Abstract
During recent years, a rising incidence of invasive pulmonary aspergillosis (IPA) in non-neutropenic critically ill patients has been reported. Critically ill patients are prone to develop disturbances in immunoregulation during their stay in the ICU, which render them more vulnerable for fungal infections. Risk factors such as chronic obstructive pulmonary disease (COPD), prolonged use of steroids, advanced liver disease, chronic renal replacement therapy, near-drowning and diabetes mellitus have been described. Diagnosis of IPA may be difficult and obtaining histo- or cytopathological demonstration of the fungus in order to meet the gold standard for IPA is not always feasible in these patients. Laboratory markers used as a non-invasive diagnostic tool, such as the galactomannan antigen test (GM), 1,3-β-glucan, and Aspergillus PCR, show varying results. Antifungal therapy might be considered in patients with persistent pulmonary infection who exhibit risk factors together with positive cultures or sequentially positive GM and Aspergillus PCR in serum, in whom voriconazole is the drug of choice. The benefit of combination antifungal therapy lacks sufficient evidence so far, but this treatment might be considered in patients with breakthrough infections or refractory disease.
Similar content being viewed by others
Introduction
Invasive pulmonary aspergillosis (IPA) has emerged as an important cause of morbidity and mortality in patients receiving intensive chemotherapy, allogeneic stem cell transplantation, and solid organ transplantation. However, during recent years, several reports have described a rising incidence of IPA in critically ill patients admitted to the intensive care unit (ICU), even in the absence of an apparent predisposing immunodeficiency [1–6]. The incidence of IPA in the ICU ranges from 0.3% to as much as 5.8% [2, 3, 6] and it carries an overall mortality rate exceeding 80%, with an attributable mortality ofalmost 20% [4, 5]. This high mortality is at least partially related to difficulties in timely diagnosis, caused by insensitive and non-specific clinical signs and lack of unequivocal diagnostic criteria.
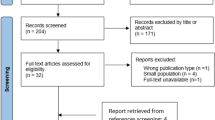
In this review, we will describe the pathophysiological mechanisms and risk factors for IPA in non-neutropenic critically ill patients, limitations and advances in the diagnostic process, and alterations in treatment with antifungal therapy. A Medline/PubMed search was performed for all articles about IPA in critically ill patients in relation to risk factors, diagnosis and antifungal therapy. All publication types of human studies in the English language were searched and an extraction of relevant articles was made for the purpose of this narrative review.
Pathophysiological mechanisms and risk factors
Aspergillus spp. are opportunistic moulds that cause both allergic and invasive syndromes. The genus Aspergillus contains approximately 175 species, only a minority of them have been associated with human disease. Infections are caused mostly by Aspergillus fumigatus; next in line are Aspergillus flavus, Aspergillus terreus, Aspergillus niger andAspergillus nidulans [7]. Aspergillus is found in soil, water, food, and in the air and grows on a wide variety of organic material, such as decaying vegetation. The conidia (spores) are easily aerosolised. The route of transmission is by air. Although exposure is universal, invasive infection occurs almost exclusively in immunocompromised individuals. Infections have frequently been described in patients with haematological malignancies and solid organ transplant recipients, but also in patients undergoing chronic intermittent haemodialysis in whom these infections were associated with hospital construction and/or ventilation systems contaminated with Aspergillus spp. [8]. Even hospital water is a frequently overlooked source of nosocomial aspergillosis [9, 10].
Natural antifungal defence in humans is based on normal mucosal barriers and an intact macrophage and neutrophil function. Alveolar macrophages form the first line of defence against inhaled Aspergillus conidia that reach the alveoli. Macrophages normally are capable of killing the conidia and preventing germination, by releasing cytokines such as tumour necrosis factor (TNF)-α and macrophage inflammatory protein (MIP)-1α [11]. During neutropenia, TNF-α and MIP-1α synthesis is reduced and the conidia can germinate to form hyphae. T-cell mediated acquired immunity also has an important role in protecting against fungal infections, as Aspergillus antigens are able to induce T-helper (Th)-1 and Th-2 type reactivity [12, 13]. Th-1 reactivity is displayed by an increase of interferon-γ and interleukin (IL)-12 and has protective effects against infection. In contrast, Th-2 reactivity is characterised by production of IL-4 and IL-10 and leads to disease progression, at least in a murine model of IPA [12, 14, 15].
Critically ill patients in ICU exhibit a complex change in immune function characterised by deactivation of macrophages and an altered cellular response due to the severity of illness which is also termed “immunoparalysis” [16, 17]. This immunologic derangement might explain why Aspergillus infections are able to develop in critically ill patients who do not display the predisposing classical risk factors [17, 18]. Many other factors will negatively influence the immune function during critical illness, such as (acute) hyperglycaemia [19] and the use of corticosteroids [20–23]. Corticosteroids have profound effects on the distribution and function of neutrophils, monocytes, and lymphocytes and they directly stimulate the growth of Aspergillus fumigatus in vitro possibly via sterol binding proteins in the fungus [21]. In particular intravenous corticosteroids treatment in patients with chronic obstructive pulmonary disease (COPD), is associated with a rising incidence of IPA [1, 24–26]. Also broad-spectrum antibiotics, which affect the distribution of normal flora, have been described as a risk factor [27]. However, not every critically ill patient in the ICU is at risk for developing invasive fungal infections. Apparently, other specific – patient-related – predisposing conditions seem to be associated with the development of IPA, in which COPD and other chronic lung disease [1–4, 28–32], diabetes mellitus [2, 31, 33], acute liver failure/advanced liver cirrhosis [2–4, 34], chronic renal failure [8, 35], and near drowning [4, 36–38] have been described (Table 1). In these, mainly retrospective, studies a mean in-hospital mortality of 80% was found in patients with highly suspected or proven IPA in the presence of at least one of these underlying conditions, despite antifungal therapy. Remarkably, patients who were suspected to be colonised only with Aspergillus spp. (i. e. no signs of pulmonary infection) demonstrated even a high in-hospital mortality rate [3, 31], which might suggest that colonisation should be considered as a potentially important finding.
Diagnostic features
A few years ago, a consensus for standard definitions and diagnosis for invasive fungal infections in immunocompromised patients with cancer and recipients of haematopoietic stem cell transplants was established by the European Organization for Research and Treatment of Cancer and the Mycoses Study Group (EORTC/MSG) in which three levels of probability for invasive fungal infections are proposed: “proven”, “probable” and “possible” [39]. However, these guidelines are intended for use in clinical trials and for epidemiologic research and, moreover, are focused on patients with classical risk factors such as neutropenia, malignancies and after haematopoietic stem cell transplantation, and it may not be possible to extrapolate them to the non-neutropenic critically ill patient.
The diagnosis of IPA in non-neutropenic critically ill patients is difficult because signs and symptoms are non-specific, and the initiation of additional diagnostic examinations is often delayed because of a low clinical suspicion. For the timing of suspicion of IPA in these patients, the combination of persistent or rapid developing infiltrative abnormalities on thoracic imaging and/or a persistent pulmonary infection despite broad spectrum antibiotics accompanied by one or more predisposing conditions (Table 1) might be the moment for triggering further diagnostic exploration. Although histopathological evidence of IPA is defined as the gold standard due to a very high tropism for blood vessels [39], trans-bronchial biopsy or surgical lung biopsy via mini-thoracotomy may not justify the risk of this invasive procedure in critically ill patients on mechanical ventilation with, sometimes, severe bleeding diathesis. Therefore, the diagnostic process will contain thoracic imaging and microbiological examination by means of direct microscopy and culture of sputum or broncho-alveolar lavage fluid (BALF). Excluding the possibility of contamination during the pre-analytical phase of a sample, isolation of Aspergillus spp. in the respiratory tract may represent three clinical situations: (1) evidence of current disease, (2) true colonisation, or (3) a marker for the future development of invasive disease. In the immunocompetent host, cultures of Aspergillus in respiratory secretions are usually a result of colonisation [32]; in the immunocompromised host, however, they may indicate invasive disease [6, 7, 39]. The positive predictive value of cultures in general is as high as 80–90% [2, 6, 40], although in some groups of patients (e. g. after lung transplantation) specificity is much lower [41]. Sensitivity of cultures in the diagnosis of IPA is poor [2, 6, 40]. Direct microscopic examination of sputum or BAL, stained with specific fluorescent stain for chitin (a fungal cell wall component) is easy to perform, rapid to read, and improves the sensitivity of microbiological examination [40, 42]. Direct visualisation of the hyphae makes it possible to discriminate between septate (e. g. Aspergillus, Fusarium and Scedosporium) and non-septate (e. g. Mucorales) moulds. Ubiquitous moulds of the order Mucorales cause serious infection in immunocompromised patients and, in contrast to Aspergillus, Fusarium and Scedosporium spp., they are not susceptible to voriconazole, which is an important factor when choosing a pre-emptive antifungal drug. The extra value of a positive culture is that growing of the fungus enables identification and susceptibility testing to antifungal drugs. This is important in view of the antifungal resistance of – for example – Aspergillus fumigatus isolates to voriconazole [43]. Nonetheless, reliance on microscopy and/or culture alone results in substantial underdiagnosis due to the low sensitivity. Fibre-bronchoscopy with inspection of the tracheobronchial tree, sampling of deep airway secretions and BAL can be helpful; the macroscopic finding of ulcerative lesions and/or pseudomembranes together with a positive microscopy and/or culture is highly suggestive for Aspergillus-related tracheobronchitis.
Chest computerised tomography (CT) has proved to be an important tool for the diagnosis of IPA in neutropenic, severely immunocompromised patients, even in the absence of evident lesions on a conventional chest X-ray. Radiological findings might include nodules with rapid growth and/or cavitations. A `halo sign' (a pulmonary mass surrounded by a zone of lower attenuation with ground-glass opacification produced by adjacent haemorrhage) and/or the `air crescent sign' (crescentic radiolucencies around a nodular area of consolidation) may be present [44–50]. The frequency of the halo sign in patients with IPA is relatively high in the early stages of the disease, but becomes progressively lower with the passage of time [51]. Combining the halo sign and the air crescent sign, the sensitivity for IPA is more than 80% as specificity reaches 60–98% [47]. However, thoracic imaging in mechanically ventilated ICU patients is less helpful due to many confounding factors such as atelectasis and, sometimes major, pleural effusions. A lower sensitivity (5–24%) of the halo sign and air crescent sign in non-neutropenic patients has been reported in the literature [3, 6, 52]. Due to the high tropism for blood vessels, IPA might be complicated by localisations in the central nervous system. Therefore, in patients with documented or highly suspected IPA, CT scanning or magnetic resonance imaging (MRI) of the brain should be considered to exclude dissemination to the brain.
In the past decade, non-invasive diagnostic tests, serological and molecular, have focused on the detection of surrogate markers for Aspergillus spp., such as the galactomannan (GM) antigen, 1,3-β-glucan and the detection of Aspergillus DNA by PCR. GM is a major Aspergillus cell-wall component that is released during the growth phase of the fungus, and detection of GM would be indicative for invasive disease [53]. Many studies have been done in order to investigate the value of the commercial Platelia Aspergillus assay (BioRad™, Marnes-La-Coquette, France) as a diagnostic tool for IPA, but mainly in patients with haematological malignancies [54–57]. The specificity of the GM assay for diagnosing IPA is at least 85%, as demonstrated by these studies, but the sensitivity of the assay varied considerably between 29% and 100% depending on the cut-off value. The most important finding of these studies was that in around two-third of patients, circulating antigen could be detected at a mean of 8 days before a probable diagnosis was made by a combination of radiographic findings and Aspergillus isolation [53, 54]. In a recent meta-analysis, 27 studies were included regarding the value of the GM serum assay for surveillance of IPA in high-risk patients. The median sensitivity for proven cases was 71% (specificity 89%); for proven or probable cases, median sensitivity and specificity were 61% and 93%, respectively [58]. Specificity increased to 95% using a cut-off value of 1.5 in cases with proven or probable IPA. Because GM is a water-soluble carbohydrate, it can also be detected in BALF. Although the Platelia ELISA (enzyme-linked immunosorbent assay) is not validated for detection of GM in this fluid, there is an increasing tendency to use these samples for diagnosis of IPA. In small clinical studies among patients with haematological malignancies and in solid organ transplant recipients, the sensitivity of the GM EIA (enzyme immuno-assay) applied to BALF ranges from 85% to 100% with a high index cut-off (> 1.5) to define positivity [59–62]. However, there are several clinical circumstances that might influence the diagnostic performance of the GM antigen test in either serum or BALF. First, the false-positive reactivity which might be caused by gastro-intestinal translocation of fungal GM from contaminated food or drink, as demonstrated in small children [63], and the use of the intravenous antibiotics piperacillin–tazobactam and amoxicillin–clavulanic acid, which is associated with serum ELISA reactivity in patients without evidence of IPA [64–67]. Second, an important factor that affects the release of GM antigens is antifungal drug therapy. Different animal and human studies have shown decreased sensitivity of the GM assay when (prophylactic) antifungal drugs were used [63, 68, 69]. In several prospective studies that assessed the performance of antigen detection, patients received antifungal prophylaxis with itraconazole, which might have a significant effect on the sensitivity of the assay [53, 54]. Third, when the Platelia Aspergillus ELISA kit was launched in Europe about a decade ago, another cut-off serum ratio was recommended than at present. Over the past years, several studies suggested lower cut-off values, ranging from 0.5 to 1 [39, 53, 54, 70–72]. It is clear that alterations in cut-off level will change the performance of the assay. Finally, the studies show that monitoring GM levels is crucial in order to diagnose (and eventually monitor treatment outcome) correctly, which means that the assay has to be performed twice weekly, preferably on receipt of the specimen. In critically ill patients without classical risk factors for IPA, the diagnostic value of the GM assay has been investigated only in one retrospective study and demonstrated a sensitivity of only 53% in patients with proven or probable IPA (cut-off value 1.0) [3]. Thus, it has to be stressed that the available data from patients with (haematological) malignancies and after solid organ transplantation can not be extrapolated to the critically ill patient in general. In the meantime, due to lack of more reliable, non-invasive diagnostic tests, the GM assay could be used as an additive tool in the diagnostic work-up of IPA.
The 1,3-β-glucan is a cell wall component of many filamentous fungi and yeasts, including Aspergillus spp. and Candida spp. Reproducible assay results, with high specificity and a high positive predictive value, demonstrated that use of an assay to detect serum 1,3-β-glucan derived from fungal cell walls is a useful diagnostic adjunct for invasive fungal infection [73]. In addition, false-positive tests have been found in patients after haemodialysis, cardiopulmonary bypass surgery, high-dose immunoglobulin treatment, and after exposure to glucan-containing gauze [33]. Furthermore, in a recent small prospective study among ICU patients, serum glucan levels did not appear to be specific for fungal infections, as serum glucan levels were also elevated in bacterial infections [74]. Hence, the usefulness of 1,3-β-glucan in the diagnosis of IPA has to be further evaluated.
Amplification of nucleic acid by PCR technology for the diagnosis of IPA is being increasingly studied. It can be applied to serum and BAL specimens [75–79]. Experience is limited to patients with haematological malignancies. White et al. evaluated the performance of a real-time PCR in whole blood in a group of patients with haematological malignancies and showed sensitivity of 92.3% and specificity of 94.6% for the diagnosis of IPA with good agreement of the GM ELISA [80]. They concluded that a negative PCR obtained twice weekly allowed a wait-and-see approach concerning starting antifungal treatment. However, comparable to the GM antigen test, there are a number of factors that potentially have an impact upon the clinical sensitivity of PCR. The magnitude of the quantitative PCR signal falls with antifungal therapy, thereby causing false-negative PCR results [81] while the (transient) colonising presence of Aspergillus in the respiratory tract may suggest a low positive predictive value [78]. Furthermore, patients at risk for IPA are often prescribed a multitude of drugs and fluids, all of which may act as non-specific inhibitors of the PCR. For example, anticoagulants inhibit PCR, thereby limiting its sensitivity [82].
One might conclude that the use of GM antigen test, 1,3-β-glucan, and Aspergillus PCR as serological and molecular markers cannot be advocated for routine use in critically ill patients, and caution is warranted in the interpretation of positive test results in patients without a clinical suspicion of pulmonary infection as well as negative test results in patients with persisting pneumonia. However, the finding of sequentially positive GM tests in serum or BALF – using higher cut-off values – together with a positive Aspergillus PCR, in a patient with persisting pulmonary infection who carries one or more risk factors, is highly indicative for IPA and might justify treatment with antifungal therapy.
Antifungal therapy
There have been important developments in antifungal drugs in the past few years, although amphotericin B deoxycholate has been the standard therapy for IPA for decades. However, multiple studies have now established not only its lack of efficacy due to an increasing antifungal resistance but also demonstrated unacceptable toxicity of this compound, in particular nephrotoxicity [83, 84]. Continuous infusion of amphotericin B deoxycholate over 24 h may reduce its nephrotoxicity [85, 86], although the efficacy may be reduced due to lower peak serum levels [87]. The use of lipid formulations may also reduce toxicity and have been studied extensively for empirical use in febrile neutropenia with the same efficacy rate as conventional amphotericin B [88]. However, lipid formulations are more expensive, and the initial use of higher doses does not improve efficacy and is associated with greater toxicity than lower doses, which suggests that high doses may not be routinely warranted.
Among the triazoles, itraconazole has activity against Aspergillus, but its clinical utility in critically ill patients with IPA has been limited by drug interactions and toxicity as well as erratic bioavailability of the oral suspensions [89]. Furthermore, strains of Aspergillus fumigatus resistant to itraconazole have already been described [90]. A large multicentre randomised trial established that voriconazole provides higher response rates and better survival than amphotericin B in the treatment of “probable or proven” IPA among patients with haematological diseases with fewer drug-related adverse events [91]. As a result of this study, voriconazole is increasingly recommended as initial therapy for IPA [92]. Voriconazole is available for intravenous and oral use. It is rapidly absorbed within 2 h after oral administration and the oral bioavailability is over 90% [93]. Clearance is hepatic via N-oxidation by the hepatic cytochrome P450 (CYP) isoenzymes, CYP2C19, CYP2C9 and CYP3A4 [93], which makes the potential for drug interactions considerable. For instance, voriconazole considerably reduces the clearance of intravenous midazolam [94], and fatal interactions with highly active antiretroviral therapy (HAART) have been described [95]. As voriconazole has limited aqueous solubility, the intravenous form includes the solvent vehicle sulfobutylether beta cyclodextrin sodium [96]. The clearance of sulfobutylether beta cyclodextrin sodium is linearly related to creatinine clearance and accumulation has been described in subjects with moderate to severe renal impairment [96], although in animal experiments the frequency of acute toxicity of sulfobutylether beta cyclodextrin sodium is low. Target organs for toxic effects are the kidney and liver, causing obstruction of renal tubules and necrosis in the liver respectively [96]. Because of this potential toxicity, it is recommended to treat patients with moderate to severe renal failure and who are on renal replacement therapy only with the oral form of voriconazole, if feasible. However, in critically ill patients safe oral administration of drugs is difficult to accomplish as, for instance, gastric reflux, gastro-intestinal bleeding and impaired function of the intestine are frequent co-morbidities, leading to potentially insufficient intestinal absorption of the drug. Furthermore, it is important to recognise that some patients may have inadequate levels of the oral drug, particularly if a standard dose of 200 mg twice daily is used rather than the recommended 4 mg/kg twice daily dose which has been studied for the intravenous formulation [97]. At present, no clinical data are available regarding the bioavailability of the oral form of voriconazole in critically ill patients. It might be considered that the fear of potential adverse effects from intravenous solutions does not justify the risk of insufficient treatment by oral solutions. Moreover, limited clinical data showed no obvious toxicity in patients undergoing intermittent haemodialysis who were treated with daily 400–800 mg of intravenous voriconazole during 2 weeks [96], and the pharmacokinetics of voriconazole appears not to be affected by continuous renal replacement therapy (CRRT). On the basis of pharmacokinetics, dose reduction is not recommended in patients receiving CRRT [98, 99]. Regarding the efficacy of voriconazole, there is a potential concern with (long-term) voriconazole therapy as occasional breakthrough infections with yeasts and moulds, with decreased susceptibility to voriconazole, have been reported [43, 100, 101].
Posaconazole is a promising new triazole with broad-spectrum antifungal profile and has shown activity for salvage treatment of IPA in patients who are refractory to or intolerant of conventional therapy. A recent multicentre, prospective study among haematological and non-neutropenic patients with refractory IPA demonstrated a 42% overall success rate for posaconazole recipients versus 26% for control subjects [102]. Posaconazole is, however, only available for oral administration, which makes it probably less applicable in critically ill patients who are susceptible to impaired drug absorption in the digestive tract.
Echinocandins are a novel class of parenterally administered semi-synthetic lipopeptides with a pathogen-specific mechanism for non-competitive inhibition of biosynthesis of the fungus cell-wall enzyme complex 1,3-β-D-glucan [103]. The echinocandins have documented in vivo activity against Candida spp. and Aspergillus spp. At present, there are three approved echinocandins, caspofungin, anidulafungin and micafungin, of which particularly caspofungin has demonstrated efficacy for the treatment of IPA. The first clinical trial to document the efficacy of caspofungin was among patients with “proven or probable” IPA who had treatment failure with (liposomal) amphotericin B, itraconazole or voriconazole, or who were intolerant to these antifungal drugs [104]. Caspofungin seems to be as effective as and generally better tolerated than liposomal amphotericin B when given as empirical antifungal therapy in patients with persistent fever and neutropenia [105]. However, prospective randomised clinical trials aimed at the treatment of IPA in (non-neutropenic) critically ill patients are lacking.
In general, there is no conclusive evidence that extended-spectrum triazoles are superior to echinocandins or polyenes, or vice versa, for monotherapy of IPA in ICU patients. We need prospective randomised controlled trials to solve this issue in critically ill patients. Table 2 gives an overview of treatment options with antifungal drugs for IPA.
Combination therapy
Because the efficacy of antifungal therapy for IPA is poor, with more than 50% of all patients experiencing failure of first-line therapies [106, 107] empirical administration of combination antifungal regiments for proven or probable IPA may be an important strategy to improve outcome.
Theoretically, there are several foreseeable advantages of combination therapy, such as a widened spectrum and potency of drug reactivity, more rapid antifungal effect, synergy, and a reduced risk of antifungal resistance [108]. The available antifungal drugs target four different cell functions: cell membrane integrity (polyenes), ergosterol biosynthesis (azoles, allylamines), DNA synthesis (pyrimidine analogues) and cell-wall integrity (echinocandins). Although antifungal drugs are targeted against specific cell functions, many drugs also have pleiotropic effects that may inhibit other elements of fungal homeostasis [108]. For instance, azoles inhibit many cytochrome-dependent enzymes of the fungal respiration chain and amphotericin B generates oxidative species that damage fungal mitochondrial function and enhance macrophage fungal killing [109]. These subtle effects could be enhanced when one antifungal is applied together with a second drug, resulting in synergy. Conversely, the combination could act antagonistically, e. g. when one antifungal agent affects the targets of the other one.
Only a few clinical studies with small numbers of patients have tried to address the need for combination antifungal therapy [110–113] . These studies have important limitations because they lack a control group and because of many other uncontrolled factors including the choice of combination, the duration of therapy, concomitant antibacterial or antiviral treatment, the lack of adequate follow-up to estimate relapses, and no discrimination between primary and sequential therapy. Results from those studies should therefore be viewed with caution. Large, adequately powered, prospective clinical trials are needed but they might be difficult to perform because of inadequate enrolment, differences in providing benefits, difficulty in documenting fungal infection, controversy regarding endpoints, the lack of surrogate markers to correlate in-vitro evidence to outcome prognosis, and the associated costs [114]. Nevertheless, combination antifungal therapy might be considered for certain clinical conditions such as refractory disease or breakthrough infections [115, 116].
Conclusion
Recent data indicate that IPA may be an underestimated opportunistic fungal infection in critically ill patients, even in the absence of severe pre-existent immunological disorders, and carries a high mortality rate. A decrease in immune function or dysregulation of the immune system due to the severity of illness, together with specific underlying risk factors such as COPD, diabetes mellitus, chronic renal replacement therapy, advanced liver disease, and long-term use of steroids, might explain the relatively high occurrence of IPA among these patients. The high mortality rate is partially related to difficulties in timely diagnosis because of non-specific signs and symptoms, low clinical suspicion, and time delay due to high risks for invasive procedures to obtain histopathological evidence for diagnosing IPA. The presence of a persistent pulmonary infection despite broad-spectrum antibiotics or abnormal thoracic imaging by CT scanning together with one of these risk factors should trigger further diagnostic exploration by collecting respiratory secretions and/or laboratory markers. Meeting the gold standard alone should not be the threshold for starting antifungal therapy, considering the high mortality rate. Invasive infection in patients with negative cultures might be supported by positive serological and molecular markers such as galactomannan antigen testing and Aspergillus PCR, which requires at least two sequentially positive samples. Antifungal therapy might be considered when persistent pneumonia with positive cultures for Aspergillus spp. or sequentially positive GM and Aspergillus PCR are present, accompanied with one of those risk factors for which voriconazole appears to be the first-line treatment. Combination therapy might be considered in breakthrough infections with moulds or yeasts or in refractory disease, although clear evidence is lacking.
References
Bulpa PA, Dive AM, Garrino MG, Delos MA, Gonzalez MR, Evrard PA, Glupczynski Y, Installe EJ (2001) Chronic obstructive pulmonary disease patients with invasive pulmonary aspergillosis: benefits of intensive care? Intensive Care Med 27:59–67
Garnacho-Montero J, Amaya-Villar R, Ortiz-Leyba C, Leon C, Alvarez-Lerma F, Nolla-Salas J, Iruretagoyena JR, Barcenilla F (2005) Isolation of Aspergillus spp. from the respiratory tract in critically ill patients: risk factors, clinical presentation and outcome. Crit Care 9:R191–R199
Meersseman W, Vandecasteele SJ, Wilmer A, Verbeken E, Peetermans WE, Van WE (2004) Invasive aspergillosis in critically ill patients without malignancy. Am J Respir Crit Care Med 170:621–625
Vandewoude K, Blot S, Benoit D, Depuydt P, Vogelaers D, Colardyn F (2004) Invasive aspergillosis in critically ill patients: analysis of risk factors for acquisition and mortality. Acta Clin Belg 59:251–257
Vandewoude KH, Blot SI, Benoit D, Colardyn F, Vogelaers D (2004) Invasive aspergillosis in critically ill patients: attributable mortality and excesses in length of ICU stay and ventilator dependence. J Hosp Infect 56:269–276
Vandewoude KH, Blot SI, Depuydt P, Benoit D, Temmerman W, Colardyn F, Vogelaers D (2006) Clinical relevance of Aspergillus isolation from respiratory tract samples in critically ill patients. Crit Care 10:R31
Perfect JR, Cox GM, Lee JY, Kauffman CA, de Repentigny L, Chapman SW, Morrison VA, Pappas P, Hiemenz JW, Stevens DA (2001). The impact of culture isolation of Aspergillus species: a hospital-based survey of aspergillosis. Clin Infect Dis 33:1824–1833
Sessa A, Meroni M, Battini G, Pitingolo F, Giordano F, Marks M, Casella P (1996) Nosocomial outbreak of Aspergillus fumigatus infection among patients in a renal unit? Nephrol Dial Transplant 11:1322–1324
Anaissie EJ, Costa SF (2001) Nosocomial aspergillosis is waterborne. Clin Infect Dis 33:1546–1548
Anaissie EJ, Stratton SL, Dignani MC, Summerbell RC, Rex JH, Monson TP, Spencer T, Kasai M, Francesconi A, Walsh TJ (2002) Pathogenic Aspergillus species recovered from a hospital water system: a 3-year prospective study. Clin Infect Dis 34:780–789
Reichenberger F, Habicht JM, Gratwohl A, Tamm M (2002) Diagnosis and treatment of invasive pulmonary aspergillosis in neutropenic patients. Eur Respir J 19:743–755
Cenci E, Perito S, Enssle KH, Mosci P, Latge JP, Romani L, Bistoni F (1997) Th1 and Th2 cytokines in mice with invasive aspergillosis. Infect Immun 65:564–570
Cenci E, Mencacci A, Fe DC, Del SG, Mosci P, Montagnoli C, Bacci A, Romani L (1998) Cytokine- and T helper-dependent lung mucosal immunity in mice with invasive pulmonary aspergillosis. J Infect Dis 178:1750–1760
Cenci E, Mencacci A, Del SG, Bacci A, Montagnoli C, d'Ostiani CF, Mosci P, Bachmann M, Bistoni F, Kopf M, Romani L (1999) Interleukin-4 causes susceptibility to invasive pulmonary aspergillosis through suppression of protective type I responses. J Infect Dis 180:1957–1968
Cenci E, Mencacci A, Bacci A, Bistoni F, Kurup VP, Romani L (2000) T cell vaccination in mice with invasive pulmonary aspergillosis. J Immunol 165:381–388
Lederer JA, Rodrick ML, Mannick JA (1999) The effects of injury on the adaptive immune response. Shock 11:153–159
Hartemink KJ, Paul MA, Spijkstra JJ, Girbes AR, Polderman KH (2003) Immunoparalysis as a cause for invasive aspergillosis? Intensive Care Med 29:2068–2071
Maertens J, Vrebos M, Boogaerts M (2001) Assessing risk factors for systemic fungal infections. Eur J Cancer Care 10:56–62
Kwoun MO, Ling PR, Lydon E, Imrich A, Qu Z, Palombo J, Bistrian BR (1997) Immunologic effects of acute hyperglycemia in nondiabetic rats. J Parenter Enteral Nutr 21:91–95
Diamond RD (1983) Inhibition of monocyte-mediated damage to fungal hyphae by steroid hormones. J Infect Dis 147:160
Ng TT, Robson GD, Denning DW (1994) Hydrocortisone-enhanced growth of Aspergillus spp.: implications for pathogenesis. Microbiology 140:2475–2479
Roilides E, Uhlig K, Venzon D, Pizzo PA, Walsh TJ (1993) Prevention of corticosteroid-induced suppression of human polymorphonuclear leukocyte-induced damage of Aspergillus fumigatus hyphae by granulocyte colony-stimulating factor and gamma interferon. Infect Immun 61:4870–4877
Schaffner A (1985) Therapeutic concentrations of glucocorticoids suppress the antimicrobial activity of human macrophages without impairing their responsiveness to gamma interferon. J Clin Invest 76:1755–1764
Crean JM, Niederman MS, Fein AM, Feinsilver SH (1992) Rapidly progressive respiratory failure due to Aspergillus pneumonia: a complication of short-term corticosteroid therapy. Crit Care Med 20:148–150
Pittet D, Huguenin T, Dharan S, Sztajzel-Boissard J, Ducel G, Thorens JB, Auckenthaler R, Chevrolet JC (1996) Unusual cause of lethal pulmonary aspergillosis in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 154:541–544
Rello J, Esandi ME, Mariscal D, Gallego M, Domingo C, Valles J (1998) Invasive pulmonary aspergillosis in patients with chronic obstructive pulmonary disease: report of eight cases and review. Clin Infect Dis 26:1473–1475
Maki DG (1989) Risk factors for nosocomial infection in intensive care. ‘Devices vs nature’ and goals for the next decade. Arch Intern Med 149:30–35
Ader F, Nseir S, Le BR, Leroy S, Tillie-Leblond I, Marquette CH, Durocher A (2005) Invasive pulmonary aspergillosis in chronic obstructive pulmonary disease: an emerging fungal pathogen. Clin Microbiol Infect 11:427–429
Ader F, Nseir S, Guery B, Tillie-Leblond I (2006) Acute invasive pulmonary aspergillosis in chronic lung disease – a review. Rev Mal Respir 23:S11–20
Chen KY, Ko SC, Hsueh PR, Luh KT, Yang PC (2001) Pulmonary fungal infection: emphasis on microbiological spectra, patient outcome, and prognostic factors. Chest 120:177–184
Khasawneh F, Mohamad T, Moughrabieh MK, Lai Z, Ager J, Soubani AO (2006) Isolation of Aspergillus in critically ill patients: a potential marker of poor outcome. J Crit Care 21:322–327
Soubani AO, Khanchandani G, Ahmed HP (2004) Clinical significance of lower respiratory tract Aspergillus culture in elderly hospitalized patients. Eur J Clin Microbiol Infect Dis 23:491–494
Vandewoude KH, Vogelaers D, Blot SI (2006) Aspergillosis in the ICU – the new 21st century problem? Med Mycol 44:S71–76
Prodanovic H, Cracco C, Massard J, Barrault C, Thabut D, Duguet A, Datry A, Derenne JP, Poynard T, Similowski T (2007) Invasive pulmonary aspergillosis in patients with decompensated cirrhosis: case series. BMC Gastroenterol 7:2
Sahlen AO, Suvarna SK, Wilkie ME (2004) A case of invasive pulmonary aspergillosis in renal failure. Nephrol Dial Transplant 19:2687
ter Maaten JC, Golding RP, Strack van Schijndel RJ, Thijs LG (1995) Disseminated aspergillosis after near-drowning. Neth J Med 47:21–24
Vieira DF, Van Saene HK, Miranda DR (1984) Invasive pulmonary aspergillosis after near-drowning. Intensive Care Med 10:203–204
Leroy P, Smismans A, Seute T (2006) Invasive pulmonary and central nervous system aspergillosis after near-drowning of a child: case report and review of the literature. Pediatrics 118:e509–e513
Ascioglu S, Rex JH, de Pauw B, Bennett JE, Bille J, Crokaert F, Denning DW, Donnelly JP, Edwards JE, Erjavec Z, Fiere D, Lortholary O, Maertens J, Meis JF, Patterson TF, Ritter J, Selleslag D, Shah PM, Stevens DA, Walsh TJ (2002) Defining opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplants: an international consensus. Clin Infect Dis 34:7–14
Levy H, Horak DA, Tegtmeier BR, Yokota SB, Forman SJ (1992) The value of bronchoalveolar lavage and bronchial washings in the diagnosis of invasive pulmonary aspergillosis. Respir Med 86:243–248
Cahill BC, Hibbs JR, Savik K, Juni BA, Dosland BM, Edin-Stibbe C, Hertz MI (1997). Aspergillus airway colonization and invasive disease after lung transplantation. Chest 112:1160–1164
Andreas S, Heindl S, Wattky C, Moller K, Ruchel R (2000) Diagnosis of pulmonary aspergillosis using optical brighteners. Eur Respir J 15:407–411
Verweij PE, Mellado E, Melchers WJ (2007) Multiple-triazole-resistant aspergillosis. N Engl J Med 356:1481–1483
Collins J (2001) CT signs and patterns of lung disease. Radiol Clin North Am 39:1115–1135
Greene R (2005) The radiological spectrum of pulmonary aspergillosis. Med Mycol 43:S147–S154
Horger M, Einsele H, Schumacher U, Wehrmann M, Hebart H, Lengerke C, Vonthein R, Claussen CD, Pfannenberg C (2005) Invasive pulmonary aspergillosis: frequency and meaning of the “hypodense sign” on unenhanced CT. Br J Radiol 78:697–703
Kami M, Kishi Y, Hamaki T, Kawabata M, Kashima T, Masumoto T, Oki Y, Tanaka Y, Sawada S, Machida U, Ohtomo K, Kanda Y, Hirai H, Mutou Y (2002) The value of the chest computed tomography halo sign in the diagnosis of invasive pulmonary aspergillosis. An autopsy-based retrospective study of 48 patients. Mycoses 45:287–294
Lee YR, Choi YW, Lee KJ, Jeon SC, Park CK, Heo JN (2005) CT halo sign: the spectrum of pulmonary diseases. Br J Radiol 78:862–865
Pasmans HL, Loosveld OJ, Schouten HC, Thunnissen F, van Engelshoven JM (1992) Invasive aspergillosis in immunocompromised patients: findings on plain film and (HR)CT. Eur J Radiol 14:37–40
Won HJ, Lee KS, Cheon JE, Hwang JH, Kim TS, Lee HG, Han J (1998) Invasive pulmonary aspergillosis: prediction at thin-section CT in patients with neutropenia – a prospective study. Radiology 208:777–782
Pinto PS (2004) The CT halo sign. Radiology 230:37–40
Greene RE, Schlamm HT, Stark P, Oestmann JW, Troke P, Patterson TF, Herbrecht R, Wingard J, Bennett JE, Lortholary J (2003) Radiological findings in acute invasive pulmonary aspergillosis: utility and reliability of halo sign and air crescent sign for diagnosis and treatment of invasive pulmonary aspergillosis in high-risk patients. Abstract European Congress of Microbiology and Infectious Diseases, 13th annual meeting
Maertens J, Verhaegen J, Lagrou K, Van EJ, Boogaerts M (2001) Screening for circulating galactomannan as a noninvasive diagnostic tool for invasive aspergillosis in prolonged neutropenic patients and stem cell transplantation recipients: a prospective validation. Blood 97:1604–1610
Maertens J, Van EJ, Verhaegen J, Verbeken E, Verschakelen J, Boogaerts M (2002) Use of circulating galactomannan screening for early diagnosis of invasive aspergillosis in allogeneic stem cell transplant recipients. J Infect Dis 186:1297–1306
Sulahian A, Boutboul F, Ribaud P, Leblanc T, Lacroix C, Derouin F (2001) Value of antigen detection using an enzyme immunoassay in the diagnosis and prediction of invasive aspergillosis in two adult and pediatric hematology units during a 4-year prospective study. Cancer 91:311–318
Herbrecht R, Letscher-Bru V, Oprea C, Lioure B, Waller J, Campos F, Villard O, Liu KL, Natarajan-Ame S, Lutz P, Dufour P, Bergerat JP, Candolfi E (2002) Aspergillus galactomannan detection in the diagnosis of invasive aspergillosis in cancer patients. J Clin Oncol 20:1898–1906
Pinel C, Fricker-Hidalgo H, Lebeau B, Garban F, Hamidfar R, Ambroise-Thomas P, Grillot R (2003) Detection of circulating Aspergillus fumigatus galactomannan: value and limits of the Platelia test for diagnosing invasive aspergillosis. J Clin Microbiol 41:2184–2186
Pfeiffer CD, Fine JP, Safdar N (2006) Diagnosis of invasive aspergillosis using a galactomannan assay: a meta-analysis. Clin Infect Dis 42:1417–1427
Sanguinetti M, Posteraro B, Pagano L, Pagliari G, Fianchi L, Mele L, La SM, Franco A, Fadda G (2003) Comparison of real-time PCR, conventional PCR, and galactomannan antigen detection by enzyme-linked immunosorbent assay using bronchoalveolar lavage fluid samples from hematology patients for diagnosis of invasive pulmonary aspergillosis. J Clin Microbioll 41:3922–3925
Musher B, Fredricks D, Leisenring W, Balajee SA, Smith C, Marr KA (2004) Aspergillus galactomannan enzyme immunoassay and quantitative PCR for diagnosis of invasive aspergillosis with bronchoalveolar lavage fluid. J Clin Microbiol 42:5517–5522
Seyfarth HJ, Nenoff P, Winkler J, Krahl R, Haustein UF, Schauer J (2001) Aspergillus detection in bronchoscopically acquired material. Significance and interpretation. Mycoses 44:356–360
Clancy CJ, Jaber RA, Leather HL, Wingard JR, Staley B, Wheat LJ, Cline CL, Rand KH, Schain D, Baz M, Nguyen MH (2007) Bronchoalveolar lavage galactomannan in diagnosis of invasive pulmonary aspergillosis among solid-organ transplant recipients. J Clin Microbiol 45:1759–1765
Ansorg R, Van den Boom R, Rath PM (1997) Detection of Aspergillus galactomannan antigen in foods and antibiotics. Mycoses 40:353–357
Viscoli C, Machetti M, Cappellano P, Bucci B, Bruzzi P, Van Lint MT, Bacigalupo A (2004) False-positive galactomannan platelia Aspergillus test results for patients receiving piperacillin–tazobactam. Clin Infect Dis 38:913–916
Adam O, Auperin A, Wilquin F, Bourhis JH, Gachot B, Chachaty E (2004) Treatment with piperacillin–tazobactam and false-positive Aspergillus galactomannan antigen test results for patients with hematological malignancies. Clin Infect Dis 38:917–920
Mattei D, Rapezzi D, Mordini N, Cuda F, Lo NC, Musso M, Arnelli A, Cagnassi S, Gallamini A (2004) False-positive Aspergillus galactomannan enzyme-linked immunosorbent assay results in vivo during amoxicillin–clavulanic acid treatment. J Clin Microbiol 42:5362–5363
Sulahian A, Touratier S, Ribaud P (2003) False-positive test for Aspergillus antigenemia related to concomitant administration of piperacillin and tazobactam. N Engl J Med 349:2366–2367
Becker MJ, De MS, Fens MH, Verbrugh HA, Bakker-Woudenberg IA (2003) Effect of amphotericin B treatment on kinetics of cytokines and parameters of fungal load in neutropenic rats with invasive pulmonary aspergillosis. J Antimicrob Chemother 52:428–434
Marr KA, Laverdiere M, Gugel A, Leisenring W (2005) Antifungal therapy decreases sensitivity of the Aspergillus galactomannan enzyme immunoassay. Clin Infect Dis 40:1762–1769
Verweij PE, Latge JP, Rijs AJ, Melchers WJ, de Pauw BE, Hoogkamp-Korstanje JA, Meis JF (1995) Comparison of antigen detection and PCR assay using bronchoalveolar lavage fluid for diagnosing invasive pulmonary aspergillosis in patients receiving treatment for hematological malignancies. J Clin Microbiol 33:3150–3153
Maertens J, Theunissen K, Verbeken E, Lagrou K, Verhaegen J, Boogaerts M, Eldere JV (2004) Prospective clinical evaluation of lower cut-offs for galactomannan detection in adult neutropenic cancer patients and haematological stem cell transplant recipients. Br J Haematol 126:852–860
Salonen J, Lehtonen OP, Terasjarvi MR, Nikoskelainen J (2000) Aspergillus antigen in serum, urine and bronchoalveolar lavage specimens of neutropenic patients in relation to clinical outcome. Scand J Infect Dis 32:485–490
Ostrosky-Zeichner L, Alexander BD, Kett DH, Vazquez J, Pappas PG, Saeki F, Ketchum PA, Wingard J, Schiff R, Tamura H, Finkelman MA, Rex JH (2005) Multicenter clinical evaluation of the (1–> 3) beta-D-glucan assay as an aid to diagnosis of fungal infections in humans. Clin Infect Dis 41:654–659
Digby J, Kalbfleisch J, Glenn A, Larsen A, Browder W, Williams D (2003) Serum glucan levels are not specific for presence of fungal infections in intensive care unit patients. Clin Diagn Lab Immunol 10:882–885
Skladny H, Buchheidt D, Baust C, Krieg-Schneider F, Seifarth W, Leib-Mosch C, Hehlmann R (1999) Specific detection of Aspergillus species in blood and bronchoalveolar lavage samples of immunocompromised patients by two-step PCR. J Clin Microbiol 37:3865–3871
Bretagne S, Costa JM, Marmorat-Khuong A, Poron F, Cordonnier C, Vidaud M, Fleury-Feith J (1995) Detection of Aspergillus species DNA in bronchoalveolar lavage samples by competitive PCR. J Clin Microbiol 33:1164–1168
Raad I, Hanna H, Sumoza D, Albitar M (2002) Polymerase chain reaction on blood for the diagnosis of invasive pulmonary aspergillosis in cancer patients. Cancer 94:1032–1036
Raad I, Hanna H, Huaringa A, Sumoza D, Hachem R, Albitar M (2002) Diagnosis of invasive pulmonary aspergillosis using polymerase chain reaction-based detection of Aspergillus in BAL. Chest 121:1171–1176
Buchheidt D, Baust C, Skladny H, Baldus M, Brauninger S, Hehlmann R (2002) Clinical evaluation of a polymerase chain reaction assay to detect Aspergillus species in bronchoalveolar lavage samples of neutropenic patients. Br J Haematol 116:803–811
White PL, Linton CJ, Perry MD, Johnson EM, Barnes RA (2006) The evolution and evaluation of a whole blood polymerase chain reaction assay for the detection of invasive aspergillosis in hematology patients in a routine clinical setting. Clin Infect Dis 42:479–486
Hope WW, Walsh TJ, Denning DW (2005) Laboratory diagnosis of invasive aspergillosis. Lancet Infect Dis 5:609–622
Garcia ME, Blanco JL, Caballero J, Gargallo-Viola D (2002) Anticoagulants interfere with PCR used to diagnose invasive aspergillosis. J Clin Microbiol 40:1567–1568
Ostrosky-Zeichner L, Marr KA, Rex JH, Cohen SH (2003) Amphotericin B: time for a new “gold standard”. Clin Infect Dis 37:415–425
Wingard JR, Kubilis P, Lee L, Yee G, White M, Walshe L, Bowden R, Anaissie E, Hiemenz J, Lister J (1999) Clinical significance of nephrotoxicity in patients treated with amphotericin B for suspected or proven aspergillosis. Clin Infect Dis 29:1402–1407
Eriksson U, Seifert B, Schaffner A (2001) Comparison of effects of amphotericin B deoxycholate infused over 4 or 24 hours: randomised controlled trial. BMJ 322:579–582
Imhof A, Walter RB, Schaffner A (2003) Continuous infusion of escalated doses of amphotericin B deoxycholate: an open-label observational study. Clin Infect Dis 36:943–951
Andes D, Stamsted T, Conklin R (2001) Pharmacodynamics of amphotericin B in a neutropenic-mouse disseminated-candidiasis model. Antimicrob Agents Chemother 45:922–926
Walsh TJ, Finberg RW, Arndt C, Hiemenz J, Schwartz C, Bodensteiner D, Pappas P, Seibel N, Greenberg RN, Dummer S, Schuster M, Holcenberg JS (1999) Liposomal amphotericin B for empirical therapy in patients with persistent fever and neutropenia. National Institute of Allergy and Infectious Diseases Mycoses Study Group. N Engl J Med 340:764–771
Marr KA, Crippa F, Leisenring W, Hoyle M, Boeckh M, Balajee SA, Nichols WG, Musher B, Corey L (2004) Itraconazole versus fluconazole for prevention of fungal infections in patients receiving allogeneic stem cell transplants. Blood 103:1527–1533
Denning DW, Venkateswarlu K, Oakley KL, Anderson MJ, Manning NJ, Stevens DA, Warnock DW, Kelly SL (1997) Itraconazole resistance in Aspergillus fumigatus. Antimicrob Agents Chemother 41:1364–1368
Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE, Oestmann JW, Kern WV, Marr KA, Ribaud P, Lortholary O, Sylvester R, Rubin RH, Wingard JR, Stark P, Durand C, Caillot D, Thiel E, Chandrasekar PH, Hodges MR, Schlamm HT, Troke PF (2002) Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med 347:408–415
Bohme A, Ruhnke M, Buchheidt D, Karthaus M, Einsele H, Guth S, Heussel G, Heussel CP, Junghanss C, Kern WK, Kubin T, Maschmeyer G, Sezer O, Silling G, Sudhoff T, Szelenyi DH, Ullmann AJ (2003) Treatment of fungal infections in hematology and oncology – guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol 82:S133–S140
Theuretzbacher U, Ihle F, Derendorf H (2006) Pharmacokinetic/pharmacodynamic profile of voriconazole. Clin Pharmacokinet 45:649–663
Saari TI, Laine K, Leino K, Valtonen M, Neuvonen PJ, Olkkola KT (2006) Effect of voriconazole on the pharmacokinetics and pharmacodynamics of intravenous and oral midazolam. Clin Pharmacol Ther 79:362–370
Scherpbier HJ, Hilhorst MI, Kuijpers TW (2003) Liver failure in a child receiving highly active antiretroviral therapy and voriconazole. Clin Infect Dis 37:828–830
von Mach MA, Burhenne J, Weilemann LS (2006) Accumulation of the solvent vehicle sulphobutylether beta cyclodextrin sodium in critically ill patients treated with intravenous voriconazole under renal replacement therapy. BMC Clin Pharmacol 6:6
Smith J, Safdar N, Knasinski V, Simmons W, Bhavnani SM, Ambrose PG, Andes D (2006) Voriconazole therapeutic drug monitoring. Antimicrob Agents Chemother 50:1570–1572
Robatel C, Rusca M, Padoin C, Marchetti O, Liaudet L, Buclin T (2004) Disposition of voriconazole during continuous veno-venous haemodiafiltration (CVVHDF) in a single patient. J Antimicrob Chemother 54:269–270
Trotman RL, Williamson JC, Shoemaker DM, Salzer WL (2001) Antibiotic dosing in critically ill adult patients receiving continuous renal replacement therapy. Clin Infect Dis 41:1159–1166
Imhof A, Balajee SA, Fredricks DN, Englund JA, Marr KA (2004) Breakthrough fungal infections in stem cell transplant recipients receiving voriconazole. Clin Infect Dis 39:743–746
Marty FM, Cosimi LA, Baden LR (2004) Breakthrough zygomycosis after voriconazole treatment in recipients of hematopoietic stem-cell transplants. N Engl J Med 350:950–952
Walsh TJ, Raad I, Patterson TF, Chandrasekar P, Donowitz GR, Graybill R, Greene RE, Hachem R, Hadley S, Herbrecht R, Langston A, Louie A, Ribaud P, Segal BH, Stevens DA, van Burik JA, White CS, Corcoran G, Gogate J, Krishna G, Pedicone L, Hardalo C, Perfect JR (2007) Treatment of invasive aspergillosis with posaconazole in patients who are refractory to or intolerant of conventional therapy: an externally controlled trial. Clin Infect Dis 44:2–12
Denning DW (2003) Echinocandin antifungal drugs. Lancet 362:1142–1151
Maertens J, Raad I, Petrikkos G, Boogaerts M, Selleslag D, Petersen FB, Sable CA, Kartsonis NA, Ngai A, Taylor A, Patterson TF, Denning DW, Walsh TJ (2004) Efficacy and safety of caspofungin for treatment of invasive aspergillosis in patients refractory to or intolerant of conventional antifungal therapy. Clin Infect Dis 39:1563–1571
Walsh TJ, Teppler H, Donowitz GR, Maertens JA, Baden LR, Dmoszynska A, Cornely OA, Bourque MR, Lupinacci RJ, Sable CA, de Pauw BE (2004) Caspofungin versus liposomal amphotericin B for empirical antifungal therapy in patients with persistent fever and neutropenia. N Engl J Med 351:1391–1402
Lin SJ, Schranz J, Teutsch SM (2001) Aspergillosis case-fatality rate: systematic review of the literature. Clin Infect Dis 32:358–366
Patterson TF, Kirkpatrick WR, White M, Hiemenz JW, Wingard JR, Dupont B, Rinaldi MG, Stevens DA, Graybill JR (2000) Invasive aspergillosis. Disease spectrum, treatment practices, and outcomes. Aspergillus Study Group. Medicine (Baltimore) 79:250–260
Lewis RE, Kontoyiannis DP (2001) Rationale for combination antifungal therapy. Pharmacotherapy 21:149S–164S
Kumar S, Chakrabarti R (2000) Amphotericin B both inhibits and enhances T-cell proliferation: inhibitory effect is mediated through H(2)O(2) production via cyclooxygenase pathway by macrophages. J Cell Biochem 77:361–371
Aliff TB, Maslak PG, Jurcic JG, Heaney ML, Cathcart KN, Sepkowitz KA, Weiss MA (2003) Refractory Aspergillus pneumonia in patients with acute leukemia: successful therapy with combination caspofungin and liposomal amphotericin. Cancer 97:1025–1032
Kontoyiannis DP, Hachem R, Lewis RE, Rivero GA, Torres HA, Thornby J, Champlin R, Kantarjian H, Bodey GP, Raad II (2003) Efficacy and toxicity of caspofungin in combination with liposomal amphotericin B as primary or salvage treatment of invasive aspergillosis in patients with hematologic malignancies. Cancer 98:292–299
Thiebaut A, Antal D, Breysse MC (2002) Refractory invasive fungal infections in patients with hematological malignancies: combination of new antifungal agents (voriconazole or caspofungin) with amphotericin B. In: Program and Abstracts of the 42nd Interscience Conference on Antimicrobial Agents and Chemotherapy, San Diego, California
Singh N, Limaye AP, Forrest G, Safdar N, Munoz P, Pursell K, Houston S, Rosso F, Montoya JG, Patton P, Del BR, Aguado JM, Fisher RA, Klintmalm GB, Miller R, Wagener MM, Lewis RE, Kontoyiannis DP, Husain S (2006) Combination of voriconazole and caspofungin as primary therapy for invasive aspergillosis in solid organ transplant recipients: a prospective, multicenter, observational study. Transplantation 81:320–326
Antoniadou A, Kontoyiannis DP (2003) Status of combination therapy for refractory mycoses. Curr Opin Infect Dis 16:539–545
Fluckiger U, Marchetti O, Bille J, Eggimann P, Zimmerli S, Imhof A, Garbino J, Ruef C, Pittet D, Tauber M, Glauser M, Calandra T (2006) Treatment options of invasive fungal infections in adults – review. Swiss Med Wkly 136:447–463
Kontoyiannis DP, Lewis RE (2003) Combination chemotherapy for invasive fungal infections: what laboratory and clinical studies tell us so far. Drug Resist Updat 6:257–269
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: http://dx.doi.org/10.1007/s00134-007-0792-y.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 2.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by-nc/2.0/.
About this article
Cite this article
Trof, R.J., Beishuizen, A., Debets-Ossenkopp, Y.J. et al. Management of invasive pulmonary aspergillosis in non-neutropenic critically ill patients. Intensive Care Med 33, 1694–1703 (2007). https://doi.org/10.1007/s00134-007-0791-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0791-z