Abstract
Context
Substitute decision makers may consider the pre-morbid health status of their critically ill loved one when making treatment decisions on her/his behalf.
Objective
To compare estimates of pre-morbid health-related quality of life (HRQOL) obtained from survivors of the acute respiratory distress syndrome (ARDS) with those of their substitute decision makers using the Short Form 36 (SF-36).
Design
Prospective cohort study.
Setting
University-affiliated intensive care unit in Toronto, Canada.
Patients
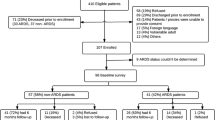
A sample of 46 ARDS survivors and their substitute decision makers drawn from a previously described cohort.
Interventions
We measured agreement and differences between responses on the SF-36 obtained from survivors (at 3 months after ICU discharge) and their substitute decision makers (at study entry).
Measurements and results
Agreement was poor for all SF-36 components and differences reached significance in three domains. In multivariable analysis considering age; sex; Acute Physiology, Age, and Chronic Health Evaluation II score; and Lung Injury Score, only patient age was associated with the mean difference between estimates for the ‘Mental Health’ domain. On average, estimates of pre-morbid HRQOL obtained from substitute decision makers were lower than those obtained from survivors.
Conclusion
Agreement between estimates of pre-morbid HRQOL provided by ARDS survivors and their substitute decision makers was poor. Compared with survivors, proxies tended to provide lower estimates of pre-morbid HRQOL. Substitute decision making for incapacitated patients is an imperfect process during which family members may underestimate their loved ones' own perception of pre-morbid health status. Alternatively, survivors of critical illness may overestimate pre-morbid HRQOL.
Similar content being viewed by others
References
Pickard AS, Knight SJ (2005) proxy evaluation of health-related quality of life: a conceptual framework for understanding multiple proxy perspectives. Med Care 43:493–499
Yip JY, Wilber KH, Myrtle RC, Grazman DN (2001) comparison of older adult subject and proxy responses on the SF-36 health-related quality of life instrument. Aging Ment Health 5:136–142
Rebollo P, Alvarez-Ude F, Valdes C, Estebanez C (2004) Different evaluations of the health related quality of life in dialysis patients. J Nephrol 17:833–840
Andresen EM, Vahle VJ, Lollar D (2001) Proxy reliability: health-related quality of life (HRQoL) measures for people with disability. Qual Life Res 10:609–619
Pierre U, Wood-Dauphinee S, Korner-Bitensky N, Gayton D, Hanley J (1998) Proxy use of the Canadian SF-36 in rating health status of the disabled elderly. J Clin Epidemiol 51:983–990
Rogers J, Ridley S, Chrispin P, Scotton H, Lloyd D (1997) Reliability of the next of kin's estimates of critically ill patients' quality of life. Anaesthesia 52:1137–1143
Capuzzo M, Grasselli C, Carrer S, Gritti G, Alvisi R (2000) Quality of life before intensive care admission: agreement between patient and relative assessment. Intensive Care Med 26:1288–1295
Hofhuis J, Hautvast JL, Schrijvers AJ, Bakker J (2003) Quality of life on admission to the intensive care: can we query the relatives? Intensive Care Med 29:974–979
Elliott D, Lazarus R, Leeder SR (2006) Proxy respondents reliably assessed the quality of life of elective cardiac surgery patients. J Clin Epidemiol 59:153–159
Graf J, Koch M, Dujardin R, Kersten A, Janssens U (2003) Health-related quality of life before, 1 month after, and 9 months after intensive care in medical cardiovascular and pulmonary patients. Crit Care Med 31:2163–2169
Graf J, Wagner J, Graf C, Koch KC, Janssens U (2005) Five-year survival, quality of life, and individual costs of 303 consecutive medical intensive care patients – a cost-utility analysis. Crit Care Med 33:547–555
Schelling G, Stoll C, Haller M, Briegel J, Manert W, Hummel T, Lenhart A, Heyduck M, Polasek J, Meier M, Preuss U, Bullinger M, Schuffel W, Peter K (1998) Health-related quality of life and posttraumatic stress disorder in survivors of the acute respiratory distress syndrome. Crit Care Med 26:651–659
Schelling G, Stoll C, Vogelmeier C, Hummel T, Behr J, Kapfhammer HP, Rothenhausler HB, Haller M, Durst K, Krauseneck T, Briegel J (2000) Pulmonary function and health-related quality of life in a sample of long-term survivors of the acute respiratory distress syndrome. Intensive Care Med 26:1304–1311
Welsh CH, Thompson K, Long-Krug S (1999) Evaluation of patient-perceived health status using the Medical Outcomes Survey Short-Form 36 in an intensive care unit population. Crit Care Med 27:1466–1471
Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al Saidi F, Cooper AB, Guest CB, Mazer CD, Mehta S, Stewart TE, Barr A, Cook D, Slutsky AS (2003) One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med 348:683–693
Heyland DK, Groll D, Caeser M. Survivors (2005) of Acute Respiratory distress syndrome: relationship between pulmonary dysfunction and long-term health-related quality of life. Crit Care Med 33:1549–1556
Orwelius L, Nordlund A, Edell-Gustafsson U, Simonsson E, Nordlund P, Kristenson M, Bendtsen P, Sjoberg F (2005) Role of preexisting disease in patients' perceptions of health-related quality of life after intensive care. Crit Care Med 33:1557–1564
Scales DC, Tansey CM, Matte-Martyn A, Herridge MS (2005) Difference in reported pre-morbid health-related quality of life (HRQOL) in ARDS survivors compared to their surrogate decision-maker (SDM). Proc Am Thor Soc 2 (abstract issue)
McHorney CA, Ware JE Jr, Lu JF, Sherbourne CD (1994) The MOS 36-item Short-Form Health Survey (SF-36). III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care 32:40–66
Ware JE Jr, Snow KK, Kosinski M, Gandek B (1993) SF-36 Health Survey manual & interpretation guide. The Health Institute, New England Medical Center, Boston, MA
Ware JE Jr, Kosinski M, Keller SD (1994) SF-36 physical and mental health summary scales: a user's manual. Health Assessment Lab, Boston, MA
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Murray JF, Matthay MA, Luce JM, Flick MR (1988) An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis 138:720–723
Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ (1995) Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med 23:1638–1652
Fleis JL (2004) Statistical methods for rates and proportions, 2nd edn. Wiley, New York
Cohen J (1960) A coefficient of agreement for nominal scales. Educ Psychol Measurement 20:37–46
Cohen J (1968) Weighted Kappa: nominal scale agreement with provision for scaled disagreement of partial credit. Psychol Bull 70:213–220
Walters SJ, Campbell MJ, Lall R (2001) Design and analysis of trials with quality of life as an outcome: a practical guide. J Biopharm Stat 11:155–176
Walters SJ (2004) Sample size and power estimation for studies with health related quality of life outcomes: a comparison of four methods using the SF-36. Health Qual Life Outcomes 2:26
Cicchetti DV, Allison T (1971) A new procedure for assessing reliability of scoring EEG sleep recordings. Am J EEG Technol 11:101–109
Shrout PE, Fleis JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86:420–428
Altman DG (1991) Practical statistics for medical research. Chapman and Hall, London
Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, Stern EJ, Hudson LD (2005) Incidence and outcomes of acute lung injury. N Engl J Med 353:1685–1693
Shalowitz DI, Garrett-Mayer E, Wendler D (2006) The accuracy of surrogate decision makers: a systematic review. Arch Intern Med 166:493–497
Weinfurt KP, Trucco SM, Willke RJ, Schulman KA (2002) Measuring agreement between patient and proxy responses to multidimensional health-related quality-of-life measures in clinical trials. An application of psychometric profile analysis. J Clin Epidemiol 55:608–618
Cohen S, Sprung C, Sjokvist P, Lippert A, Ricou B, Baras M, Hovilehto S, Maia P, Phelan D, Reinhart K, Werdan K, Bulow HH, Woodcock T (2005) Communication of end-of-life decisions in European intensive care units. Intensive Care Med 31:1215–1221
Andrews P, Azoulay E, Antonelli M, Brochard L, Brun-Buisson C, Dobb G, Fagon JY, Gerlach H, Groeneveld J, Mancebo J, Metnitz P, Nava S, Pugin J, Pinsky M, Radermacher P, Richard C, Tasker R (2006) Year in review in intensive care medicine, 2005. II. Infection and sepsis, ventilator-associated pneumonia, ethics, haematology and haemostasis, ICU organisation and scoring, brain injury. Intensive Care Med 32:380–390
Arnold RM, Kellum J (2003) Moral justifications for surrogate decision making in the intensive care unit: implications and limitations. Crit Care Med 31:S347–S353
Azoulay E, Pochard F, Chevret S, Adrie C, Bollaert PE, Brun F, Dreyfuss D, Garrouste-Org Goldgran-Toledano D, Jourdain M, Wolff M, Le Gall JR, Schlemmer B (2003) Opinions about surrogate designation: a population survey in France. Crit Care Med 31:1711–1714
Booth MG, Doherty P, Fairgrieve R, Kinsella J (2004) Relatives' knowledge of decision making in intensive care. J Med Ethics 30:459–461
Hopman WM, Towheed T, Anastassiades T, Tenenhouse A, Poliquin S, Berger C, Joseph L, Brown JP, Murray TM, Adachi JD, Hanley DA, Papadimitropoulos E (2000) Canadian normative data for the SF-36 Health Survey. Canadian Multicentre Osteoporosis Study Research Group. CMAJ 163:265–271
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: http://dx.doi.org/10.1007/s00134-006-334-z
Rights and permissions
About this article
Cite this article
Scales, D.C., Tansey, C.M., Matte, A. et al. Difference in reported pre-morbid health-related quality of life between ARDS survivors and their substitute decision makers. Intensive Care Med 32, 1826–1831 (2006). https://doi.org/10.1007/s00134-006-0333-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0333-0