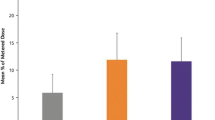
Results A total of 247 patients were randomized in the study. At endpoint time assessment (week 20), FEV1 was significantly increased in the tobramycin group and the adjusted mean difference between groups (intention-to-treat population) was statistically significant (p < 0.001). At the same time, clinically relevant improvements in FVC and FEF25–75% were detected in the TSI group (p = 0.022 and p = 0.001, respectively). The microbiologic outcomes at the end of the last ‘on’ cycle period were significantly better in the TSI group than the placebo group (p = 0.024), although there was a concomitant trend toward an increase in the MIC of isolated P. aeruginosa strains. The percentage of patients hospitalized as well as the need for parenteral antipseudomonal antibiotics was significantly lower in the TSI group (p = 0.002 and p = 0.009, respectively). Patients treated with TSI had fewer lost school/working days due to the disease (p < 0.001). A favorable effect of tobramycin in terms of an increase in bodyweight and body mass index was also noted, when compared with placebo, at all timepoints (p < 0.01 and p < 0.001, respectively). No significant changes in serum creatinine and auditory function were detected. The proportion of patients with drug-related adverse events was 15% in both treatment groups.
Conclusions Long-term, intermittent administration of this aerosolized tobramycin formulation (300mg/4mL) in CF patients with P. aeruginosa chronic infection significantly improved pulmonary function and microbiologic outcome, decreased hospitalizations, increased nutritional status, and was well tolerated.









Similar content being viewed by others
Notes
1 The use of trade names is for product identification purposes only and does not imply endorsement.
References
Smith AL. Inhaled antibiotic therapy. What drug? What dose? What regimen? What formulation? J Cystic Fibrosis 2002; 1: S189–93
Ratjen F, Doring G. Cystic fibrosis. Lancet 2003; 361: 681–9
Ballmann M, Rabsch P, von der Hardt H. Long term follow-up of changes in FEV1 and treatment intensity during Pseudomonas aeruginosa colonisation in patients with cystic fibrosis. Thorax 1998 Sep; 53(9): 732–7
Farrel PM, Shen G, Spolaingard M, et al. Acquisition of Pseudomonas aeruginosa in children with cystic fibrosis. Pediatrics 1997; 100Suppl. 2: 1–9
Moss RB. Administration of aerosolised antibiotics in cystic fibrosis. Chest 2001; 120: 107–113S
Ramsey BW, Pepe MS, Quan JM, et al. Intermittent administration of inhaled tobramycin in patients with cystic fibrosis. N Engl J Med 1999; 340: 23–30
Hodson ME, Gallagher CG, Govan JR. A randomised clinical trial of nebulised tobramycin or colistin in cystic fibrosis. Eur Respir J 2002; 20: 658–64
Poli G, Acerbi D, Pennini R, et al. Clinical pharmacology study of Bramitob®, a tobramycin solution for nebulization, in comparison with Tobi®. Pediatr Drugs 2007; 9Suppl. 1: 3–9
Nikolaizik WH, Trociewicz K, Ratjen F. Bronchial reactions to the inhalation of high-dose tobramycin in cystic fibrosis. Eur Respir J 2002; 20: 122–6
Lenoir G, Antypkin YG, Miano A, et al. Efficacy, safety, and local pharmacokinetics of highly concentrated nebulized tobramycin in patients with cystic fibrosis colonized with Pseudomonas aeruginosa. Pediatr Drugs 2007; 9Suppl. 1: 11–20
Johansen HK, Hoiby N. Seasonal onset of initial colonisation and chronic infection with Pseudomonas aeruginosa in patients with cystic fibrosis in Denmark. Thorax 1992; 47: 109–11
Quanjer PhH, Tammeling GJ, Cotes JE, et al. Lung volumes and forced ventilatory flows. Eur Respir J 1993; 6Suppl. 16: 5–40
Knudson RJ, Lebowitz MD, Holberg CJ. Changes in the normal maximal respiratory flow-volume curve with growth and aging. Am Rev Respir Dis 1983; 127: 725–34
National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing, 13th information supplement. M100-S13. Wayne (PA): NCCLS, 2003
Henry DA, Campbell ME, LiPuma JJ, et al. Identification of Burkholderia cepacia isolates from patients with cystic fibrosis and use of a simple new selective medium. J Clin Microbiol 1997; 35(3): 614–9
Bavenfein A, Rotter K, Weisslein-Pfister C. Selective procedure to isolate Haemophilus influenzae from sputa with large quantities of Pseudomonas aeruginosa. Infection 1987; 15: 64–7
Hodson ME. Treatment of cystic fibrosis in the adult. Respiration 2000; 67(6): 595–607
Lewis JA, Jones DR, Rohmel J. Biostatistical methodology in clinical trials: European guideline. Stat Med 1995; 14: 1655–82
Kerem E, Reisman J, Corey M, et al. Prediction of mortality in patients with cystic fibrosis. N Engl J Med 1992; 326: 1187–91
Gibson RL, Burns JL, Mamsey BW. Pathophysiology and management of pulmonary infections in cystic fibrosis. Am J Respir Crit Care Med 2003; 168: 918–51
Corey M, McLaughlin FJ, Williams M, et al. A comparison of survival growth and pulmonary function in patients with cystic fibrosis in Boston and Toronto. J Clin Epidemiol 1988; 41: 583–91
Bell SC, Bowermann AR, Davies CA, et al. Nutrition in adults with cystic fibrosis. Clin Nutr 1998; 17: 211–5
Wiedemann B, Paul KD, Stern M, et al. Evaluation of body mass index percentiles for assessment of malnutrition in children with cystic fibrosis. Eur J Clin Nutr. Epub 2007 Jan 10
Moss RB. Long-term benefits of inhaled tobramycin in adolescent patients with cystic fibrosis. Chest 2002; 121: 55–63
Murray TS, Egan M, Kazmierczak BI. Pseudomonas aeruginosa chronic colonization in cystic fibrosis patients. Curr Opin Pediatr 2007 Feb; 19(1): 83–8
Taccetti G, Campana S, Festini F, et al. Early eradication therapy against Pseudomonas aeruginosa in cystic fibrosis patients. Eur Respir J 2005; 26: 458–61
Jones AM. Eradication therapy for early Pseudomonas infection in CF: many questions still unanswered. Eur Respir J 2005; 26: 373–5
Yankaskas JR, Marshall BC, Sufian B, et al. Cystic fibrosis adult care: consensus conference report. Chest 2004; 125: 1–39S
Burns JL, Van Dalfsen JM, Shawar RM, et al. Effect of chronic intermittent administration of inhaled tobramycin on respiratory microbial flora in patients with cystic fibrosis. J Infect Dis 1999; 179: 1190–6
Nikolaizik WH, Jenni-Galovic V, Schoni M. Bronchial constriction after nebulised tobramycin in patients with cystic fibrosis colonized with Pseudomonas aeruginosa. Eur J Pediatr 1995; 155: 608–11
Ramagopal M, Lands LC. Inhaled tobramycin and bronchial hyperactivity in cystic fibrosis. Pediatr Pulmonol 2000; 29: 366–70
Nikolaizik WH, Trociewicz K, Ratjen F. Bronchial reactions to the inhalation of high-dose tobramycin in cystic fibrosis. Eur Respir J 2002; 20: 122–6
Modi AC, Quittner AL. Barriers to treatment adherence for children with cystic fibrosis and asthma: what gets in the way? J Pediatr Psychol 2006; 31: 846–58
Acknowledgments
The authors would like to thank Chiesi Farmaceutici S.p.A. (Parma, Italy) for their support in conducting this trial, and MDS Pharma Services (Paris, France) for the study implementation and periodic monitoring of the trial. The sponsor is indebted to Prof. A. Chuchalin, Scientific Research Pulmonology Institute, Russian State Medical University, Moscow, Russia and Prof. H. Mazurek, Bronchiology and Cystic Fibrosis Center, Department of National Research Institute for Tuberculosis and Lung Diseases, Rabka Hospital, Poland for their contributions to the study design as well as their review of the manuscript, and to the patients and their families for their participation in the study.
In addition to the main investigators, the following authors participated in the study: F. Gönzi (Kenézy Hospital, Debrecen, Hungary), K. Holics (Heim Pál Hospital, Budapest, Hungary), E. Sólyom (Miskolc Country Hospital, Miskolc, Hungary), G. Dobra (Petz Aladar County Hospital, Gyor, Hungary), T. Dolinay (Josa Andras Kohraz Gyermekosztaly, Nyiregyhaza, Hungary), A. Szabo (Children’s Hospital, Szeged, Hungary), J. Kus (I Klinika Chorob Pluc Instytutu Gruzlicy I Chorob Pluc, Warszawa, Poland), M. Kaczmarski (III Klinika Chorob Dzieci AM w Bialymstoku, Bialystok, Poland), J. Alkiewicz (Department of Pediatric Pneumonology and Allergic Diseases, Poznań, Poland), T. Latoś (Rehabilitation Department, Institute of Mother and Child, Karpacz, Poland), W. Mŧynarczyk (Department of Lung Diseases, Medical Academy, Poznań, Poland), I. Stelmach (Marie Skŧodowska Curie Hospital, Department of Pediatrics and Allergology, Lodz, Poland), T. Gembitskaya (Scientific Research Pulmonological Institute of St. Petersburg, State Medical University, St. Petersburg, Russia), A. Orlov (St. Olga City Pediatric Hospital, Pulmonological Department, St. Petersburg, Russia).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chuchalin, A., Csiszér, E., Gyurkovics, K. et al. A Formulation of Aerosolized Tobramycin (Bramitob®) in the Treatment of Patients with Cystic Fibrosis and Pseudomonas aeruginosa Infection. Pediatr-Drugs 9 (Suppl 1), 21–31 (2007). https://doi.org/10.2165/00148581-200709001-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00148581-200709001-00004