Abstract
Purpose
Preclinical studies suggest that HMG-CoA reductase inhibitors (statins) may attenuate organ dysfunction. We evaluated whether statins are associated with attenuation of lung injury and prevention of associated organ failure in patients with ALI/ARDS.
Methods
From a database of patients with ALI/ARDS, we determined the presence and timing of statin administration. Main outcome measures were the development and progression of pulmonary and nonpulmonary organ failures as assessed by changes in PaO2/FiO2 ratio and Sequential Organ Failure Assessment score (SOFA) between days 1 and 7 after the onset of ALI/ARDS. Secondary outcomes included ventilator free days, ICU and hospital mortality, and lengths of ICU and hospital stay.
Results
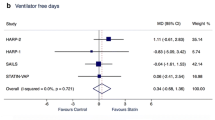
From 178 patients with ALI/ARDS, 45 (25%) received statin therapy. From day 1 to day 7, the statin group showed less improvement in their PaO2/FiO2 ratio (27 vs. 55, P = 0.042). Ventilator free days (median 21 vs. 16 days, P = 0.158), development or progression of organ failures (median ΔSOFA 1 vs. 2, P = 0.275), ICU mortality (20% vs. 23%, P = 0.643), and hospital mortality (27 vs. 37%, P = 0.207) were not significantly different in the statin and non-statin groups. After adjustment for baseline characteristics and propensity for statin administration, there were no differences in ICU or hospital lengths of stay.
Conclusion
In this retrospective cohort study, statin use was not associated with improved outcome in patients with ALI/ARDS. We were unable to find evidence for protection against pulmonary or nonpulmonary organ dysfunction.
Similar content being viewed by others
Introduction
Acute lung injury (ALI) and the acute respiratory distress syndrome (ARDS) are critical illnesses with significant associated morbidity and mortality. The hallmark of ALI/ARDS is the acute onset of hypoxemia in the setting of diffuse bilateral infiltrates on chest radiography with an absence of left atrial hypertension [1]. Though strategies such as low tidal volume ventilation [2] and restrictive fluid management [3] may lead to improved outcomes, morbidity and mortality remain high. Unfortunately, pharmacologic therapies (inhaled nitric oxide, prostaglandin E1, surfactant, lisofylline, ketoconazole, and N-acetylcysteine) have been disappointing.
HMG-CoA reductase inhibitors (statins) are effective lipid lowering drugs often used for primary and secondary prevention of cardiovascular disease. Recently, statins have been shown to possess important anti-inflammatory, immunomodulatory and antioxidant effects, independent of their lipid lowering properties [4–6]. As ALI/ARDS is believed to be mediated by an intense inflammatory response within the lungs with associated oxidant injury [7], it is plausible that statin therapy may ameliorate this syndrome. Indeed, statins have been noted to attenuate lung injury in a variety of animal models [5, 6, 8, 9]. Jacobson et al. [8] noted a reduction in inflammatory indices and attenuation of vascular leak with statin administration in a murine model of acute lung injury. Pirat et al. [6] noted a reduction in the severity of acute lung injury in rats receiving statin therapy prior to clamping the superior mesenteric artery (intestinal ischemia/reperfusion induced acute lung injury). To date, this protective effect has not been observed in clinical investigations.
Importantly, statins are believed protective in a variety of other disease states as well. Though their impact on perioperative cardiovascular morbidity and mortality have perhaps received the greatest interest [10–15], evidence exists for a role in acute kidney injury [15, 16], bacteremia/sepsis [17–24], and cerebrovascular disease [25, 26] as well. As the majority of patients with ALI/ARDS do not die from respiratory failure but rather from sepsis syndrome with multi-organ failure [27, 28], we speculated that statins may improve outcome in this regard as well. We undertook this retrospective review to evaluate the potential role of HMG-CoA reductase inhibitors in the attenuation of lung injury in ALI/ARDS and the prevention of associated distal organ dysfunction.
Materials and methods
Study population
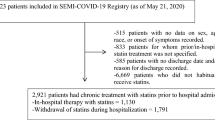
After institutional review board approval, we reviewed a pre-existing database [29] that included consecutive prospectively collected adult (>18 years) cases of ALI and ARDS occurring in three different intensive care units (ICU) at a single academic institution over a 7-month period (October 2005–May 2006). The availability of an “in-house” night time critical care consultant in one of the three ICU’s involved in the study was the only significant systematic change in critical care practice over the data collection period. All patients who met criteria for ALI or ARDS over this time interval were included in the database. Patients who denied the use of their medical records for research were excluded (n = 4). The three ICUs studied include a primary medical ICU, surgical (non-cardiac, non-neurologic) ICU, and a mixed medical/surgical (non-cardiac, non-neurologic) ICU. ALI and ARDS were defined according to the criteria established by the American-European Consensus Conference (AECC) [1].
Data abstraction
Electronic medical records were reviewed and data abstracted by the study investigators. Data on baseline demographics (age, gender, admission location, postoperative state), patient comorbidities, baseline Sequential Organ Failure Assessment (SOFA) scores [30], and severity of illness and predicted hospital death as determined by the Acute Physiology and Chronic Health Evaluation Survey (APACHE) III [31] were recorded. The etiology of ALI/ARDS (pulmonary vs. extrapulmonary), presence of relevant coexisting conditions, initial PaO2/FiO2 ratios and ventilatory parameters at the time of meeting AECC criteria were noted, as were the patients’ Do Not Resuscitate (DNR) status on admission to the ICU.
We then determined whether each patient was being treated with an HMG-CoA reductase inhibitor at the time of hospital admission, received this therapy during their hospitalization, received therapy during both time periods, or did not receive a statin at any time. Initial comparisons were made separately for those who received a statin at any point (pre-hospitalization only or continued during the hospitalization) and the subgroup of statin users whose therapy was continued after admission to the hospital. As outcomes were not significantly different with these separate comparisons, our final analyses compared patients who received a statin at any time to those who did not receive such therapy.
Measurements and outcome
Outcomes measures were defined a priori. The primary outcome measures were the change in PaO2/FiO2 ratio (∆PaO2/FiO2 = PaO2/FiO2 on day 7 to PaO2/FiO2 on day 1) and the change in SOFA score (∆SOFA = SOFA score on day 1 to SOFA score on day 7). Day 1 was defined as the time the patient first met AECC criteria for ALI/ARDS. For those who were discharged from the ICU prior to day 7, the last ICU day was utilized for determining day 7 values. Missing SOFA score data points were assumed to be normal. Secondary outcome measures included ventilator free days (VFD) at day 28, ICU and hospital (HOS) mortality, and ICU and HOS lengths of stay (LOS). Patients who died prior to day 28 were considered to have had 0 VFD.
Statistical analysis
The sample size needed to detect a difference of 50 mmHg in ΔPaO2/FiO2 ratio between the two groups (statin vs. no statin) was estimated at a total of 106 patients with an alpha of 0.05, beta of 0.8, and SD of 91 (as calculated from the ΔPaO2/FiO2 ratio for the control group–non-statin). The sample size needed to detect a difference of two points in ΔSOFA score between the two groups was estimated at a total of 116 patients with an alpha of 0.05, beta of 0.8, and SD of 3.82 (as calculated from the ΔSOFA score for the control group–non-statin). Both sample size calculations assumed an equal distribution of patients in each subgroup. Dichotomous variables are presented as counts with percentages. Continuous data are presented as median with 25–75% interquartile ranges (IQ range). For univariate analysis, comparisons between the two groups were performed with a Pearson’s χ2 test or Fisher’s exact test as appropriate for categorical variables. Continuous variables were tested using a nonparametric Mann–Whitney rank-sum test. Because observational studies risk unequal distributions of important covariates between treatment groups, the probability of receiving statin therapy was calculated with propensity scores. Propensity scores, defined as the conditional probability of being treated given an individual’s profile of covariates, attempt to minimize bias by accounting for variables that alter the probability of being treated. Once determined, the propensity score can then be used to minimize bias through matching, stratification, or regression adjustment. This is, in effect, an attempt to ‘quasi-randomize’ an observational trial. In the present study, propensity scores for statin administration were determined with multivariate analysis taking statin administration as a primary outcome variable. Covariates were entered in the model when significant differences (P < 0.05) were noted between statin and non-statin user’s baseline characteristics or when strong biologic associations were thought possible. Variables entered into the initial model included age, gender, admission to the mixed medical/surgical intensive care unit, admission to the surgical intensive care unit, SOFA-1 score, pulmonary ARDS, sepsis, postoperative state (yes/no), hyperlipidemia, coronary artery disease (CAD), congestive heart failure (CHF), peripheral vascular disease (PVD), and diabetes mellitus. The model was refined with forward, then backwards, stepwise regression, taking into account colinearity and interaction. The model was completed with nominal logistic regression. Multivariate analysis was also performed for ICU LOS. Covariates entered in the final model included statin administration, propensity score for statin administration, APACHE III predicted ICU LOS, DNR code status on admission to the ICU, and postoperative state (yes/no).
Results
From 178 patients with ALI/ARDS, 45 (25%) were receiving statin therapy at the time of hospitalization. Thirty-five of these patients had their statin therapy continued during the hospitalization. In ten patients, the statin was discontinued on admission to the hospital. The patients’ baseline characteristics are presented in Table 1. The statin group was slightly older, less likely to be admitted to the “mixed” ICU, had a higher prevalence of diabetes mellitus, and had lower baseline SOFA scores (Table 1). A higher percentage of the non-statin patients had associated sepsis (62 vs. 36%; P = 0.002). As expected, the statin group had a higher incidence of hyperlipidemia, CAD, CHF, and PVD. The groups were not significantly different in regards to gender, initial PaO2/FiO2 ratios, postoperative state, DNR status on admission to the ICU, or ventilator parameters at the time of meeting diagnostic criteria for ALI/ARDS.
Univariate analyses of patient outcomes are shown in Table 2. When evaluating ∆PaO2/FiO2, less improvement was noted in the statin group. No differences between groups were noted in ∆SOFA score, VFD, ICU mortality (20 vs. 23%, statin vs. no statin; odds ratio, 0.82; 95% confidence interval, 0.36 to 1.89; p = 0.643), or hospital mortality (27 vs. 37%, statin vs. no statin; odds ratio, 0.62; 95% confidence interval, 0.29–1.32; P = 0.207). Whereas no difference was noted in hospital LOS, a shorter ICU LOS was observed in the statin cohort.
As the statin group’s ICU LOS was significantly shorter in univariate analysis, multivariable evaluation incorporating the propensity score for statin administration was performed. The probability of receiving statin therapy was evaluated as described above. CAD, hyperlipidemia and PVD were strong predictors of statin administration (Table 3). Sepsis and admission to the mixed medical/surgical ICU were associated with a reduced likelihood of receiving statin therapy. The model proved reliable with an area under the curve (AUC) of 0.88. Additional covariates entered in the multivariable ICU LOS evaluation included statin administration, APACHE III predicted ICU LOS, postoperative state, and DNR status on admission to the ICU. APACHE III predicted ICU LOS and DNR status on ICU admission were statistically significant predictors of actual ICU LOS. The association between statin administration and ICU LOS found in univariate analysis was lost in this multivariate evaluation (Table 4).
An additional evaluation was performed after stratification according to the propensity for receiving statin therapy. The group was dichotomized into those with low probability for statin administration (propensity score <0.50) and those with high probability for statin administration (propensity score >0.50). We noted an inconsistent effect with statin therapy when comparing the low probability to high probability subgroups (Table 5). Specifically, though statins were associated with more VFD and lower ICU and hospital mortality in the high probability cohort, this apparent effect was absent in the low probability subgroup.
Subgroup evaluation of the statin cohort noted a higher baseline severity of illness in statin users whose therapy was stopped after hospital admission (n = 10) when compared to patients who continued to receive statin therapy after hospital admission (electronic supplementary material Table E1). When these ten patients were excluded in a sensitivity analysis, the results were not significantly different (electronic supplementary material Tables E2, E3).
Discussion
In light of the apparent beneficial effects of statin therapy in animal models with or at risk for ALI/ARDS, we hypothesized that statins may prevent the progression of pulmonary and nonpulmonary organ dysfunction in patients with ALI/ARDS. Despite lower baseline SOFA scores and a lower prevalence of sepsis in the statin cohort, the present study did not find evidence for a beneficial treatment effect. Specifically, we were unable to find evidence for either lung protection or protection against associated organ system dysfunction, our primary outcomes of interest. Though univariate analysis noted a shorter ICU LOS in the statin group, this association was lost in multivariate evaluation.
Further evaluation noted differential effects of statin therapy when comparing the subgroup of patients with low probability for statin administration to those with high probability (Table 5). We specifically noted a lack of effect with statin therapy in the cohort of patients with a low propensity for statin administration (propensity score < 0.50). Should a true beneficial effect of statin therapy exist, it would be expected to persist independent of the propensity score. These results further temper our enthusiasm for the potential role of statin therapy in the management of ALI/ARDS.
We acknowledge the retrospective observational design of the present study with the associated potential for multiple confounding variables. Importantly, statin administration was prescribed at the discretion of treating physicians and could have been influenced by factors that were not measured in this study (e.g., tolerance to the enteral route of administration). We also noted variable consistency in the administration of statin therapy. Some patients (n = 10) who were receiving statins in the pre-hospital setting did not continue to receive this therapy after admission to the hospital. One could postulate that outcomes might have been different had their therapy been continued. Although we observed similar results when these ten patients were excluded in a sensitivity analysis, the small sample size limits meaningful conclusions. In addition, our sample size calculations assumed equal distributions of statin exposure which was not the case. The substantially larger number of patients enrolled (n = 178) should mitigate this limitation. Nevertheless, it is clearly possible that significant associations were missed due to a lack of power. Due to the limited sample size we were also unable to perform subgroup analysis between the different HMG-CoA reductase inhibitor medications or dosing regimens. These would be important considerations in future efforts evaluating the potential benefit of statin therapy.
HMG-CoA reductase inhibitors are believed to improve outcome after major non-cardiac surgery [10–14]. These beneficial effects have primarily been attributed to a reduction in cardiac morbidity. Though the mechanism by which this protection occurs is unclear, it is not believed to be a result of lipid lowering. Rather, these more immediate protective effects have been attributed to anti-inflammatory activity [17, 18, 32, 33], antioxidant activity [4–7], and optimization of endothelial function with increased nitric oxide and reduced endothelin-1 production [4, 18, 32, 34].
More recently, statins have been shown to attenuate lung injury in a variety of animal models [5, 6, 8, 9, 35]. To our knowledge, this association has not been well studied in human trials. In the present study, statin users were noted to have less improvement in their P/F ratios and similar VFD when compared to non-users. Though our results differ from much of the pre-clinical data, several important points deserve mention. First, previous evaluations have focused primarily on ALI prevention and very little of the available animal and retrospective clinical data have examined the role of statin therapy in established ALI. Indeed, we believe the present study to be one of the first evaluations of statin therapy in this setting. Consequently, though our data do not support statin administration for established ALI, we cannot rule out a role for statins in the prevention of ALI. Although the present study’s methodology precludes comment on this possibility (only patients meeting criteria for ALI were included in the database), both animal and retrospective clinical data do support a role in this setting [17–23]. Second, it is also possible the statin group was pre-selected as a more severely ill cohort of ALI patients as they developed lung injury despite statin therapy. Although our APACHE III and baseline SOFA scores do not support this hypothesis, our study design does not allow a more definitive comment on this specific possibility. A third potentially important factor in the explanation of our differing results regards dosing. Pre-clinical trials have generally administered much larger statin doses than used in clinical practice (up to 30 mg/kg) [9]. Clearly, different outcomes may be seen with such large variations in dosing regimens.
In addition to their potential for lung protection, statins have been associated with improved outcome in a variety of additional disease processes. Multiple studies have now shown improved outcomes in patients with bacteremia and/or sepsis [17–24]. Shouten et al. [16] recently published evidence of a renal protective effect in patients undergoing aortic surgery requiring a suprarenal aortic cross clamp. Patients with aneurysmal subarachnoid hemorrhage have also been shown to have improved neurologic outcomes with acute administration of statin therapy [25]. As ALI/ARDS is frequently associated with multi-organ failure, we hypothesized that statin administration might attenuate the progression of non-pulmonary organ dysfunction in patients with ALI/ARDS as well. Our results do not support this hypothesis. The ∆SOFA scores were not significantly different between statin users and non-users. We also failed to find differences in ICU or hospital mortality (Table 2). Though a non-statistically significant trend towards lower hospital mortality was noted in the statin cohort, we emphasize the discrepancy in hospital mortality between those with high propensity for statin administration and those with low propensity. Specifically, the mortality trend exists only in the high propensity cohort. Should a true effect on mortality exist, it should manifest regardless of the propensity for statin administration. We also note the recent work of Fernandez et al. [36] In this retrospective cohort study of critically ill patients, statin therapy did not appear protective as hospital mortality was higher in the statin cohort (61 vs. 42%).
Though the shorter ICU LOS for patients who received statin therapy is initially intriguing, this association was lost after adjustment for baseline characteristics and the propensity for statin administration. We believe the statin group may have had fewer ICU days simply because they were less ill at the time of meeting criteria for ALI (as indicated by their lower baseline SOFA scores) and were able to take enteral medications. Though it is possible statin users were less ill at baseline as a result of their statin use, our methodology does not allow for an assessment of this possibility. Again, the recent work of Fernandez et al. [36] would not appear to support this hypothesis. Finally, our methodology also precludes comment on a potential role for statin therapy in the prevention of ALI in high-risk subgroups with specific co-existing conditions such as sepsis or pneumonia. Previously reported trials would support a role for statins in this setting [17–24].
Conclusion
In this retrospective cohort study, we evaluated the role of statin therapy in patients with ALI/ARDS. We were not able to find evidence for a lung protective effect with statin administration. We were also unable to find evidence for prevention of associated organ dysfunction. At the present time, we cannot advocate the use of statin therapy as a means of attenuating lung injury or preventing multi-organ dysfunction in patients with established ALI or ARDS.
References
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R (1994) The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149:818–824
The Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342:1301–1308
Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL (2006) Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 354:2564–2575
Epstein M, Campese VM (2005) Pleiotropic effects of 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibitors on renal function. Am J Kidney Dis 45:2–14
Naidu BV, Woolley SM, Farivar AS, Thomas R, Fraga C, Mulligan MS (2003) Simvastatin ameliorates injury in an experimental model of lung ischemia–reperfusion. J Thorac Cardiovasc Surg 126:482–489
Pirat A, Zeyneloglu P, Aldemir D, Yucel M, Ozen O, Candan S, Arslan G (2006) Pretreatment with simvastatin reduces lung injury related to intestinal ischemia–reperfusion in rats. Anesth Analg 102:225–232
Jain R, DalNogare A (2006) Pharmacological therapy for acute respiratory distress syndrome. Mayo Clin Proc 81:205–212
Jacobson JR, Barnard JW, Grigoryev DN, Ma S-F, Tuder RM, Garcia JGN (2005) Simvastatin attenuates vascular leak and inflammation in murine inflammatory lung injury. Am J Physiol Lung Cell Mol Physiol 288:L1026–L1032
Yao HW, Mao LG, Zhu JP (2006) Protective effects of pravastatin in murine lipopolysaccharide-induced acute lung injury. Clin Exp Pharmacol Physiol 33:793–797
Le Manach Y, Coriat P, Collard CD, Riedel B (2008) Statin therapy within the perioperative period. Anesthesiology 108:1141–1146
Poldermans D, Bax JJ, Kertai MD, Krenning B, Westerhout CM, Schinkel AFL, Thomson IR, Lansberg PJ, Fleisher LA, Klein J, van Urk H, Roelandt JRTC, Boersma E (2003) Statins are associated with a reduced incidence of perioperative mortality in patients undergoing major noncardiac vascular surgery. Circulation 107:1848–1851
Lindenauer PK, Pekow P, Wang K, Gutierrez B, Benjamin EM (2004) Lipid-lowering therapy and in-hospital mortality following major noncardiac surgery. JAMA 291:2092–2099
Durazzo AES, Machado FS, Ikeoka DT, De Bernoche C, Monachini MC, Puech-Leao P, Caramelli B (2004) Reduction in cardiovascular events after vascular surgery with atorvastatin: a randomized trial. J Vasc Surg 39:967–975
O’Neil-Callahan K, Katsimaglis G, Tepper MR, Ryan J, Mosby C, Ioannidis JP, Danias PG (2005) Statins decrease perioperative cardiac complications in patients undergoing noncardiac vascular surgery: The Statins for Risk Reduction in Surgery (StaRRS) study. J Am Coll Cardiol 45:336–342
Sukhija R, Bursac Z, Kakar P, Fink L, Fort C, Satwani S, Aronow WS, Bansal D, Mehta JL (2008) Effect of statins on the development of renal dysfunction. Am J Cardiol 101:975–979
Schouten O, Kok NFM, Boersma E, Bax JJ, Feringa HHH, Vidakovic R, Statius van Eps RG, van Sambeek MRHM, Poldermans D (2006) Effects of statins on renal function after aortic cross clamping during major vascular surgery. Am J Cardiol 97:1383–1385
Pruefer D, Makowski J, Schnell M, Buerke U, Dahm M, Oelert H, Sibelius U, Grandel U, Grimminger F, Seeger W, Meyer J, Darius H, Buerke M (2002) Simvastatin inhibits inflammatory properties of Staphylococcus aureus α-toxin. Circulation 106:2104–2110
Yasuda H, Yuen PS, Hu X, Zhou H, Star RA (2006) Simvastatin improves sepsis-induced mortality and acute kidney injury via renal vascular effects. Kidney Int 69:1535–1542
Almog Y (2003) Statins, inflammation, and sepsis: hypothesis. Chest 124:740–743
Almog Y, Shefer A, Novack V, Maimon N, Barski L, Eizinger M, Friger M, Zeller L, Danon A (2004) Prior statin therapy is associated with a decreased rate of severe sepsis. Circulation 110:880–885
Hackam DG, Mamdani M, Li P, Redelmeier DA (2006) Statins and sepsis in patients with cardiovascular disease: a population-based cohort analysis. Lancet 367:413–418
Kruger P, Fitzsimmons K, Cook D, Jones M, Nimmo G (2006) Statin therapy is associated with fewer deaths in patients with bacteraemia. Intensive Care Med 32:75–79
Merx MW, Liehn EA, Janssens U, Lütticken R, Schrader J, Hanrath P, Weber C (2004) HMG-CoA reductase inhibitor simvastatin profoundly improves survival in a murine model of sepsis. Circulation 109:2560–2565
Gao F, Linhartova L, McD Johnston A, Thickett DR (2008) Statins and sepsis. Br J Anaesth 100:288–298
Tseng M-Y, Czosnyka M, Richards H, Pickard JD, Kirkpatrick PJ (2005) Effects of acute treatment with pravastatin on cerebral vasospasm, autoregulation, and delayed ischemic deficits after aneurysmal subarachnoid hemorrhage: a phase II randomized placebo-controlled trial. Stroke 36:1627–1632
Nassief A, Marsh JD (2008) Statin therapy for stroke prevention. Stroke 39:1042–1048
Stapleton RD, Wang BM, Hudson LD, Rubenfeld GD, Caldwell ES, Steinberg KP (2005) Causes and timing of death in patients with ARDS. Chest 128:525–532
Montgomery AB, Stager MA, Carrico CJ, Hudson LD (1985) Causes of mortality in patients with the adult respiratory distress syndrome. Am Rev Respir Dis 132:485–489
Yilmaz M, Iscimen R, Keegan MT, Vlahakis NE, Afessa B, Hubmayr RD, Gajic O (2007) Six-month survival of patients with acute lung injury: prospective cohort study. Crit Care Med 35:2303–2307
Ferreira FL, Bota DP, Bross A, Melot C, Vincent J-L (2001) Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA 286:1754–1758
Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, Sirio CA, Murphy DJ, Lotring T, Damiano A (1991) The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest 100:1619–1636
Gueler F, Rong S, Park JK, Fiebeler A, Menne J, Elger M, Mueller DN, Hampich F, Dechend R, Kunter U, Luft FC, Haller H (2002) Postischemic acute renal failure is reduced by short-term statin treatment in a rat model. J Am Soc Nephrol 13:2288–2298
Yokota N, O’Donnell M, Daniels F, Burne-Taney M, Keane W, Kasiske B, Rabb H (2003) Protective effect of HMG-CoA reductase inhibitor on experimental renal ischemia–reperfusion injury. Am J Nephrol 23:13–17
Laufs U, Liao JK (1998) Post-transcriptional regulation of endothelial nitric oxide synthase mRNA stability by Rho GTPase. J Biol Chem 273:24266–24271
Jacobson JR, Dudek SM, Singleton PA, Kolosova IA, Verin AD, Garcia JGN (2006) Endothelial cell barrier enhancement by ATP is mediated by the small GTPase Rac and cortactin. Am J Physiol Lung Cell Mol Physiol 291:L289–L295
Fernandez R, De Pedro VJ, Artigas A (2006) Statin therapy prior to ICU admission: protection against infection or a severity marker? Intensive Care Med 32:160–164
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
134_2009_1421_MOESM2_ESM.doc
Table E2. Patient outcome in the subgroup of statin users whose therapy was continued during the hospitalization (DOC 81kb)
134_2009_1421_MOESM3_ESM.doc
Table E3. Multivariate analysis of intensive care unit length of stay in the subgroup of statin users whose therapy was continued in the hospital (DOC 57kb)
Rights and permissions
About this article
Cite this article
Kor, D.J., Iscimen, R., Yilmaz, M. et al. Statin administration did not influence the progression of lung injury or associated organ failures in a cohort of patients with acute lung injury. Intensive Care Med 35, 1039–1046 (2009). https://doi.org/10.1007/s00134-009-1421-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-009-1421-8