Abstract
Background
Monitoring CO2 levels in preterm infants receiving mechanical ventilation is designed to avoid the harmful consequences of hypocapnia or hypercapnia. Capnography is of questionable accuracy for monitoring PCO2 in preterm infants.
Objectives
To determine the accuracy of sidestream capnography in ventilated preterm infants by comparing end-tidal carbon dioxide (EtCO2) values to mixed venous carbon dioxide pressure (PvCO2) and to transcutaneous carbon dioxide pressure (TcPCO2).
Methods
Simultaneous recordings of EtCO2, TcPCO2 and PvCO2 in 37 ventilated preterm infants. The PvCO2–EtCO2 gradient was calculated. The Bland–Altman technique and the intra-class correlation coefficient (ICC) were used to assess agreement between methods. The area under the curve (AUC) was calculated.
Results
Ninety-nine EtCO2/PvCO2 pairs were studied from 37 preterm infants with a mean gestational age of 27.7 ± 1.9 weeks and a mean birth weight of 1,003 ± 331 g. The mean PvCO2–EtCO2 gradient was 11.2 ± 8.0 mmHg, and the ICC was 0.28. The mean PvCO2–TcPCO2 gradient was 0 ± 7.8 mmHg, and the ICC was 0.78. AUCs for EtCO2 and TcPCO2 were similar in detecting high or low PvCO2.
Conclusion
Despite an insufficient correlation between EtCO2 and PvCO2, capnography was able to detect low and high CO2 warning levels with a similar efficacy to that of TcPCO2, and may therefore be of clinical interest.
Similar content being viewed by others
Introduction
Control of blood carbon dioxide (CO2) levels is of utmost importance in ventilated preterm infants, as both low and high arterial pressures of CO2 (PaCO2) and PaCO2 fluctuations may result in pulmonary and cerebral complications [1–4]. However, the invasive techniques used to monitor PaCO2 present several shortcomings, including blood losses, sepsis and thrombosis [5]. Repeated arterial puncture is painful, and crying can modify PaCO2 values. Noninvasive continuous monitoring methods are therefore desirable. The noninvasive technique most widely used in premature infants is transcutaneous CO2 monitoring (TcPCO2). TcPCO2 values are higher than those of PaCO2, but a good correlation is observed between the two methods. TcPCO2 reduces the need for blood gas samples and yields useful information on CO2 trends [6]. However, TcPCO2, which may cause skin burns in extremely preterm infants, requires very careful calibration and nursing procedures, and is unreliable during periods of hemodynamic instability [7]. Capnography, the noninvasive technique for monitoring CO2 from the airway, is accurate and widely used in both intubated and non-intubated adults and children. In mechanically ventilated preterm infants, mainstream capnography [8] and, more recently, low-flow sidestream technology [9, 10], have been evaluated, but the question of whether capnography is sufficiently accurate in this patient population has not yet been resolved [9, 11, 12]. The objective of this study was to evaluate the accuracy of low-flow sidestream expired CO2 monitoring in ventilated preterm infants by comparing end-tidal carbon dioxide (EtCO2) values to mixed venous carbon dioxide pressure (PvCO2) and to TcPCO2.
Methods
Patient population
Very low birth weight (VLBW; <1,500 g) infants admitted to the Service de Médecine Néonatale, Groupe Hospitalier Cochin-Saint Vincent de Paul in Paris, France, from January to October 2007 were eligible for inclusion in the study if they met the following criteria: need for mechanical ventilation via an endotracheal tube, indwelling central venous access (umbilical venous catheter), no need for positive inotropic agents and absence of congenital heart disease. Mechanical ventilation was performed using pressure-limited, time-cycled ventilators (Babylog 8000®, Dräger Medical and VIP Bird®, Viasys Healthcare) in a synchronized mode of intermittent mandatory ventilation (SIMV). Using the Babylog 8000® ventilator, the ventilator flow probe calculated the air leak around the uncuffed endotracheal tube, based on the difference detected between exhaled and inhaled volumes. The air leak was estimated visually on the VIP Bird® ventilator screen, based on the difference between expiratory and inspiratory flow rates. Since air leak affects the accuracy of EtCO2 measurements, those measurements performed with calculated air leaks >30% or estimated air leaks >one-third of inhaled volume were excluded from the study (seven EtCO2 measurements). All infants were studied lying supine [13], in a quiet state. The study was approved by the individual Institutional Review Boards, and parental consent was obtained.
Blood sampling from central venous catheter
In agreement with the unit guidelines, blood sampling and fluid infusions for VLBW infants were performed using an umbilical venous, rather than arterial catheter, during the first few days of life. Appropriate catheter placement was in the inferior vena cava, close to the junction with the right atrium. PvCO2 was used as a proxy for the gold standard PaCO2. Good correlation has been demonstrated between PvCO2 and PaCO2 in adults [14, 15] and children [16–18]. Blood gases were measured whenever deemed necessary by the attending neonatologist.
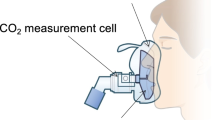
End-tidal carbon dioxide monitoring
Exhaled CO2 was continuously monitored using a commercially available Capnostream™20 (Oridion Medical Inc, Needham, MA), which utilizes low-flow sidestream (Microstream™) sampling technology [19]. The CO2 adapter (<0.5 ml dead space) is placed immediately between the endotracheal tube and the ventilator flow probe. The capnograph collects a continuous sample of gas at a flow rate of 50 ml/min and records the instantaneous CO2 concentration every 40 ms. A 30-s EtCO2 measurement was obtained in each patient just before the PvCO2 sampling. During this 30-s period of EtCO2 measurement, minor fluctuations in EtCO2 were observed corresponding to normal respiratory variations. The median of the range obtained during the recording period was used to determine the EtCO2 value. Recordings were performed only when CO2 waveforms were deemed visually similar to those previously reported [9]. The printer speed was 25 mm/s. Each recording was performed simultaneously with collection of blood samples. Further waveform analysis was performed subsequently, based on the first five breaths of each 30-s recording. As each set of CO2 measurements can be used for up to 72 h, the number of EtCO2 samples in each patient was related to the number of blood samples performed in this time period. Because the end-tidal CO2 value is related to infant position, all measures were performed in the supine position [13] in a quiet state.
Waveform analysis
The major features of the CO2 waveform (capnogram) were analyzed visually on the paper recording (Fig. 1). The turning points in CO2 concentration were detected, corresponding to the start of inhalation and the end of exhalation that define each breath. Within a breath, the linear phases of the capnogram were identified, including the initial expiratory rise and the alveolar plateau. An acceptable EtCO2 waveform was represented by a triphasic shape (ascending, alveolar and descending phases). An adequate alveolar phase was necessary to validate the recording (only one EtCO2 recording was excluded for inadequate alveolar phase). The segments were measured manually with a ruler on the paper recordings. Mean duration of the alveolar plateau (± standard deviation) was calculated on the five selected respiratory cycles.
Time-based capnogram in a mechanically ventilated preterm infant showing phases A–E and take-off angle. AB inhalation trough, BC initial expiratory phase, CD alveolar phase, D end-tidal point corresponding to maximum exhalation of carbon dioxide (at the end of the alveolar phase), BD expiratory phase, DE initial inhalation phase, a take-off angle, AE respiratory cycle
Transcutaneous CO2 measurement
The Linde Microgas 7650 monitor (Kontron, USA) was used for TcPCO2 measurement. This device measures CO2 potentiometrically by determining the pH of an electrolyte solution within a hydrophilic spacer, which is placed on top of the sensing area. The spacer is covered by a highly gas-permeable, hydrophobic membrane. For study purposes, the temperature was set at 43°C, and barometric pressure was set at 750 mmHg. PCO2 temperature correction was set at auto, and the PCO2 metabolic constant was set at 5 mmHg. The spacer was placed on the thorax for each patient. Each preterm infant had the sensor timed out at 3 h to prevent skin injury. The double-sided adhesive ring was applied to the sensor. A small drop of contact gel was applied to the center of the sensor.
Statistical analysis
Agreement between PvCO2 and EtCO2 measures was assessed by the Bland–Altman method [20] and the intra-class correlation coefficient (ICC). The PvCO2–EtCO2 gradient was defined as the difference between simultaneous PvCO2 and EtCO2 measurements.
Univariate analysis of eight factors [birth weight, gestational age, mean airway pressure, respiratory distress syndrome (RDS), severe RDS, FiO2, alveolar phase, PvCO2] that may influence the gradient was performed, followed by multivariate linear regression analysis of those variables with a P-value <0.20 on univariate analysis. Severe RDS was defined as RDS requiring at least two instillations of exogenous surfactant.
Receiver-operating characteristic (ROC) curves were used to examine the performance characteristics of TcPCO2 and of EtCO2 for detection of low and high CO2 levels. The ROC curve is a plot of 1− specificity versus sensitivity for all cutoff values in the range of CO2 observed values. For each method, we estimated the area under the ROC curves (AUC) corresponding to the C statistic from the logistic regression model. AUC is used as a global index of test performance with an AUC = 0.5 indicating no discrimination ability and an AUC = 1 indicating perfect discrimination ability. An AUC >0.8 indicates good discrimination ability. We compared the AUC of the ROC curves obtained for TcPCO2 and EtCO2 measures by non-parametric tests. The threshold level for hypocapnia was defined as a PvCO2 below 45 mmHg and for hypercapnia as PvCO2 above 60 mmHg. These values, which roughly correspond to PaCO2 of 39 mmHg and 54 mmHg, provided a safety threshold to avoid pulmonary [1] and cerebral complications [21, 22]. We then determined the thresholds of EtCO2 values for obtaining the best combination of sensitivity and specificity for hypocapnia and hypercapnia. All tests were two-sided, and P values below 0.05 were considered to denote statistical significance. Statistical analyses were performed with SAS software package version 9 (SAS Institute, Cary, NC).
Results
Thirty-seven VLBW preterm infants were prospectively enrolled (19 males and 18 females). The mean birth weight was 1,003 ± 331 g (mean ± SD), and mean gestational age was 27.7 ± 1.9 weeks. The causes of intubation were RDS (36/37) and low Apgar scores (1/37). Preterm infants with RDS were treated by exogenous surfactant given prophylactically (14/36) or as rescue therapy (18/36). A median of two pairs of EtCO2 and PvCO2 measurements (range one to ten pairs) were performed at the median age of 1 day of life (range, 1 h to 3 days). Ninety-nine pairs were available for analysis. The clinical characteristics and ventilatory settings are listed in Table 1.
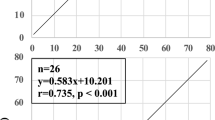
EtCO2 and PvCO2 correlation
The EtCO2 values were lower than the corresponding PvCO2 with a mean PvCO2–EtCO2 gradient = 11.2 ± 8.0 mmHg (PvCO2 = 49.0 ± 10.9 mmHg, EtCO2 = 37.8 ± 8.9 mmHg). The ICC for all pairs was 0.28. The gradient between EtCO2 and PvCO2 is illustrated in Fig. 2, where the difference is plotted against the mean of the two values.
Fifty-one PvCO2 measurements were situated between 45 and 60 mmHg, 35 measurements were below 45 mmHg, and 13 values were above 60 mmHg. When PvCO2 was above 60 mmHg, compared with below 60 mmHg, the PvCO2–EtCO2 gradient was higher (21.5 ± 5.9 mmHg vs. 9.6 ± 7, P < 0.0001).
Univariate analysis showed that four factors [birth weight (P = 0.05), FiO2 (P = 0.003), alveolar phase duration (P = 0.003) and PvCO2 (P < 0.0001)] influenced the PvCO2–EtCO2 gradient with P < 0.20. Multivariate linear regression was performed with these four factors and identified alveolar plateau duration and PvCO2 as independent factors influencing the gradient. The gradient increased with increasing PvCO2 and decreased with increasing alveolar plateau duration (Table 2). Alveolar phase >5 mm (0.2 s) improved the accuracy of EtCO2 values.
EtCO2 and TcPCO2 correlation
The mean TcPCO2-EtCO2 gradient was 11.2 ± 9.0 mmHg (TcPCO2 = 49.0 ± 12.4 mmHg, EtCO2 = 37.8 ± 8.9 mmHg). The ICC for all pairs was 0.30.
TcPCO2 and PvCO2 correlation
The mean PvCO2–TcPCO2 gradient was 0 ± 7.8 mmHg (PvCO2 = 49.0 ± 10.9 mmHg, TcPCO2 = 49.0 ± 12.4 mmHg). The ICC for all pairs was 0.78.
Hypercapnia and hypocapnia thresholds
All ninety-nine EtCO2/PvCO2 pairs were used to determine potential thresholds to be used as warnings levels for potential occurrence of hypocapnia or hypercapnia. The ROC curves for both TcPCO2 and EtCO2 are shown in Fig. 3. The AUC for EtCO2 was 0.81 (95% CI, 0.71–0.92) for high CO2 (>60 mmHg) and 0.89 (95%CI, 0.83–0.96) for low CO2 (<45 mmHg), indicating good discrimination ability. No significant difference was observed for the AUC of EtCO2 and TcPCO2 for high CO2 (P = 0.18) or low CO2 (P = 0.71). An EtCO2 value <34 mmHg had a sensitivity of 83% (95%CI, 75–90%) and a specificity of 86% (95%CI, 79–93%) for identifying PvCO2 below 45 mmHg. An EtCO2 value >44 mmHg had a sensitivity of 77% (95%CI, 69–85%) and a specificity of 78% (95%CI, 70–86%) for identifying PvCO2 above 60 mmHg.
Discussion
Low-flow sidestream end-tidal CO2 monitoring was assessed in mechanically ventilated preterm infants. Correlations between EtCO2 and PvCO2, and between EtCO2 and TcPCO2 were studied. Mean gradients of 11 mmHg were demonstrated between EtCO2 and PvCO2, and between EtCO2 and TcPCO2. A good correlation was observed between TcPCO2 and PvCO2, but not between EtCO2 and PvCO2 or between EtCO2 and TcPCO2. However, EtCO2 accurately identified high and low PvCO2 cutoffs that can be used as warnings signs to maintain PvCO2 within safety margins.
Capnography is a validated method for monitoring CO2 in ventilated adults and in healthy anesthetized infants [23, 24], and for confirming endotracheal tube position in adults, children and premature infants [25, 26]. The noninvasive nature of this technique is a major advantage for neonatal care. However, the accuracy and reliability of EtCO2 monitoring to predict PaCO2 in ventilated premature infants remains unclear [27]. Capnography has been found to be an accurate method for monitoring CO2 in ventilated preterm infants in some studies [8, 28], but not in others [11, 12].
Two capnographic technologies are available: mainstream and sidestream. Mainstream technology requires an adapter placed proximal to the endotracheal tube. Good correlations between PaCO2 and EtCO2, and mean gradient between 3.4 and 6.9 mmHg have been reported [8, 28–32]. However, linear relationships or correlation coefficients do not adequately assess the agreement between PaCO2 and EtCO2 [8, 28–30, 32]. Moreover, reported gradients may be clinically unacceptable. Sidestream technology uses an aspirating sample port on the side of the endotracheal tube. Conventional sidestream capnographs require a large sample cell and a high flow rate (150–200 ml/min). Microstream™ technology employs a sampling flow rate of 50 ml/min, approximately one-third that used by conventional sidestream systems. This low-flow rate reduces the competition for tidal volume and decrease condensation within the system. Because of the highly CO2-specific infrared source, the sample cell utilizes a much smaller volume (15 μl) that permits a low-flow rate without compromising response rate or accuracy. Also, the low-flow sidestream capnography attempts to overcome the limitations of mainstream technology applied to low birth weight infants by using both smaller sample volumes and smaller added dead space [9, 11, 12, 19]. However, in two studies performed in ventilated very preterm [11] and preterm [12] infants with lung disease, using low-flow sidestream capnography, a poor correlation was observed between EtCO2 and PaCO2. The changes in CO2 trends was assessed in only one of the two studies, which concluded that EtCO2 both underestimated CO2 levels in newborn infants with respiratory failure and did not reliably monitor trends in PaCO2 levels over time [12]. More recently, mainstream and sidestream technologies were compared in intubated preterm infants. Sidestream distal EtCO2 measurement provide both good correlation and agreement with PaCO2, and was more accurate than mainstream EtCO2 [10]. More accurate results have been reported in newborns without respiratory disease [9], and severity of lung disease was reported to affect the accuracy of EtCO2 [10]. Most studies did not calculate the ICC [8, 12, 28, 30].
In line with previous reports [11, 12], the present study showed a poor concordance between EtCO2 measurement and PvCO2 measurement (used to estimate PaCO2), as evaluated from the gradient, using the Bland and Altman technique and the ICC. Our ICC value of 0.28 is markedly lower than previously reported early in life [11]. Unsatisfactory reliability of sidestream capnography [12] may be due to technical limitations of end-tidal CO2 analysis in low birth weight infants with high respiratory rate, low tidal volume, and lack of alveolar plateau [33]. Our finding of a lower gradient when the alveolar phase increased supports this hypothesis. Other difficulties are due to the presence of parenchymal lung disease and ventilation perfusion mismatching, which results in alveolar CO2 underestimating PaCO2 [8, 12, 34]. Previous studies in newborn infants confirmed that the PaCO2–EtCO2 gradient was decreased in children with milder compared to more severe lung disease [10, 12, 30]. Our finding of an increased gradient in infants with a higher oxygen requirement and higher PvCO2 may be interpreted in a similar fashion.
Various waveform parameters influencing the PvCO2–EtCO2 gradient were analyzed: length of inspiratory phase, expiratory phase and alveolar phase. The alveolar plateau is the most relevant of these parameters, as it represents alveolar CO2, in contrast with the ascending phase, which represents gas mixing with dead space gas during initial expiration [9]. A long alveolar phase is necessary to reduce the PvCO2–EtCO2 gradient.
Despite the above-mentioned difficulties and limitations, predefined cutoff values for low (<45 mmHg) and high (>60 mmHg) PvCO2 could be detected using sidestream capnography, with good sensitivity and specificity. The cutoff values, corresponding to PaCO2 of 39 and 54 mmHg, were chosen as warning values rather than thresholds to define hypocapnia or hypercapnia. They are designed to provide the clinician with sufficient time to adapt ventilation parameters—if deemed necessary—in order to modify the CO2 trend and avoid development of true hypocapnia or hypercapnia (regardless of its definition), whose deleterious effects have been clearly established [1, 2, 21, 22].
The major limitation of the study is the use of venous (PvCO2) rather than PaCO2 as the reference. PvCO2 is also a proxy of PaCO2, but this choice was based on the fact that umbilical venous rather than arterial catheters are routinely used to monitor ventilation trends in our unit for safety purposes [5, 35]. Although not evaluated in ventilated preterm infants, PvCO2 correlated well with PaCO2 in adults receiving mechanical ventilation [14, 15] and in children receiving intensive care [16–18]. In our study, PvCO2 correlated well with TcPCO2 measurements (ICC = 0.78). TcPCO2 is known to accurately predict PaCO2 in neonates [36], suggesting that PvCO2 may also have a role as a proxy for PaCO2 trends. PvCO2 is 6 mmHg higher than PaCO2 in adults [37–39]. This difference may not be the same in the entire spectrum of PaCO2 and in all diseases [16, 18]. This difference must be taken into account when interpreting the mean PvCO2–EtCO2 gradient in this study and should not be directly compared to the bias used in studies using PaCO2.
Another limitation was the use of repeated measurements from the same patient. This allowed the collection of more pairs, but may have influenced the results due to interdependence of measurements.
We could not assess whether the ventilator flowmeter modified the EtCO2 measurement or whether sidestream capnography modified the reading of the ventilator flowmeter. However, Microstream™ technology uses flow sampling lower than previous devices, which limits the competition for tidal volume [19] and reduces a potential extra artificial air leak.
Finally, in preterm infants ventilated with uncuffed endotracheal tubes, leaks are commonly observed, which may influence the EtCO2 value. Therefore, we excluded EtCO2 recordings where a leak of more than 30% was detected. It is possible that lesser leaks may also have influenced the EtCO2 bias.
In conclusion, EtCO2 monitoring underestimated CO2 levels compared with venous CO2 measurements in mechanically ventilated newborn infants. The accuracy of EtCO2 monitoring decreased with decreasing alveolar plateau and increasing PvCO2. However, EtCO2 detected low and high PvCO2 and may therefore be useful for detecting CO2 warning levels, in order to avoid harmful episodes of hypocapnia or hypercapnia.
References
Garland JS, Buck RK, Allred EN, Leviton A (1995) Hypocarbia before surfactant therapy appears to increase bronchopulmonary dysplasia risk in infants with respiratory distress syndrome. Arch Pediatr Adolesc Med 149:617–622
Fujimoto S, Togari H, Yamaguchi N, Mizutani F, Suzuki S, Sobajima H (1994) Hypocarbia and cystic periventricular leukomalacia in premature infants. Arch Dis Child 71:F107–F110
Szymonowicz W, Yu VY, Wilson FE (1984) Antecedents of periventricular haemorrhage in infants weighing 1250 g or less at birth. Arch Dis Child 59:13–17
Fabres J, Carlo WA, Phillips V, Howard G, Ambalavanan N (2007) Both extremes of arterial carbon dioxide pressure and the magnitude of fluctuations in arterial carbon dioxide pressure are associated with severe intraventricular hemorrhage in preterm infants. Pediatrics 119:299–305
Hermansen MC, Hermansen MG (2005) Intravascular catheter complications in the neonatal intensive care unit. Clin Perinatol 32:141–156 vii
Greenhough A (2003) Neonatal respiratory disorders. Arnold, New York, pp 227–235
Bhat R, Kim WD, Shukla A, Vidyasagar D (1981) Simultaneous tissue pH and transcutaneous carbon dioxide monitoring in critically ill neonates. Crit Care Med 9:744–749
Rozycki HJ, Sysyn GD, Marshall MK, Malloy R, Wiswell TE (1998) Mainstream end-tidal carbon dioxide monitoring in the neonatal intensive care unit. Pediatrics 101:648–653
Hagerty JJ, Kleinman ME, Zurakowski D, Lyons AC, Krauss B (2002) Accuracy of a new low-flow sidestream capnography technology in newborns: a pilot study. J Perinatol 22:219–225
Kugelman A, Zeiger-Aginsky D, Bader D, Shoris I, Riskin A (2008) A novel method of distal end-tidal CO2 capnography in intubated infants: comparison with arterial CO2 and with proximal mainstream end-tidal CO2. Pediatrics 122:e1219–e1224
Aliwalas LL, Noble L, Nesbitt K, Fallah S, Shah V, Shah PS (2005) Agreement of carbon dioxide levels measured by arterial, transcutaneous and end tidal methods in preterm infants ≤28 weeks gestation. J Perinatol 25:26–29
Tingay DG, Stewart MJ, Morley CJ (2005) Monitoring of end tidal carbon dioxide and transcutaneous carbon dioxide during neonatal transport. Arch Dis Child Fetal Neonatal Ed 90:F523–F526
Kugelman A, Bilker A, Bader D, Cohen A, Tirosh E (2002) Sidestream end-tidal capnometry as related to infant’s position and maturation. Acta Paediatr 91:869–873
Chu YC, Chen CZ, Lee CH, Chen CW, Chang HY, Hsiue TR (2003) Prediction of arterial blood gas values from venous blood gas values in patients with acute respiratory failure receiving mechanical ventilation. J Formos Med Assoc 102:539–543
Malinoski DJ, Todd SR, Slone S, Mullins RJ, Schreiber MA (2005) Correlation of central venous and arterial blood gas measurements in mechanically ventilated trauma patients. Arch Surg 140:1122–1125
Yildizdas D, Yapicioglu H, Yilmaz HL, Sertdemir Y (2004) Correlation of simultaneously obtained capillary, venous, and arterial blood gases of patients in a paediatric intensive care unit. Arch Dis Child 89:176–180
Tobias JD, Connors D, Strauser L, Johnson T (2000) Continuous pH and Pco2 monitoring during respiratory failure in children with the Paratrend 7 inserted into the peripheral venous system. J Pediatr 136:623–627
Bilan N, Behbahan AG, Khosroshahi AJ (2008) Validity of venous blood gas analysis for diagnosis of acid–base imbalance in children admitted to pediatric intensive care unit. World J Pediatr 4:114–117
Colman Y, Krauss B (1999) Microstream capnograpy technology: a new approach to an old problem. J Clin Monit Comput 15:403–409
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Okumura A, Hayakawa F, Kato T, Itomi K, Maruyama K, Ishihara N, Kubota T, Suzuki M, Sato Y, Kuno K, Watanabe K (2001) Hypocarbia in preterm infants with periventricular leukomalacia: the relation between hypocarbia and mechanical ventilation. Pediatrics 107:469–475
Kaiser JR, Gauss CH, Pont MM, Williams DK (2006) Hypercapnia during the first 3 days of life is associated with severe intraventricular hemorrhage in very low birth weight infants. J Perinatol 26:279–285
Badgwell JM, Heavner JE (1991) End-tidal carbon dioxide pressure in neonates and infants measured by aspiration and flow-through capnography. J Clin Monit 7:285–288
McDonald MJ, Montgomery VL, Cerrito PB, Parrish CJ, Boland KA, Sullivan JE (2002) Comparison of end-tidal CO2 and Paco2 in children receiving mechanical ventilation. Pediatr Crit Care Med 3:244–249
Wyllie J, Carlo WA (2006) The role of carbon dioxide detectors for confirmation of endotracheal tube position. Clin Perinatol 33:111–119 vii
Salthe J, Kristiansen SM, Sollid S, Oglaend B, Soreide E (2006) Capnography rapidly confirmed correct endotracheal tube placement during resuscitation of extremely low birthweight babies (<1000 g). Acta Anaesthesiol Scand 50:1033–1036
Molloy EJ, Deakins K (2006) Are carbon dioxide detectors useful in neonates? Arch Dis Child Fetal Neonatal Ed 91:F295–F298
Wu CH, Chou HC, Hsieh WS, Chen WK, Huang PY, Tsao PN (2003) Good estimation of arterial carbon dioxide by end-tidal carbon dioxide monitoring in the neonatal intensive care unit. Pediatr Pulmonol 35:292–295
Meredith KS, Monaco FJ (1990) Evaluation of a mainstream capnometer and end-tidal carbon dioxide monitoring in mechanically ventilated infants. Pediatr Pulmonol 9:254–259
Sivan Y, Eldadah MK, Cheah TE, Newth CJ (1992) Estimation of arterial carbon dioxide by end-tidal and transcutaneous PCO2 measurements in ventilated children. Pediatr Pulmonol 12:153–157
Amuchou Singh S, Singhal N (2006) Dose end-tidal carbon dioxide measurement correlate with arterial carbon dioxide in extremely low birth weight infants in the first week of life? Indian Pediatr 43:20–25
Bhat YR, Abhishek N (2008) Mainstream end-tidal carbon dioxide monitoring in ventilated neonates. Singapore Med J 49:199–203
Thompson JE, Jaffe MB (2005) Capnographic waveforms in the mechanically ventilated patient. Respir Care 50:100–108 discussion 108-109
Scarpelli E (1975) Pulmonary physiology of the fetus newborn and child, 3rd edn. Lea and Febiger, Philadelphia, pp 18–20
Messer J, Livolsi A, Escande B, Moriette G, Desfrere L (2002) Umbilical artery catheters: more dangerous than useful? Eur J Pediatr 161:130 author reply 131
Whitehead MD, Halsall D, Pollitzer MJ, Delpy DT, Parker D, Reynolds EO (1980) Transcutaneous estimation of arterial PO2 and PCO2 in newborn infants with a single electrochemical sensor. Lancet 1:111–114
Comroe J (1979) Physiology of respiration. Year Book Medical Publishers, Chicago, pp 8–21
Vallee F, Vallet B, Mathe O, Parraguette J, Mari A, Silva S, Samii K, Fourcade O, Genestal M (2008) Central venous-to-arterial carbon dioxide difference: an additional target for goal-directed therapy in septic shock? Intens Care Med 34:2218–2225
Adrogue HJ, Rashad MN, Gorin AB, Yacoub J, Madias NE (1989) Assessing acid–base status in circulatory failure. Differences between arterial and central venous blood. N Engl J Med 320:1312–1316
Acknowledgments
The authors gratefully acknowledge the technical assistance of Mr. Ozenne, Deltamedics, France, and the contribution of Anthony Saul, M.B. B.S., for stylistic review of the manuscript. Deltamedics, France, provided the technical support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lopez, E., Grabar, S., Barbier, A. et al. Detection of carbon dioxide thresholds using low-flow sidestream capnography in ventilated preterm infants. Intensive Care Med 35, 1942–1949 (2009). https://doi.org/10.1007/s00134-009-1647-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-009-1647-5