Abstract
Objective
This study evaluated the efficacy of noninvasive continuous positive pressure (CPAP) ventilation in infants with severe upper airway obstruction and compared CPAP to bilevel positive airway pressure (BIPAP) ventilation.
Design and setting
Prospective, randomized, controlled study in the pulmonary pediatric department of a university hospital.
Patients
Ten infants (median age 9.5 months, range 3—18) with laryngomalacia (n=5), tracheomalacia (n=3), tracheal hypoplasia (n=1), and Pierre Robin syndrome (n=1)
Interventions
Breathing pattern and respiratory effort were measured by esophageal and transdiaphragmatic pressure monitoring during spontaneous breathing, with or without CPAP and BIPAP ventilation.
Measurements and results
Median respiratory rate decreased from 45 breaths/min (range 24–84) during spontaneous breathing to 29 (range 18–60) during CPAP ventilation. All indices of respiratory effort decreased significantly during CPAP ventilation compared to unassisted spontaneous breathing (median, range): esophageal pressure swing from 28 to 10 cmH2O (13–76 to 7–28), esophageal pressure time product from 695 to 143 cmH2O/s per minute (264–1417 to 98–469), diaphragmatic pressure time product from 845 to 195 cmH2O/s per minute (264–1417 to 159–1183) During BIPAP ventilation a similar decrease in respiratory effort was observed but with patient-ventilator asynchrony in all patients.
Conclusions
This short-term study shows that noninvasive CPAP and BIPAP ventilation are associated with a significant and comparable decrease in respiratory effort in infants with upper airway obstruction. However, BIPAP ventilation was associated with patient-ventilator asynchrony.
Similar content being viewed by others
Introduction
Upper airways obstruction due to congenital abnormalities of the larynx and trachea can cause severe respiratory distress in infancy [1, 2]. Although laryngomalacia is the most frequent congenital abnormality of the larynx and the most common cause of stridor in newborns and infants [3, 4, 5], it usually resolves by the second year of life and rarely requires specific treatment [6]. However, in up to 14% of cases the prognosis is less favorable, requiring a supraglottoplasty or even a tracheotomy to relieve the obstruction [2, 7].
Noninvasive positive pressure ventilation (NPPV), which incorporates both continuous positive airway pressure (CPAP) [8, 9] and bilevel positive airway pressure (BIPAP) ventilation [10], has been recognized as an effective treatment of upper airway obstruction associated with alveolar hypoventilation in children and infants with obstructive sleep apnea [8, 9] and chronic stridor due to laryngomalacia [10]. BIPAP ventilation has been show efficiently to unload the respiratory muscles and improve alveolar ventilation in young children with laryngomalacia [10]. CPAP delivers a continuous distending pressure throughout the respiratory cycle, and this mode is the cornerstone of the ventilatory support that has been successfully used in these patients [8, 9, 11]. However, BIPAP ventilation, which employs both CPAP and a patient-triggered additional positive pressure during inspiration, is an alternative mode that has proved beneficial in adult patients and young children [10, 12]. The rationale for using this mode over CPAP is that it not only reduces the upper airway obstruction due to the collapse during inspiration but also provides additional inspiratory pressure support which could potentially contribute to greater unloading of the respiratory muscles, although this has not been demonstrated in pediatric patients with upper airway obstruction. The aim of the present study was therefore to perform a physiological evaluation to assess the efficacy of NPPV in infants and then to compare the efficacy of CPAP and BIPAP ventilation in this age group.
Material and methods
We studied ten patients (five boys, five girls) with median age of 9.5 months (range 3–18; four under 6 months) and median weight of 7.6 kg (range 4.6–9.8). Clinical characteristics are presented in Table 1. Criteria for inclusion were the presence of severe upper airway obstruction documented on a laryngotracheal endoscopy under general anesthesia. Exclusion criteria were severe mental retardation excluding the possibility to initiate NPPV at home, important midfacial deformity excluding the tolerance of a nasal or a facial mask, inability to close the mouth, and enrollment in other investigative protocols. All the patients were naive to NPPV. All had sleep disturbance, apnea and hypopnea, desaturation, and hypercapnia documented by polysomnography. Laryngomalacia was the most common cause of upper airway obstruction, affecting 50% of the patients. Three patients had tracheomalacia and one a tracheal hypoplasia. NPPV was started in patient numbers 5 and 9 after an unsuccessful attempt to definitely remove a tracheostomy; in these two patients the tracheostomy was not in place at the start of NPPV. Four patients had associated disorders: trisomy 21 (n=3), interventricular communication with surgical repair (n=1), and bronchopulmonary dysplasia (n=1). Upper airway obstruction persisted in all the infants despite tonsillectomy, endoscopic resection of the aryepiglottic folds, and antireflux treatment using proton pump inhibitors, and all required nutritional support by gastrostomy because of failure to thrive. The study was approved by our institutional board and written informed consent was obtained from all parents.
Experimental apparatus
NPPV was delivered by a home pressure support ventilator (BiPAP Harmony or BiPAP Synchrony, Respironics, Murrysville, Calif., USA) through a well fitting custom-molded nasal mask with a dead space less than 5 ml. These two ventilators were evaluated during the study because the Synchrony is thought to have a more sensitive trigger system than the Harmony. The assignment of the ventilator was performed in a random order, with five patients (nos. 1, 3, 4, 7, 10) ventilated with the Harmony device and the five (nos. 2, 5, 6, 8, 9) with Synchrony. The custom-made nasal masks were molded as the child sucked on their pacifier in order to favor simultaneous closure of the mouth during NPPV. A commercial single-line circuit, recommended by the manufacturer, was used and was connected to the nasal mask via a exhalation valve (Plateau Exhalation Valve, Respironics). No humidification or oxygen therapy was used during the study.
Measurements
Arterialized earlobe capillary blood gases were measured before the study during spontaneous breathing in room air [13]. Pulse oximetry (arterial oxygen saturation), respiratory rate, and heart rate were recorded continuously (Ultracap, Nellcorr Puritan-Bennett, Courtaboeuf, France).
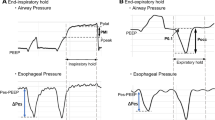
Airway pressure (Paw) was measured with a differential pressure transducer (MP 45 model, Validyne, Northridge, Calif., USA; ±100 cmH2O) on the mask (Fig. 1). Due to the increase in dead space that accompanied the insertion of a pneumotachograph circuit we were unable to measure flow. During the spontaneous breathing (SB) period the children could not tolerate the mask alone because of profound desaturations in all the patients, with arterial oxygen saturation nadir values of 75%.
Esophageal (Pes) and gastric (Pga) pressures were measured using a 2.1-mm external diameter catheter mounted pressure transducer system with two integrated pressure transducers (Gaeltec, Dunvegan, UK) inserted pernasally after careful local anesthesia (lidocaine 2%, Astra Zeneca, Rueil-Malmaison, France) [10, 14]. After calibration of the two pressure transducers using a 10-cm water column before each study the catheter was advanced gently until the distal tip was in the stomach and the proximal pressure transducer in the middle portion of the esophagus. Placement of the Pga transducer was checked by gentle manual pressure on the patient’s abdomen to observe fluctuations in Pga, which should be absent on the Pes trace. Placement of the Pes transducer was checked the presence of a negative deflection during inspiration. The validity of the Pes measurement was checked by a series of two or three “occlusion tests” as recommended by Baydur et al. [15], showing a ratio of ΔPes/Δmouth pressure close to the unity. In these infants these “occlusion tests” consisted of an occlusion of the nasal mask at end-expiration and allowing the child to perform a spontaneous occluded inspiratory effort. Transdiaphragmatic pressure (Pdi) was obtained by on line subtracting of the Pes signal from the Pga signal. All the signals were digitized at 128 Hz and sampled for analysis using an analogic/numeric acquisition system (MP 100, Biopac Systems, Goletta, Calif., USA), run on a PC computer (Elonex, Gennevilliers, France) with Acknowledge software.
Protocol
No sedation was administered. The procedure started with adjustment of CPAP ventilation to optimal level, followed by adjustment of BIPAP ventilation to optimal level. Thereafter, following a period of stabilization of at least 15 min, respiratory pattern with no NPPV was recorded for 5 min. Then CPAP and BIPAP ventilation were compared in a random order, with measurement of respiratory pattern for 5 min after a 15 min of stabilization. During CPAP the initial pressure level was set at 4 cmH2O. The pressure was progressively increased in 1 cmH2O increments and set at a level that was associated with the clinical disappearance of the stridor and snoring [11] and also the greatest fall in Pes and Pdi swings [10]. BIPAP was titrated with an expiratory pressure level corresponding to the optimal CPAP level, and an additional inspiratory pressure support of 4, 6, and 8 cmH2O. The inspiratory pressure thus represented the sum of the CPAP and the pressure support level. The highest pressure support level tolerated by the patient was used for comparison with CPAP ventilation. The sensitivity of the inspiratory and expiratory triggers (Digital Auto-Track Sensitivity with leak adaptation for the Synchrony) was fixed by the manufacturer and were not adjustable. The ventilators were set in the spontaneous mode, with no backup rate.
Data analysis
Respiratory rate and inspiratory time/total respiratory cycle time (Ti/Ttot) were calculated from the Pes trace. Pes and Pdi swings and the PTPes and PTPdi per breath and per minute were measured and calculated as previously described [10, 16, 17, 18]. In brief, the PTPes/breath was obtained by measuring the area under the Pes signal between the onset of the inspiration, defined as the point at which occurred the deflection on the Pes trace, and the end of the inspiration, defined as the peak of Pdi [19], except that it was not referred to the chest wall static recoil pressure-time relationship because of the impossibility to obtain accurate tidal volume measurements. The PTPdi/breath was obtained by measuring the area under the Pdi signal from the onset of its positive deflection to its return to baseline. Both PTPes and PTPdi are also expressed per minute by multiplying the pressure-time products per breaths by the breathing frequency (PTPes/min and PTPdi/min) [16].
The quality of the inspiratory trigger was evaluated on the Titrigger, which is the time delay between the onset of inspiratory effort (swing Pes) and the moment when the airway pressure exceeded the positive end expiratory pressure [20], and the Timusc, which is the time delay between the onset of inspiratory effort and the peak of Pdi [19]. The ratio of these two (Titrigger/Timusc) indicates the importance of the trigger delay with regard to the patient’s estimated neural inspiratory time. The respiratory effort required to trigger the ventilator was evaluated on the esophageal (PTPestrigger) and diaphragmatic pressure time product (PTPditrigger); this was defined as the area of the pressures curves below baseline during the inspiratory trigger time (Titrigger). The ratio PTPestrigger/PTPdi were used as markers of the respiratory effort required to trigger the ventilator with regard to the patient’s total respiratory effort. An ineffective triggering effort was defined as a decrease in Pes greater than 1 cmH2O, but without a subsequent increase in airway pressure delivered by the ventilator [21]. Quantification of ineffective trigger effort was expressed as a percentage of the number of asynchronized cycles per minute divided by the total number of patient cycles per minute [21].
After elimination of artifactual cycles corresponding to cough and esophageal spasms, at least 20 successive breaths were used to calculate the average values. Data are presented as median and range. The three conditions of SB, CPAP, and BIPAP ventilation were compared using the nonparametric Friedman test. When a significant difference was observed, pairwise comparisons were performed using Wilcoxon’s tests. A p value less than 0.05 was considered statistically significant.
Results
Breathing pattern and respiratory effort during spontaneous breathing
Breathing pattern during SB was characterized by a high respiratory rate (median 45, range 24–84) and high Ti/Ttot ratio (median 63%, range 35–86%). Respiratory effort was elevated, as shown by the increased Pes swings, Pdi swings, PTPes/min, and PTPdi/min (Table 2). Despite this increased work of breathing the patients were unable to maintain a normal gas exchange, as demonstrated by their low PaO2 (69 mmHg, 53–79) and high PaCO2 (54 mmHg, 43–73; Table 1). No correlation was observed between patient age, arterial blood gases, and indices of respiratory effort.
Breathing pattern and respiratory effort during CPAP and BIPAP ventilation
All patients tolerated both NPPV sessions. Levels of CPAP used ranged from 8 to 12 cmH2O (mean 11±2). CPAP ventilation resulted in a significant decrease in respiratory rate and Ti/Ttot (Table 2). In the overall group there was an approx. 75% reduction in all indices of respiratory effort during CPAP (Table 2). There were no correlation between optimal level of CPAP, patient age, cause of upper airway obstruction, or PTPes and PTPdi values during SB.
During BIPAP ventilation the mean level of additional inspiratory pressure support was 5±1 cmH2O (range 4–6). An improvement in breathing pattern and respiratory effort similar to that observed during CPAP ventilation was observed during BIPAP ventilation (Table 2). A tracing from patient no. 6 during BIPAP ventilation is shown on Fig. 2. Individual data of the PTPes/min and PTPdi/min of the ten patients during SB and the two modes are presented on Fig. 3. No difference was observed between the two ventilators, Harmony and Synchrony.
Tracing in patient no. 6 during bilevel positive airway pressure ventilation showing the patient ventilator asynchrony with inspiratory efforts not followed by a positive pressure support (thin arrows) and the continuation of the delivery of the positive airway pressure during the patient’s expiratory phase (thick arrows). Vertical dotted lines patient-ventilator asynchronized cycles. Pes esophageal pressure; Pgas gastric pressure, Paw airway pressure; Pdi transdiaphragmatic pressure
Patient-ventilator synchronization during BIPAP ventilation
Ineffective inspiratory efforts were observed during BIPAP ventilation in all the patients (Table 3). A great interpatient variability was observed, with the proportion of ineffective inspiratory efforts ranging from 32% to 97% (median 64%; Table 3). The analysis of the sensitivity of the inspiratory trigger revealed a long trigger delay with median ΔT of 300 ms, range 180–530 ms, and high median TItrigger/TImusc ratio of 65% (range 29–94%). This highlights the importance of the respiratory effort required to trigger the ventilator with a median PTPestrigger of 1.42 (0.36–6.25) and median PTPditrigger of 0.97 cmH2O.s (0.17–7.53). Furthermore, the median respiratory effort necessary to trigger the ventilator was 17% and 18% of the median PTPes/breath and PTPdi/breath, respectively. In addition, as observed in Fig. 2, expiratory trigger was inoperative in the majority of our patients. The difference between the PTPes and PTPdi during CPAP and BIPAP was not correlated with the percentage of ineffective respiratory efforts during BIPAP mode. Again, no difference was observed between the Harmony and Synchrony devices.
Discussion
This physiological study demonstrates that NPPV ventilation improves the breathing pattern and reduces the respiratory effort of very young infants with severe upper airway obstruction. CPAP ventilation remains the preferred mode rather than BIPAP, as the trigger of the domiciliary ventilators tested in the present study (BiPAP Harmony and BiPAP Synchrony) were insufficiently sensitive for these young infants.
CPAP ventilation adequately decreases respiratory effort
The findings of the present study are in agreement with those of previous studies in older children with obstructive sleep apnea demonstrating the efficacy of CPAP ventilation [8, 9, 11]. In the current study this ventilatory mode adequately unloaded the respiratory muscles and improved the ventilatory pattern of infants, all of whom were aged 18 months or under.
The limitations of BIPAP ventilation
BIPAP ventilation has been recommended for adult patients with obstructive sleep apnea not only to reduce the level of PEEP required but also to provide additional unloading of the respiratory muscles during inspiration, which could improve the efficacy and comfort of this ventilatory mode [12, 22]. Furthermore, it has been demonstrated that this mode is also useful in older children with laryngomalacia [10]. Because of the findings of these studies [10, 12, 22] and the requirement to reduce the high inspiratory muscle load observed in infants with upper airways obstruction we reasoned that the addition of positive pressure support during inspiration could be beneficial. However, in contrast to our original hypothesis, we observed that the inspiratory and expiratory trigger sensitivity of two devices tested was insufficient and resulted in patient-ventilator asynchrony. The BIPAP device has a fixed inspiratory and expiratory flow-trigger, and both bench studies and clinical studies have shown significant differences in the trigger sensitivity and performance of the various bilevel pressure devices [20, 23, 24]. The clinical impact of these ventilator characteristics vary between patients, with a significant impact on respiratory effort shown in some patients [20] but not in others [23]. These discrepancies may be explained by the different devices tested but also by the patient’s disease. A bench study showed that the performance of a home bilevel pressure ventilator decreased when the respiratory effort increased [24]. Furthermore, leaks can also affect the quality of the trigger [25]. In a test lung comparison Stell and coworkers [26] concluded that leaks would cause minor increases in the inspiratory trigger delays by slowing the decline in mask pressure.
It must be underlined that these studies were either bench studies or clinical studies performed in adult patients. However, the respiratory effort of these adult patients is far less important than those measured in the infants in the present study. Moreover, the breathing pattern of these infants was also different with a higher respiratory rate and a smaller tidal volume, which could promote patient-ventilator asynchrony. A fundamental characteristic of the present patient group is the existence of severe upper airway obstruction. Changes in intrathoracic pressure, as iniated during inspiration, could be poorly transmitted through the obstructed airway to the ventilatory circuit. It would thus be more logical to use a different mechanism of triggering, in particular Pes or Pdi, to initiate and terminate breath. A Pdi control of airway pressure support has been recently evaluated in healthy adults and was associated with a greater reduction in respiratory effort than a flow triggered pressure support [27]. The efficacy of BIPAP ventilation on the breathing pattern and respiratory effort in this short-term physiological study was probably not explained by the pressure support unloading effect but rather by the decrease in upper airway resistance induced by PEEP, as was similarly observed under the CPAP condition. However, the patient ventilator asynchrony observed during BIPAP ventilation explained the greater mean respiratory effort of the patients during this mode.
Limitations of the study
Although our study has a number of limitations, we feel that they do not detract from the results. The first limitation is that we were unable to measure airflow and thus cannot accurately report the onset and the end of the inspiration. This deficiency in experimental design was due to the increase in dead space during spontaneous breathing and the occurrence of high air flows during NPPV which disallows the measurement of the patient’s own airflow. The absence of flow measurements could also represent a limitation for the accurate evaluation of the quality of the triggers but the patient-ventilator asynchrony was so important (see Fig. 2) that we can reasonably expect that our conclusions would have been similar with a flow measurement.
Our study was a short-term physiological study performed during daytime. It is difficult to perform measurements of the work of breathing in infants during sleep because these measurements are relatively invasive. In addition, the Pes measuring device may interfere with sleep parameters. We noted, however, that all the infants fell asleep within a few minutes after the initiation of NPPV with the appropriate CPAP level. Nevertheless, because leaks generally increased during sleep [28], it is improbable that the patient-ventilator asynchrony observed during daytime can be improved during the night.
The tolerance of the custom-made nasal masks was excellent in this short-term study, but one of the major disadvantages of mask ventilation in growing individuals is the development of facial bones malformation [29]. Systematic pediatric maxillofacial evaluation prior to the initiation of NPPV and during follow-up is thus mandatory in these young children.
Although we deemed it unethical to subject these children to repetitive invasive measures arterial blood gas measurements during NPPV, we observed that the arterial blood gases normalized in all the patients within 1 week after starting NPPV.
This short term study shows that noninvasive CPAP and BIPAP ventilation are associated with a significant and comparable decrease in respiratory effort in infants with severe upper airway obstruction. BIPAP ventilation, however, was associated with patient-ventilator asynchrony with the domiciliary ventilators used in the present study. Long-term studies and the evaluation of devices with improved trigger systems are warranted to firmly recommend CPAP or BIPAP ventilation as the preferred ventilatory mode of these infants.
References
Rupa V, Raman R (1991) Aetiological profile of paediatric laryngeal stridor in an Indian hospital. Ann Trop Paediatr 11:137–141
Altman KW, Wetmore RF, Marsch RR (1997) Congenital abnormalities requiring tracheotomy: a profile of 56 patients and their diagnosis over a 9 year period. Int J Pediatr Otorhinolaryngol 41:199–206
Holinger LD (1980) Etiology of stridor in the neonate and child. Ann Otol Rhinol Laryngol 89:397–400
Lis G, Szczerbinski T, Cichocka-Jarosz E (1995) Congenital stridor. Pediatr Pulmonol 20:220–224
Altman KW, Wetmore RF, Marsch RR (1999) Congenital airway abnormalities in patients requiring hospitalisation. Arch Otolaryngol Head Neck Surg 125:525–528
McSwiney PF, Cavanagh NP, Languth P (1977) Outcome in congenital stridor (laryngomalacia). Arch Dis Child 52:215–218
Denoyelle F, Mondain M, Gresillon N, Roger G, Chaudré F, Garabédian EN (2003) Failures and complications of supraglottoplasty in children. Arch Otolaryngol Head Neck Surg 129:1077–1080
Guilleminault C, Pelayo R, Clerk A, Leger D, Boclan RC (1995) Home nasal continuous positive airway pressure in infants with sleep-disordered breathing. J Pediatr 127:905–912
Waters KA, Everett FM, Bruderer JW, Sullivan CE (1995) Obstructive sleep apnea: the use of nasal CPAP in 80 children. Am J Respir Crit Care Med 152:780–785
Fauroux B, Pigeot J, Polkey MI, Roger G, Boulé M, Clément A, Lofaso F (2001) Chronic stridor caused by laryngomalacia in children. Work of breathing and effects of noninvasive ventilatory assistance. Am J Respir Crit Care Med 164:1874–1878
Downey III R, Perkin RM, MacQuarrie J (2000) Nasal continuous positive airway pressure use in children with obstructive sleep apnea younger than 2 years of age. Chest 117:1608–1612
Sanders MH, Kern N (1990) Obstructive sleep apnea treated by independently adjusted inspiratory and expiratory positive airway pressures via nasal mask. Chest 98:317–324
Gaultier C, Boulé M, Allaire Y, Clément A, Burry A, Girard F (1978) Determination of capillary oxygen tension in infants and children: assessment of methodology and normal values during growth. Bull Euro Physiopathol Respir 14:287–294
Stell IM, Tompkins S, Lovell AT, Goldstone JC, Moxham J (1999) An in vivo comparison of a catheter mounted pressure transducer system with conventional balloon catheters. Eur Respir J 13:1158–1163
Baydur A, Behrakis PK, Zin WA, Jaeger MJ, Milic-Emili J (1982) A simple method for assessing the validity of the esophageal balloon technique. Am Rev Respir Dis 126:788–791
Sassoon CSH, Light RW, Lodia R, Sieck GC, Mahutte CK (1991) Pressure-time product during continuous positive airway pressure, pressure support ventilation and T-piece during weaning from mechanical ventilation. Am Rev Respir Dis 143:459–475
Field S, Sanci S, Grassino A (1984) Respiratory muscle oxygen consumption estimated by the diaphragm pressure-time index. J Appl Physiol 57:44–51
Barnard P, Levine S (1986) Critique on application of diaphragmatic time-tension index to spontaneously breathing humans. J Appl Physiol 60:1067–1072
Parthasarathy S, Jubran A, Tobin M (2000) Assessment of neural inspiratory time in ventilator-supported patients. Am J Respir Crit Care Med 162:546–552
Lofaso F, Brochard L, Hang T, Lorino H, Harf A, Isabey D (1996) Home versus intensive care pressure support devices. Experimental and clinical comparison. Am J Respir Crit Care Med 153:1591–1599
Parthasarathy S, Jubran A, Tobin MJ (1998) Cycling of inspiratory and expiratory muscle groups with the ventilator in airflow limitation. Am J Respir Crit Care Med 158:1471–1478
Vanpee D, El Khawand C, Rousseau L, Jamart J, Delaunois L (2002) Effects of nasal pressure support on ventilation and inspiratory work in normocapnic and hypercapnic patients with stable COPD. Chest 122:75–83
Vitacca M, Barbano L, D’Anna S, Porta R, Bianchi L, Ambrosino N (2002) Comparison of five bilevel pressure ventilators in patients with chronic ventilatory failure. Chest 122:2105–2114
Tassaux D, Strasser S, Fonseca S, Dalmas E, Jolliet P (2002) Comparative bench study of triggering, pressurization, and cycling between the home ventilator VPAP II and three ICU ventilators. Intensive Care Med 28:1254–1261
Calderini E, Confalonieri M, Puccio PG, Francavilla N, Stella L, Gregoretti C (1999) Patient-ventilator asynchrony during noninvasive ventilation: the role of the expiratory trigger. Intensive Care Med 25:622–667
Stell IM, Paul G, Lee KC, Ponte J, Moxham J (2001) Noninvasive ventilator triggering in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 164:2092–2097
Sharshar T, Desmarais G, Louis B, Macadou G, Porcher R, Harf A, Raphael JC, Isabey D, Lofaso F (2003) Transdiaphragmatic pressure control of airway pressure support in healthy subjects. Am J Respir Crit Care Med 168:760–769
Teschler H, Stampa J, Ragette R, Konietzko N, Berthon-Jones M (1999) Effect of mouth leak on effectiveness of nasal bilevel ventilatory assistance and sleep architecture. Eur Respir J 14:1251–1257
Fauroux B, Lavis JF, Nicot F, Picard A, Clément A, Vazquez MP (2004) Tolerance of nasal masks used for positive pressure ventilation in children. Eur Respir J 24:474S
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Essouri, S., Nicot, F., Clément, A. et al. Noninvasive positive pressure ventilation in infants with upper airway obstruction: comparison of continuous and bilevel positive pressure. Intensive Care Med 31, 574–580 (2005). https://doi.org/10.1007/s00134-005-2568-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2568-6