Abstract
Objective
To compare the triggering performance of mid-level ICU mechanical ventilators with a standard ICU mechanical ventilator.
Design
Experimental bench study.
Setting
The respiratory care laboratory of a university-affiliated teaching hospital.
Subject
A computerized mechanical lung model, the IngMar ASL5000.
Interventions
Ten mid-level ICU ventilators were compared to an ICU ventilator at two levels of lung model effort, three combinations of respiratory mechanics (normal, COPD and ARDS) and two modes of ventilation, volume and pressure assist/control. A total of 12 conditions were compared.
Measurements and main results
Performance varied widely among ventilators. Mean inspiratory trigger time was <100 ms for only half of the tested ventilators. The mean inspiratory delay time (time from initiation of the breath to return of airway pressure to baseline) was longer than that for the ICU ventilator for all tested ventilators except one. The pressure drop during triggering (Ptrig) was comparable with that of the ICU ventilator for only two ventilators. Expiratory Settling Time (time for pressure to return to baseline) had the greatest variability among ventilators.
Conclusions
Triggering differences among these mid-level ICU ventilators and with the ICU ventilator were identified. Some of these ventilators had a much poorer triggering response with high inspiratory effort than the ICU ventilator. These ventilators do not perform as well as ICU ventilators in patients with high ventilatory demand.
Similar content being viewed by others
Introduction
As a group, mechanical ventilators can be categorized into four sub-groups: (1) non-invasive positive pressure ventilators; (2) transport/home care ventilators; (3) mid-level ICU or subacute care ventilators, ventilators with limited capability when compared to standard ICU ventilators but designed for use in the acute care setting; and (4) ICU ventilators. A precise definition of a mid-level ventilator does not exist. We included ventilators for this study considered by their manufacturer as midlevel ventilators. In general, the gas delivery, mode and monitoring capabilities as well as price of these ventilators are between those of home care and ICU ventilators. Of these four groups, the ICU ventilators are the most sophisticated and used more commonly. As a result, they are the group that has been most frequently studied in the laboratory [1–3]. However, the mid-level ICU ventilators are becoming increasingly available in many hospitals and being used in many settings where ICU ventilators were traditionally used. Previous studies have also evaluated the performance of NPPV ventilators [4–6] and home/transport ventilators [7–9], but, to our knowledge, such evaluations have never been done for mid-level ICU ventilators.
One of the primary goals of mechanical ventilation is to reduce the patient’s work of breathing [10–12]. During patient-triggered assisted ventilation, unloading of patient effort is highly dependent on patient–ventilator interaction [13–15], which is affected by triggering and the gas delivery characteristics of the ventilator. Previous studies of ICU ventilators [1, 2, 16], as well as home care transport ventilators [7–9] and NPPV ventilators [4–6] indicate that triggering and gas delivery capabilities of these ventilators can vary greatly.
In this study we compare the performance of ten mid-level ICU mechanical ventilators to each other and to one ICU ventilator using a computerized mechanical lung model to simulate patient’s inspiratory efforts and respiratory system mechanical characteristics. We hypothesized that the performance of these mid-level ICU mechanical ventilators would vary widely and would not be equivalent to the performance of the ICU ventilator. Our results have been previously published as an abstract [17].
Methods
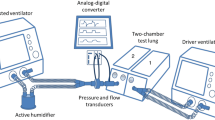
Ten mid-level mechanical ventilators (Table 1) were compared to each other and to a standard ICU ventilator, the PB840 (Puritan Bennett, Pleasanton, CA, USA) using the ASL5000 lung simulator (IngMar Medical, Pittsburg, PA, USA). The 840 was chosen because of its excellent triggering and gas delivery performance in previous studies of ICU ventilators [1, 3, 16]. The ASL5000 simulator is a computerized mechanical lung simulator consisting of a piston moving inside a cylinder. The lung model uses the equation of motion to control the movement of the piston:
where: E = elastance, or 1/compliance; V = volume; R = resistance; V′ = flow; PEEP = positive end expiratory effort; Pmus = muscle pressure (inspiratory effort); Paw = airway pressure.
Flow and airway pressure are measured by flow and pressure sensors at the entrance of the piston, and volume is obtained by integration of flow over time. The user sets compliance, resistance, and the Pmus profile/waveform. The ASL5000 executes the necessary calculations at 2,000 Hz to control the piston movement.
Each ventilator evaluated was connected to the ASL5000 by the manufacturer’s standard circuit, if provided, or a standard disposable corrugated circuit (Hudson, Temecula, CA, USA) when no circuit was provided.
Study setup
Three combinations of resistance (Rrs) and compliance (Crs) to simulate normal (Rrs = 3 cm H2O/L s−1, Crs = 60 mL/cm H2O), COPD (Rrs = 10 cm H2O/L s−1, Crs = 80 mL/cm H2O), and ARDS patients (Rrs = 7.5 cm H2O/L s−1, Crs = 30 mL/cm H2O) were set on the ASL5000. Two levels of effort were set, 30 and 60 L/min peak flow demand, to simulate low and high patient effort, respectively. In addition, two modes of ventilation, pressure assist/control (PCV) and volume assist/control (VCV) were applied at each of the settings, resulting in 12 test conditions. Prior to the beginning of data collection, we used the duration of inspiratory effort and flow demand of the lung model to set each ventilator. For VCV, target tidal volume was calculated using the lung model’s inspiratory time and flow demand. Inspiratory flow was titrated to equal the lung model’s flow and inspiratory time demand using a decelerating flow pattern when available. For PCV, we chose an inspiratory pressure of 10 cm H2O and inspiratory time was the same as used in VCV. The values set are shown in Table 2; the same settings were used for all ventilators. Inspiratory rise time, when adjustable, was set to the fastest value that did not cause an initial pressure overshoot that would shutdown the lung model, and triggering was set at the most sensitive value that did not cause auto-triggering. PEEP was set at 5 cm H2O. In addition, the respiratory rate was maintained at 15/min to avoid the development of intrinsic PEEP. No intrinsic PEEP was identified with any ventilator regardless of lung model or ventilator settings. When available, flow triggering was preferred over pressure triggering. Some ventilators used a standard, disposable, double-limbed breathing circuit with a compressible volume of 1.7 mL/cm H2O. Other ventilators required a proprietary circuit. Compressible volume ranged from 0.6 to 1.7 mL/cm H2O with a mean of 1.4 mL/cm H2O. Table 1 shows rise time and sensitivity settings for all the tested ventilators.
Variables evaluated
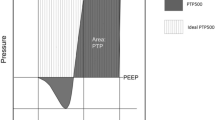
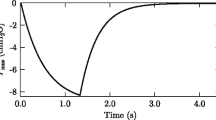
Figure 1 illustrates the variables that we measured on each ventilator during all comparisons. Three of these four variables addressed the trigger function of the ventilator and the fourth is the function of the exhalation valve. Inspiratory Trigger Time (Ttrig): Defined as time in seconds from beginning of the lung model’s inspiratory effort to the lowest value of airway pressure (Paw) needed to trigger the ventilator. Inspiratory Time Delay (TI delay): Defined as time in seconds from the beginning of the lung model’s inspiratory effort, causing Paw to fall below baseline, to the return of Paw to baseline. Ttrig reflects how fast the ventilator identifies patient effort and initiates inspiratory flow, evaluating the “pre-triggering phase”. TI delay evaluates the whole triggering process, not only patient effort recognition but also ability of the ventilator to deliver adequate initial flow to counteract patient effort and pressurize the system.
Airway pressure versus time tracing illustrating the variables evaluated. Inspiratory Trigger Time (Ttrig) is time (s) from the beginning of the lung model’s inspiratory effort to the lowest value of airway pressure (Paw) during triggering; Inspiratory Delay Time (TI delay) is the time (s) from the beginning of the lung model’s inspiratory effort, causing Paw to fall below baseline, to the return of Paw to baseline; Inspiratory Trigger Pressure (Ptrig) is the magnitude of airway pressure drop (cm H2O) during triggering; Expiratory Settling Time (TE sett) is time (s) from the beginning of expiration to return and stabilization of Paw to baseline (PEEP level)
Inspiratory Trigger Pressure (Ptrig): defined as the magnitude of airway pressure drop during triggering, in cm H2O. Expiratory Settling Time (TE sett): defined as time in seconds from the beginning of expiration to the return and stabilization of Paw at baseline (PEEP level).
Data collection and analysis
Ventilators were allowed to stabilize in each test condition for 3 to 5 min, after which one minute of ventilation was recorded. Data acquisition was done at 512 Hz and stored in a desktop computer. Offline analysis on a breath-by-breath basis was done by the ASL5000 Labview software (National Instruments, Austin, TX, USA). All breaths were visually inspected and five representative breaths were selected for analysis. Results are presented as means ± standard deviation. Statistical analysis was done with SPSS (Chicago, IL, USA). ANOVA and Dunnett T3 test for multiple comparisons was used for overall comparisons between ventilators and for the comparisons of lung mechanics within each ventilator, and paired t-tests were used for comparisons between level of effort and mode of ventilation within each of the ventilators. A P-value <0.05 was considered significant. Differences greater than 10% were considered important. We chose to report only differences that were both statistically significant and important because of the small standard deviations observed with lung model studies, which resulted in differences being statistically significant even when within measurement error.
Results
Overall performance
Table 3 lists the combined results for each ventilator across the 12 test conditions by Ttrig. This same listing is also used in all figures. Ttrig was <100 ms for most ventilators. The PB840 and Vela had the shortest Ttrig. TI delay had a very similar pattern, and the only ventilator to have a mean TI delay shorter than 100 ms was the 840.
Ptrig was greater than 2 cm H20 for all ventilators except the Vela and the PB840. TE sett was shortest for the Savina and longest for the Esprit.
Effect of lung mechanics
Comparisons between simulated normal, ARDS and COPD lung mechanics were determined by combining the results from the two modes of ventilation and two levels of effort for each ventilator (Fig. 2). The impact of ARDS on the target variables was consistent, whereas for COPD, the impact was much more variable among ventilators
Comparison of the evaluated variables among normal, COPD and ARDS lung mechanics for each of the ventilators. Gray bars represent normal, dashed bars represent COPD and black bars represent ARDS mechanics. * Indicates that the difference, in relation to normal, was statistically and clinically (>10%) significant
.
Compared to normal mechanics, simulated ARDS mechanics resulted in shorter Ttrig for most ventilators. ARDS mechanics had little impact on TI delay. However, ARDS resulted in a greater Ptrig for most ventilators and shorter TE sett for all ventilators.
Compared to normal, COPD resulted in shorter Ttrig, but the effect was less pronounced than that of ARDS and not seen for all ventilators. COPD mechanics had a variable effect on TI delay. Also, COPD mechanics resulted in greater Ptrig for most ventilators.
Effect of inspiratory effort
Comparisons between high and low effort were determined by combining the results from the two modes of ventilation and three levels of lung mechanics for each ventilator (Fig. 3). High effort resulted in shorter Ttrig for most ventilators. High effort had little impact on TI delay. Ptrig for all ventilators was increased by higher effort, but high effort had almost no impact on TE sett.
Effect of mode of ventilation
Comparisons between PCV and VCV were determined by combining the results from the two levels of effort and three levels of lung mechanics for each ventilator (Fig. 4). Compared to VCV, PCV had little impact on Ttrig. TI delay with PCV was longer for some ventilators than with VCV. Ptrig and TE sett with PCV had varying effects compared with VCV.
Discussion
The findings of this study can be summarized as follows: (1) the triggering capabilities of the mid-level ICU ventilators did not equal that of the PB840 ICU ventilator (Table 3); (2) Ttrig and TI delay tended to be longer, whereas Ptrig and TE sett tended to be greater in the mid-level ICU ventilators than that in the PB840; (3) triggering performance of the mid-level ICU ventilators decreased as flow demand increased; (4) Overall these ventilators performed better during simulated ARDS than COPD or normal lung mechanics; and (5) large trigger performance variability was found across mid-level ICU ventilators.
Overall triggering performance
For all variables evaluated, most mid-level ICU ventilators had greater breath-by-breath variability and greater variability across test conditions than the PB840 (Table 3). There were also important differences in overall performance among the mid-level ICU ventilators, consistent with comparisons among other non-ICU ventilators (transport, home and NPPV ventilators) [7, 9, 18].
Inspiratory trigger time evaluates the ability of the ventilator to sense inspiratory effort and open the inspiratory flow valve. Ttrig was less than 100 ms, which is considered a reasonable cutoff, for only half of the mid-level ICU ventilators tested. Previous studies evaluating bilevel ventilators [6] and ICU ventilators [16] also found that most ventilators took longer than 100 ms to trigger, but studies with home ventilators [4], and transport ventilators [8, 9] have reported that many of these ventilators could be triggered in less than 100 ms. These contrasting results are likely related to differences in the level of effort and model mechanics among studies.
Inspiratory Delay Time reflects the ventilator’s ability to pressurize the system above baseline and reflects both triggering capabilities and the ventilator’s performance in the initial phase of inspiration [11, 12]. In general, the more compliant the lung and the lower the resistance, the longer the TI delay. Our results are similar to those of previous studies of other categories of ventilators [5, 7, 16].
Inspiratory Trigger pressure determines the pressure change required to activate gas delivery, and it is related to the lung model used, lung model settings, especially the level of effort, and the individual ventilator algorithms used for triggering and pressurization. As a result, absolute values vary across different studies. Our results contrast with those by Miyoshi et al. [8] who found greater Ptrig for one ICU ventilator when compared to four transport ventilators. During CPAP, Takeuchi et al. [1] found that Ptrig was less than 4 cm H2O for five ICU ventilators.
Expiratory Settling Time reflects the ventilator’s ability to decompress the circuit during exhalation while maintaining PEEP and essentially evaluates the function of the expiratory valve. However, it is also influenced by lung mechanics and tidal volume. As a result, it had the highest variability among the measured variables. It was the only variable for which some of the mid-level ICU ventilators outperformed the PB840. Previous studies have reported similar results with transport and bilevel ventilators [6, 8].
Mode, effort and lung mechanics
The impact of mode of ventilation was small (Fig. 4). This was expected due to study design, because the ventilator settings in each mode were calculated to meet the lung model’s demand, and as a result, tidal volume and flow pattern were very similar for PCV and VCV, and inspiratory times were identical.
Higher effort was associated with a greater airway pressure drop during triggering (Ptrig), and shorter triggering time (Ttrig), but had little or no effect on TI delay. These results are consistent with those previously published [2, 4, 7–9, 16]. The explanation for this is that higher effort results in a faster decrease in airway pressure, shortening the time to reach triggering, but also results in greater airway pressure decrease, counterbalancing the ventilator’s pressurization capabilities and increasing the time to return airway pressure to baseline.
Lung mechanics had a large impact on both inspiratory and expiratory variables. ARDS mechanics reduced Ttrig for all ventilators and tended to decrease TI delay while COPD mechanics tended to increase it. This is a result of the impact of lung mechanics on the post-triggering phase (after triggering while the ventilator pressurizes the system) but is also related to differences in the Ttrig between ARDS and COPD, as TI delay includes Ttrig.
Limitations of the study
The primary limitation of this study is that it was performed on a mechanical model, which can never mimic all of the complexities of the interaction of a mechanical ventilator with a patient. The ASL5000 has two characteristics that make it very different from patients and from the typical dual chamber mechanical models (TTL, Michigan Instruments, Grand Rapids, MI, USA): first, it does not simulate expiratory efforts, normally present in patients with high effort and in dual chamber mechanical models; second, the Pmus profile in the ASL5000 was not modified by pressurization during the inspiratory phase. Therefore, comparisons of our results to previous studies using dual chamber lung models should take this into account.
Conclusions
Most mid-level ICU ventilators do not perform as well as the PB840, exhibit a much greater variability for inspiratory phase variables, and are more susceptible to the influences of level of effort and lung mechanics than that of the PB840. These results indicate that for patients with high inspiratory efforts and altered lung mechanics, ICU ventilators may be superior to mid-level ICU ventilators.
References
Takeuchi M, Williams P, Hess D, Kacmarek RM (2002) Continuous positive airway pressure in new-generation mechanical ventilators: a lung model study. Anesthesiology 96:162–172
Richard JC, Carlucci A, Breton L, Langlais N, Jaber S, Maggiore S, Fougere S, Harf A, Brochard L (2002) Bench testing of pressure support ventilation with three different generations of ventilators. Intensive Care Med 28:1049–1057
Chatmongkolchart S, Williams P, Hess DR, Kacmarek RM (2001) Evaluation of inspiratory rise time and inspiration termination criteria in new-generation mechanical ventilators: a lung model study. Respir Care 46:666–677
Tassaux D, Strasser S, Fonseca S, Dalmas E, Jolliet P (2002) Comparative bench study of triggering, pressurization, and cycling between the home ventilator VPAP II and three ICU ventilators. Intensive Care Med 28:1254–1261
Stell IM, Paul G, Lee KC, Ponte J, Moxham J (2001) Noninvasive ventilator triggering in chronic obstructive pulmonary disease. A test lung comparison. Am J Respir Crit Care Med 164:2092–2097
Bunburaphong T, Imanaka H, Nishimura M, Hess D, Kacmarek RM (1997) Performance characteristics of bilevel pressure ventilators: a lung model study. Chest 111:1050–1060
Battisti A, Tassaux D, Janssens JP, Michotte JB, Jaber S, Jolliet P (2005) Performance characteristics of 10 home mechanical ventilators in pressure-support mode: a comparative bench study. Chest 127:1784–1792
Miyoshi E, Fujino Y, Mashimo T, Nishimura M (2000) Performance of transport ventilator with patient-triggered ventilation. Chest 118:1109–1115
Zanetta G, Robert D, Guerin C (2002) Evaluation of ventilators used during transport of ICU patients—a bench study. Intensive Care Med 28:443–451
Ramar K, Sassoon CS (2005) Potential advantages of patient–ventilator synchrony. [review] [50 refs]. Respir Care Clin N Am 11:307–317
Tobin MJ, Jubran A, Laghi F (2001) Patient–ventilator interaction. Am J Respir Crit Care Med 163:1059–1063
Kondili E, Xirouchaki N, Georgopoulos D (2007) Modulation and treatment of patient–ventilator dyssynchrony. Curr Opin Crit Care 13:84–89
Bigatello LM, Nishimura M, Imanaka H, Hess D, Kimball WR, Kacmarek RM (1997) Unloadiing of the work of breathing by proportional assist ventilation in a lung model. Crit Care Med 25:267–272
Sassoon CS, Foster GT (2001) Patient–ventilator asynchrony. Curr Opin Crit Care 7:28–33
Prinianakis G, Kondili E, Georgopoulos D (2005) Patient–ventilator interaction: an overview. Respir Care Clin N Am 11:201–224
Williams P, Kratohvil J, Ritz R, Hess DR, Kacmarek RM (2000) Pressure support and pressure assist/control: are there differences? an evaluation of the newest intensive care unit ventilators. Respir Care 45:1169–1181
Ferreira CJ, Chipman DW, Kacmarek RM (2006) (Abstract) Performance of mechanical ventilators in the setting of patient effort: a bench study. Respir Care 51:1284
Lofaso F, Brochard L, Hang T, Lorino H, Harf A, Isabey D (1996) Home versus intensive care pressure support devices. experimental and clinical comparison. Am J Respir Crit Care Med 153:1591–1599
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was partially funded by an unrestricted grant from Hamilton Medical; Dr. Ferreira was partially funded by CAPES, Brazil.
Robert Kacmarek has received research grants and honorariums for lecturing from Hamilton Medical, Puritan-Bennett Corp, Respironics Inc. Viasys Inc and Maquet Medical and is a consultant for Space Labs. Daniel Chipman has received honorarium from Maquet Medical for lecturing.
Rights and permissions
About this article
Cite this article
Ferreira, J.C., Chipman, D.W. & Kacmarek, R.M. Trigger performance of mid-level ICU mechanical ventilators during assisted ventilation: a bench study. Intensive Care Med 34, 1669–1675 (2008). https://doi.org/10.1007/s00134-008-1125-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1125-5