Abstract
Objective
To determine the frequency, characteristics and outcomes of severe agitation among ventilated medical intensive care unit (MICU) patients.
Design
Prospective cohort study.
Setting
Eighteen-bed MICU in 964-bed tertiary care center.
Patients
All ventilated patients, aged 18 years or older and admitted for more than 24 h between January 1, 2001 and May 8, 2001.
Interventions
None.
Measurements
Data were collected daily by concurrent chart abstractions. Variables included sociodemographic, clinical, laboratory, pharmacologic and non-pharmacologic interventions, ventilator settings and adverse events. Severe agitation, the main outcome variable, was defined as two or more Motor Activity Assessment Scale (MAAS) scores above 4 in a 24-h period and sedative and/or narcotic doses above the established sedation and analgesia protocol or a combination of two or more sedatives.
Results
Twenty-three (16.1%) of 143 enrolled patients exhibited severe agitation. Agitated patients were younger (hazard ratio [HR] 1.32), more likely to be admitted from an outside hospital ICU (HR 2.48), had lower pH (HR 1.55) and PaO2/FIO2 less than 200 mmHg (HR 2.59). Agitated patients had longer MICU stays (median 12 versus 5 days, p<0.0001) and more ventilator days (median 14 versus 6, p<0.0001). Agitated patients were more likely to self-extubate (26% versus 6%, p=0.002). Benzodiazepines, narcotics and neuromuscular blocking agents were administered more frequently and at higher doses, but haloperidol was not.
Conclusion
Severe agitation occurs commonly in critically ill patients and is associated with adverse events including longer ICU stays, duration of mechanical ventilation and self-extubation.
Similar content being viewed by others
Introduction
Stress and mechanical ventilation contribute to the frequent need for sedative and/or analgesic agents [SAAs] as well as non-pharmacologic management of pain, anxiety and agitation [1, 2, 3, 4, 5]. Recently, we found 85% of ventilated patients received SAAs [6]. Clinical experience has shown that subsets of patients have agitation that is difficult to manage. In the absence of an evident medical cause, clinicians often respond to ongoing or severe agitation by increasing doses of SAAs and by using multiple medications. Occasionally, a neuromuscular blocking agent may be required to facilitate mechanical ventilation. High doses and/or multiple medications come with increased likelihood of adverse drug reactions, weaning time and ICU length of stay [5, 7, 8, 9]. Yet, if the patient’s agitation is not managed, he/she may be compromised physiologically and is at greater risk of disrupting critical therapies.
The use of guidelines regarding ICU sedation, analgesia and neuromuscular blocking agents confer benefits, such as fewer ventilator days [6, 10]. In spite of the risks of agitation in ventilated ICU patients, little is known regarding its frequency, associated risk factors, practice patterns or clinical outcomes. Understanding patient risk factors allows clinicians to identify high-risk patients early and implement appropriate, targeted interventions.
Our hypothesis is that severe agitation in intubated patients will have an impact on selected outcomes such as: mortality, ICU length of stay and interruption of therapy. Thus, the aims of this prospective cohort study were to determine the frequency of severe agitation in intubated MICU patients; to identify patient characteristics associated with severe agitation; to describe associated non-pharmacologic and pharmacologic measures (i.e., medicated within the MICU guidelines) and to determine clinical outcomes associated with severe agitation.
Methods
Setting
The study took place in a closed, 18-bed medical intensive care unit (MICU) within The Cleveland Clinic Foundation (CCF), a 964-bed tertiary referral center. Patients are admitted under the direct care and supervision of the MICU medical staff consisting of board certified, attending pulmonary/critical care staff, pulmonary/critical care fellows and residents and interns from the internal medicine program. Interdisciplinary rounds are conducted daily and house officers write all orders.
The nurse-to-patient ratio is 1:2. Nurses assess each patient’s level of agitation and assign a score using the Motor Activity Assessment Scale (MAAS), a 7-point scale ranging from 0 (unresponsive, does not move to noxious stimuli) to 6 (dangerously agitated) (Table 1) [11] that has been tested for inter-rater reliability in our MICU [12]. Nurses assess and document each patient’s level of sedation and motor activity every 4 h and with changes in sedation. House staff use the MICU Sedation and Analgesia Guidelines, adapted from the American College of Critical Medicine (See the electronic supplementary material) [5, 7] and indicate the targeted sedation score or activity level, e.g., MAAS 1–3; the nurse administers the amount of medication judged necessary to maintain the patient within the targeted score. The sedation goal is reassessed daily, along with attempts to decrease the dose of sedatives/analgesics; daily interruption of sedation is not practiced [13]. For patients who received a neuromuscular blocking agent, nurses evaluate physiological variables, endotracheal tube placement, hemodynamic status, pain status, train-of-four measurement and sedation score (See the electronic supplementary material). All patients who receive a neuromuscular blocking agent are administered sedatives and analgesics. The decision to utilize paralysis was based on the attending physician’s judgement and individualized in every patient. A critical care clinical pharmacist monitors the daily doses and type of SAAs, and the sedation score.
Typically, before the patient with agitation is treated with medications, the nurse and physician perform a comprehensive evaluation to rule out organic reasons for the agitation, such as severe hypoxemia, pain or a new neurologic event. Besides pharmacologic measures, nurses utilize a variety of non-pharmacologic measures to reduce or manage agitation, such as: minimizing noise and light and using quiet music. Protocols for management of invasive mechanical ventilation and weaning/discontinuation are used in all patients receiving mechanical ventilation [14]. The modality of mechanical ventilation used is volume cycle assist control.
Participants
All consecutively admitted patients from January 8, 2001 through May 8, 2001, who were 18 years old or more and received mechanical ventilation were eligible for enrollment in the study. The only exclusion criterion was length of stay less than 24 h. Participants or their family members provided informed consent prior to any data collection. The institutional review board approved the study. No effort was made to disguise the study from the medical and nursing staff.
Outcome measures
The primary outcome measure was severe agitation. There is no well-accepted definition of severe agitation in the literature; we based our definition on two components: hyperactive behavior judged to be dangerous and doses of SAAs higher than the recommended guideline dosages [6]. Severe agitation was prospectively defined as: (1) two or more MAAS scores higher than 4 in a 24-h period, (Table 1) [5, 11] and (2) SAA doses above the MICU Sedation and Analgesia Guidelines or (3) the combination of two sedatives within the same 24-h period (i.e., lorazepam and propofol) because maximal doses of one of the sedatives did not achieve adequate sedation. Prior to the study, four external intensivists agreed that the proposed definition was adequate. A panel of MICU clinicians confirmed the classification of patients (agitated or non-agitated) and to assure the absence of inadequate sedation due to underdosing.
Data collected on admission included demographic characteristics, admission source, baseline severity of illness as measured by the Acute Physiology and Chronic Health Evaluation (APACHE) II [15], admitting diagnoses, alcohol or drug use, history of smoking, selected psychiatric diagnoses (manic depression, depression, anxiety, schizophrenia), and reason for ventilation.
Daily data collection included: the last recorded arterial blood gases with corresponding ventilator settings, laboratory values (white blood count, sodium, potassium, glucose, magnesium, phosphate, hematocrit, liver function tests, creatinine, blood urea nitrogen, albumin, total protein), nursing interventions (music, relaxation television channel, encourage family visitation, position for comfort, post orienting objects, reorientation, physical restraints), and total doses of sedatives, analgesics or neuromuscular blocking agents. Documented new conditions or adverse events occurring during the MICU stay included: ethanol withdrawal, encephalopathy, delirium, psychosis, acute renal failure, gastrointestinal bleeding, pneumothorax, sepsis, nosocomial infection, new stroke, adverse drug reaction, new pulmonary embolism, deep vein thrombosis, metabolic acidosis, tracheotomy or other event. Finally, we recorded discharge disposition, length of stay, weaning status and patient-disruption of endotracheal tubes, arterial lines or nasogastric tubes.
Trained ICU registered nurses using standardized data collection instruments gathered all information daily. Weekly quality checks were conducted by one of two investigators (JW, RM) to ensure inter-rater reliability. The data were coded and entered by the personnel in the Department of Biostatistics and Epidemiology. Chart audits were performed for all suspicious or missing data. Data were then transferred to SAS data sets for analysis.
Statistics
Descriptive statistics included frequencies and percentages for categorical variables and means, standard deviations and medians and ranges for continuous level variables. Cox-proportional hazards with time-varying covariates were used to model the time until patients became agitated [16]. The resulting estimates are reported as hazard ratios (95% confidence interval). Probability values test the hypothesis that the hazard ratios =1.0. Outcomes were examined between the two groups by using chi-square tests for categoric variables and Wilcoxon-rank sum tests for skewed variables. All time-to-event analyses were performed using S-PLUS 6.1 (Insightful, Seattle, WA). All other analyses were performed using SAS software (version 8.0, SAS Institute, Cary, NC).
Results
Characteristics of the study group
During the study, 350 patients were admitted to the MICU. One hundred forty-three consecutive patients were enrolled; no eligible patient was excluded. Fifty percent were men and the median age was 62.0 years (range 22.5–98.1 years). Twenty-five percent were admitted from outside hospitals. Hypoxic respiratory failure was the most frequent admitting diagnosis and most frequent reason (58%) for mechanical ventilation. The mean tidal volume was 6.6 ml/kg (SD=2) of actual body weight. Fifty-two patients (36.3%) had findings consistent with acute lung injury or the acquired respiratory distress syndrome at 24 hours of admission [17]. The median APACHE II score on admission was 20 (range 6–38). The median length of MICU stay was 6.0 days (range 1–40 days). The median duration of mechanical ventilation was 7 days (range 1–44 days). Nine percent extubated themselves. Sixty-eight percent were discharged to one of the hospital general units and the MICU mortality was 28%.
Occurrence of severe agitation
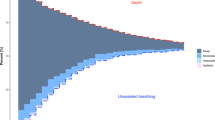
Twenty-three patients, 16.1% (95% CI 10.9–23.0%) of ventilated patients admitted to the MICU, were severely agitated at some point during their MICU stay. Ten (7%) patients became severely agitated during their first 24 h in the MICU. The long-term rate of agitation (the probability of experiencing severe agitation if in the MICU for longer than 14 days) was estimated to be 33.5% (95% CI 13.4–49.0%).
Features associated with severe agitation
Table 2 shows patients’ characteristics at the time of admission to the MICU. The characteristics that differed significantly between those who developed severe agitation versus those who did not were younger age (50.2 versus 62.6 years, p=0.0016) and more frequently admitted from an outside hospital (48% versus 21%, p=0.0158). Those admitted from outside hospitals were more likely to develop severe agitation within the first 24 h of admission compared to patients admitted from other sources (17% versus 4%, p 0.0085).
Features on admission significantly associated with the development of severe agitation included younger age, admission from an outside hospital, marijuana use and currently not married (Table 3). Over the course of the hospitalization, features preceding or concurrent with the onset of severe agitation included: (1) increased FIO2, (2) PaO2/FIO2 below 200 mmHg and (3) decreased pH. Multivariate models showed that younger age, admission from another hospital, lower pH and PaO2/FIO2 below 200 mmHg were associated with severe agitation (Table 4).
Notably, no associations with laboratory indices or onset of adverse events before the onset of severe agitation were found. There was no significant difference between the two groups in term of ventilator settings including size of the tidal volume and the level of positive end-expiratory pressure. During the MICU stay, 2 (8.7%) of the severely agitated patients and 6 (5%) of the non-agitated patients had delirium noted in the medical records.
Management
Both benzodiazepines and opiates were administered more frequently and in greater doses to those experiencing severe agitation both prior to or on the day of agitation onset as well as throughout the MICU stay as compared to those who did not experience severe agitation (See Table in ESM). For example, 96% of the severely agitated patients received lorazepam at some point during their MICU stay compared to 75% of non-severe agitation patients (p=0.028), and 91% of the severely agitated patients received lorazepam by continuous intravenous infusion compared with 26% of non-severe agitation patients (p<0.001). Haloperidol was administered to only 4% of severely agitated patients prior to or on the day of onset. Thirty percent of severely agitated patients received haloperidol at some point during their MICU stay compared to 20% of non-severely agitated patients (p=0.27). Neuromuscular blocking agents were administered to 48% of the severely agitated patients versus to 11% of the non-severely agitated patients (p<0.0001). In all patients, the indication for the use of a neuromuscular blocking agent was to facilitate mechanical ventilation. Patients that were severely agitated received more continuous intravenous infusions of opiates and in higher doses when compared with the non-agitated group (See ESM Table, S2). No association with nursing interventions prior to or after severe agitation onset was found.
Outcomes associated with severe agitation
Outcomes associated with having severe agitation included (Table 5): longer ICU stay (12 versus 5 days, p<0.0001), longer duration of mechanical ventilation (14 versus 6 days, p<0.0001) and greater frequency of self-extubation (26 versus 6%, p=0.002). Eighty-six percent of agitated patients who self-extubated from mechanical ventilation required reintubation as compared to 17% of non-agitated patients who self-extubated (Fisher’s exact test p=0.029). No significant difference in ICU survival rates was observed.
Discussion
Severe agitation in mechanically ventilated patients is a significant clinical issue confronting critical care nurses and physicians. The main findings of this prospective cohort study were: (1) severe agitation occurs in 16% of mechanically ventilated patients; (2) correlates of severe agitation were younger age, transfer to the ICU from another hospital, acidemia and worsened oxygenation; and (3) the occurrence of severe agitation was associated with adverse outcomes including longer ICU stay, longer duration of mechanical ventilation and a higher rate of self-extubation, but was not associated with higher mortality.
Fraser et al. [18] observed severe agitation more frequently (46%) among ICU patients; unlike our findings, they observed no age-related differences in the occurrence of severe agitation. Possible explanations for these discrepancies include differences in inclusion criteria (e.g., we studied only mechanically ventilated patients, while Fraser et al. [18] studied ventilated and non-ventilated patients), definition of severe agitation and our use of a protocol [6] to manage SAAs. Indeed, to the extent that such protocols can lessen the frequency of severe agitation, we speculate that the lower frequency in our series may reflect this practice. Also, to the extent that agitation represents a hyperactive subtype of delirium [19, 20, 21], the lower rate of such delirium among patients older than 65 years may contribute to the higher frequency of agitation observed among younger patients [20, 21].
Our observation that severe agitation was more common among patients transferred from other hospitals invites comment. The possibility that such transferred patients were sicker than those admitted from within our hospital or emergency department is belied by similar APACHE II scores (data not shown). On the other hand, others have shown that patients transferred from outside hospitals experience a higher rate of mortality that is not reflected in APACHE scores. Presumably the higher rate of mortality reflects post-admission developments that prompt transfer for management, but which are not present, and therefore not captured by APACHE ratings, at the time of initial ICU admission [22, 23, 24]. Recently, Rosenberg et al. [24] found that patients transferred to the MICU of a tertiary center have a longer hospital stay and higher mortality rate compared with patients admitted directly to the MICU. Another plausible explanation is that variation in practices may account for the severe agitation in the transferred group; it is unknown to what extent sedation and analgesia protocols were utilized by referring hospitals.
The association of severe agitation with PaO2/FIO2 lower than 200 mmHg may reflect the contribution of severe hypoxemia to the development of agitation [19]. Also, the worse acidemia in severely agitated patients may reflect their greater degree of illness or their having received high-dose intravenous lorazepam, which can cause metabolic acidosis mediated by the large volumes of infused propylene glycol as the vehicle for lorazepam [25]. While severe hypoxemia and acidemia are markers of severe lung dysfunction and the need for greater ventilatory support, there was no significant difference between the groups in terms of ventilatory settings, including tidal volume and level of positive end-expiratory pressure.
Because severely agitated patients received higher doses of sedatives and analgesics (see ESM Table, S2) and because continuous infusions of sedatives has been associated with longer duration of mechanical ventilation [7], it is conceivable that medication use contributed to longer mechanical ventilation. The length of ICU stay for the non-agitated group was within the range reported recently by others [10, 13, 26]. The overall incidence of therapy disruption among severely agitated patients was higher than that of non-agitated patients and reflects findings by others of the association of agitation with therapy disruption [27, 28, 29, 30, 31]. Though not observed in this series, self-extubation has been associated with a higher ICU mortality rate [26]. Also, patient-initiated device removal incurs higher ICU costs [27, 32].
Several authors have suggested the use of non-pharmacologic measures, such as minimizing noise and light, may be helpful in the management of the agitated critical care patient [1, 5, 33, 34, 35]. There was no difference in the frequency of use of these measures by the nurses. Rather, our team relied on pharmacologic measures. Non-pharmacologic strategies for the treatment of delirium have been underutilized in hospital and ICU settings [33, 34]. In the future, it will be important to assess the impact that these measures have on the management and outcomes of the severely agitated patient.
Intensive care unit clinicians are confronted with the paradox of a subset of patients who, despite the fact of their having received higher doses of SAAs, disrupt their therapy more frequently and remain for a longer period of time in the MICU on mechanical ventilation. It is clear that our current sedation and analgesia protocol, based on the previous and the most recent practice guidelines of the ACCCM [5, 35], is inadequate to manage the severely agitated patient. Clinicians need to modify the diagnostic strategy and therapy to improve the management of these patients. Patients should be systematically evaluated for the presence of delirium and, in the presence of delirium, the choice of haloperidol should be increased in this patient population [2, 20, 36, 37].
Several potential shortcomings of the current study warrant mention. First, at the time of this study there was no systematic assessment for delirium among mechanically ventilated patients [2, 36]. Indeed, few patients in our sample were diagnosed as having delirium, a finding reported in studies of hospitalized patients [38, 39, 40]. Because the diagnosis of delirium would prompt the administration of haloperidol rather than analgesics or sedatives, it is conceivable that the occurrence of severe agitation among mechanically ventilated patients despite the use of a protocol may, in part, reflect this. A second potential limitation of our study is that the results from our ICU, based in a tertiary care institution and with active use of a protocol to guide sedation, may not generalize to other settings. We did not disguise the study from the medical and nursing staff, therefore staff may have altered their behavior. This is unlikely; our unit has used the same sedation protocol and agitation guidelines for the last 7 years. Lastly, because this is an observational study, we are unable to offer new insights in terms of the pathogenesis, prevention and management of severe agitation.
In conclusion, notwithstanding these potential limitations, our results confer better understanding of the frequency, correlates and outcomes associated with severe agitation. Both the frequency of severe agitation and the gravity of consequences suggest the need for greater strategies to lessen its occurrence among mechanically ventilated patients. Physicians’ and nurses’ assessment of delirium and early pharmacologic approaches to treat agitation are essential.
References
Fontaine DK (1994) Nonpharmacologic management of patient distress during mechanical ventilation. Critical Care Clinics 10:695–708
Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, Truman B, Speroff T, Gautam S, Margolin R, Hart RP, Dittus R (2001) Delirium in mechanically ventilated patients: validity and reliability of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). JAMA 286:2703–2710
Ely EW, Gautam S, Margolin R, Francis J, May L, Speroff T, Truman B, Dittus R, Bernard R, Inouye SK (2001) The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med 27:1892–1900
Ostermann ME, Keenan SP, Seiferling RA, Sibbald WJ (2000) Sedation in the intensive care unit: a systematic review. JAMA 283:1451–1459
Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM, Crippen DW, Fuchs BD, Kelleher RM, Marik PE, Nasraway SA Jr, Murray MJ, Peruzzi WT, Lumb PD (2002) Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 30:119–141
Bair N, Bobek MB, Hoffman-Hogg L, Mion LC, Slomka J, Arroliga AC (2000) Introduction of sedative, analgesic and neuromuscular blocking agent guidelines in a medical intensive care unit: physician and nurse adherence. Crit Care Med 28:707–713
Kollef MH, Levy NT, Ahrens TS, Schaiff R, Prentice D, Sherman G (1998) The use of continuous IV sedation is associated with prolongation of mechanical ventilation. Chest 114:541–548
Hsiang JK, Chesnut RM, Crisp CB, Klauber MR, Blunt BA, Marshall LF (1994) Early, routine paralysis for intracranial pressure control in severe head injury: is it necessary? Crit Care Med 22:1471–1476
Murray MJ, Cowen J, DeBlock H, Erstad B, Gray AW Jr, Tescher AN, McGee WT, Prielipp RC, Susla G, Jacobi J, Nasraway SA Jr, Lumb PD (2002) Clinical practice guidelines for sustained neuromuscular blockade in the adult critically ill patient. Crit Care Med 30:142–156
Brook AD, Ahrens TS, Schaiff R, Prentice D, Sherman G, Shannon W, Kollef MH (1999) Effect of a nursing-implemented sedation protocol on the duration of mechanical ventilation. Crit Care Med 27:2609–2615
Devlin JW, Boleski G, Mlynarek M, Nerenz DR, Peterson E, Jankowski M, Horst HM, Zarowitz BJ (1999) Motor Activity Assessment Scale: a valid and reliable sedation scale for use with mechanically ventilated patients in an acute surgical intensive care unit. Crit Care Med 27:1271–1275
Hogg LH, Bobek MB, Mion LC, Legere BM, Banjac S, VanKerkhove K, Arroliga AC (2001) Interrater reliability of 2 sedation scales in a medical intensive care unit: a preliminary report. Am J Crit Care 10:79–83
Kress JP, Pohlman AS, O’Connor MF, Hall JB (2000) Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 342:1471–1477
MacIntyre NR, Cook DJ, Ely EW Jr, Epstein SK, Fink JB, Heffner JE, Hess D, Hubmayer RD, Scheinhorn DJ, American College of Chest Physician; American Association of Respiratory Care; American College of Critical Care Medicine (2001) Evidence-based guidelines for weaning and discontinuing ventilatory support. Chest 120:375S–395S
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Therneau TM, Grambsch PM (2000) Modeling survival data: extending the Cox model. Springer, New York
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Le Gall JR, Morris A, Spragg R (1994) The American-European consensus conference on ARDS. Definitions, mechanism, relevant outcomes and clinical trial coordination. Am J Respir Crit Care Med 149:818–824
Fraser GL, Prato BS, Riker RR, Berthiaume D, Wilkins ML (2000) Frequency, severity and treatment of agitation in young versus elderly patients in the ICU. Pharmacotherapy 20:75–82
Ely EW, Siegel MD, Inouye SK (2001) Delirium in the intensive care unit: an under-recognized syndrome of organ dysfunction. Semin Respir Crit Care Med 22:115–126
O’Keefe ST, Lavan JN (1999) Clinical significance of delirium subtypes in older people. Age and Ageing 28:115–119
Marcantonio E, Ta T, Duthie E, Resnick NM (2002) Delirium severity and psychomotor types: their relationship with outcomes after hip fracture repair. J Am Geriatr Soc 50:850–857
Clough JD, Kay R, Gombeski WR Jr, Nickelson DE, Loop FD (1993) Mortality of patients transferred to a tertiary care hospital. Cleve Clin J Med 60:449–454
Escarce JJ, Kelley MA (1991) Admission source to the medical intensive care unit predicts hospital death independent of APACHE II score. JAMA 264:2389–2394
Rosenberg AL, Hofer TP, Strachan C, Watts CM, Hayward RA (2003) Accepting critically ill transfer patients: adverse effect on a referral center’s outcome and benchmark measures. Ann Intern Med 138:882–890
Tuohy KA, Nicholson WJ, Schiffman F (2003) Agitation by sedation. Lancet 361:308
Freire AX, Afessa B, Cawley P, Phelps S, Bridges L (2002) Characteristics associated with analgesia ordering in the intensive care unit and relationships with outcome. Crit Care Med 30:2468–2472
Fraser GL, Riker RR, Prato BS, Wilkins ML (2001) The frequency and cost of patient-initiated device removal in the ICU. Pharmacotherapy 21:1–6
Atkins PM, Mion LC, Mendelson W, Palmer RM, Slomka J, Franko T (1997) Characteristics and outcomes of patients who self-extubate from ventilatory support: a case-control study. Chest 112:1317–1323
Vassal T, Anh NG, Gabillet JM, Guidet B, Staikowsky F, Offenstadt G (1993) Prospective evaluation of self-extubations in a medical intensive care unit. Intensive Care Med 19:340–342
Betbese AJ, Perez M, Bak E, Rialp G, Mancebo J (1998) A prospective study of unplanned endotracheal extubation in intensive care unit patients. Crit Care Med 26:1180–1186
Carrion MI, Ayuso D, Marcos M, Paz Robles M, de la Cal MA, Alia I, Esteban A (2000) Accidental removal of endotracheal and nasogastric tubes and intravascular catheters. Crit Care Med 28:63–66
Happ MB (2000) Using a best practice approach to prevent treatment interference in critical care. Prog Cardiovasc Nurs 15:58–62
Meagher DJ (2001) Delirium: optimizing management. BMJ 322:144–149
Cohen IL, Abraham E, Dasta JF, Gallagher JT, Papadakos PJ, Pohlman AS (2002) Management of the agitated intensive care unit patient. Crit Care Med 30:S97–S123
Shapiro BA, Warren J, Egol AB, Greenbaum DM, Jacobi J, Nasraway SA, Schein RM, Spevetz A, Stone JR (1995) Practice parameters for intravenous analgesia and sedation for adult patients in the intensive care unit. An executive summary. Crit Care Med 23:1596–1600
Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y (2001) Intensive care delirium screening checklist: evaluation of a new screening tool. Intensive Care Med 27:859–864
Francis J, Martin D, Kapoor WN (1990) A prospective study of delirium in hospitalized elderly. JAMA 263:1097–1101
Szokol JW, Vender JS (2001) Anxiety, delirium and pain in the intensive care unit. Crit Care Clinics 17:821–842
Inouye SK, Foreman MD, Mion LC, Katz KH, Cooney LM Jr (2001) Nurses’ recognition of delirium and its symptoms. Arch Intern Med 161:2467–2473
Rockwood K, Cosway S, Stolee P, Kydd D, Carver D, Jarrett P, O’Brien B (1994) Increasing the recognition of delirium in elderly patients. J Am Geriatr Soc 42:252–256
Author information
Authors and Affiliations
Corresponding author
Additional information
This research was partially supported by Nursing Education and Research Fund. Presented in part at the 2002 Annual Meeting of Society of Critical Care Medicine, San Diego, California.
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Woods, J.C., Mion, L.C., Connor, J.T. et al. Severe agitation among ventilated medical intensive care unit patients: frequency, characteristics and outcomes. Intensive Care Med 30, 1066–1072 (2004). https://doi.org/10.1007/s00134-004-2193-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-004-2193-9