Abstract
Purpose
To determine whether, during mechanical ventilation, an optimal positive end-expiratory pressure (PEEP) can be identified by measurement of regional tidal volume and compliance [V T(reg), C RS(reg)].
Methods
Sixteen anaesthetized intubated neonatal piglets underwent a stepwise vital capacity manoeuvre performed during pressure control ventilation, with 5 cmH2O PEEP increments to 25 cmH2O, and decrements to 0 cmH2O. Peak inflating pressure was 10 cmH2O above PEEP throughout. The manoeuvre was performed in the normal lung, after repeated saline lavage and after surfactant therapy. Global V T and C RS were measured at the airway opening; V T(reg) and C RS(reg) were measured in the ventral, medial and dorsal lung using electrical impedance tomography (EIT).
Results
Most uniform distribution of regional tidal ventilation was noted during PEEP decrements after lung recruitment, at varying PEEP levels. In the lavaged and surfactant-treated lung the PEEP optimal for ventilation distribution was also associated with highest mean V T(reg) [lavaged: 95 ± 9.3% of maximum, mean ± standard deviation (SD); surfactant-treated: 92 ± 17%] and global V T (96 ± 10%; 96 ± 15%). Regional C RS plots clearly demonstrated co-existent ventral overdistension and dorsal recruitment, particularly during PEEP increments; whereas during PEEP decrements, peak C RS(reg) values showed considerable interregional concordance [e.g. peak C RS(reg) in the lavaged left lung; ventral: 0.017 ± 0.0036; medial: 0.016 ± 0.0054; dorsal: 0.017 ± 0.0073 cmH2O−1; P = 0.98, analysis of variance (ANOVA)].
Conclusions
After lung recruitment, a PEEP level can be identified by EIT at which tidal ventilation is uniformly distributed, with associated concordance in compliance between lung regions. Bedside monitoring of regional tidal ventilation and compliance using EIT may thus aid in PEEP selection.
Similar content being viewed by others
Introduction
A body of theoretical and experimental evidence indicates that mechanical ventilation of the diseased lung is best applied using an open lung approach [1, 2]. Titration of positive end-expiratory pressure (PEEP) after maximal lung expansion allows tidal ventilation to be applied near the deflation limb of the pressure–volume (P–V) envelope [3], and is associated with best compliance and gas exchange [4, 5], less repetitive recruitment and derecruitment of lung units [6], and reduction in ventilator-induced lung injury [7]. Benefits have also been noted in animal models equivalent in size to term human newborns [3, 8]. Clinical trials of open lung ventilation have suggested a benefit of this strategy in adults with acute lung injury [9]; similar trials have yet to be conducted in neonatal or paediatric subjects.
Open lung ventilation requires firstly the application of sufficient recruiting pressure to inflate atelectatic lung units [10, 11], and secondly the selection of a PEEP such that recruitment is maintained during subsequent tidal ventilation [2, 10]. PEEP selection in this setting is frequently made difficult by inhomogeneity in P–V behaviour in the diseased lung [12–14], not detectable by global lung indices such as gas exchange or compliance that have historically been used to guide PEEP titration [15, 16].
It is becoming clear that bedside recordings using electrical impedance tomography (EIT) afford an opportunity to monitor regional lung function in ventilated subjects. EIT has allowed demonstration of regional filling characteristics suggestive of ventilation inhomogeneity [17], and a shift of the regional distribution of tidal ventilation after recruitment [4, 18, 19], derecruitment [18, 20] or surfactant administration [19]. During PEEP trials in the injured lung, regional tidal ventilation has been found to alter considerably with PEEP increments and decrements, with regional changes not being mirrored in global lung behaviour [5]. Preliminary observations of regional heterogeneity of compliance measured by EIT have also been made in two human subjects [21], but systematic data on changes in regional lung compliance during PEEP titration are lacking.
This study examines indices of regional lung function during a stepwise vital capacity manoeuvre used in the normal, injured and surfactant-treated neonatal lung. We aimed to record the course of regional tidal volume and compliance [V T(reg), C RS(reg)] during such a manoeuvre, and to compare the changes seen with concomitant alterations in global V T and C RS. We hypothesised that a PEEP level would be identifiable at which distribution of regional tidal ventilation was optimised, and/or C RS(reg) values concordant between lung regions.
Materials and methods
The experimental methods used in this study were approved by the university and state committee for animal care, and adhered to the guidelines on animal experimentation. The methods for animal preparation, ventilation and lung lavage have been described previously [19]. Briefly, newborn piglets were anaesthetized with ketamine (35 mg/kg i.m.), tracheotomized and mechanically ventilated in supine position with PEEP of 5 cmH2O, V T of 10 mL/kg, respiratory rate of 30–40 breaths/min and FiO2 of 1.0 (Galileo Gold; Hamilton Medical, Switzerland). Intravenous and intra-arterial catheters were placed, and blood pressure was monitored continuously. Anaesthesia was maintained with intravenous infusions of fentanyl (20 μg/kg/h) and midazolam (0.3 mg/kg/h), and muscle relaxation with infusion of pancuronium bromide (0.3 mg/kg/h). Airway opening pressure and airflow were monitored (Florian respiratory monitor; Acutronic Medical Systems, Zug, Switzerland), and PaO2 and PaCO2 were recorded with an indwelling arterial blood gas electrode (Paratrend 7; Diametrics Medical, High Wycombe, UK). Changes in electrical impedance within the lung were recorded using 16 electrodes placed around the chest at the level of the sixth parasternal intercostal space (Goe-MF II EIT system; Viasys Healthcare, Höchberg, Germany) [19]. EIT measurements were performed with an electrical current of 5 mArms and 70 kHz and a scan rate of 13 Hz. From these signals, changes in V T(reg), C RS(reg) and end-expiratory lung volume [EELV(reg)] were derived as described below.
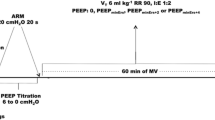
The experimental protocol consisted of a stepwise vital capacity manoeuvre during pressure control ventilation (Fig. 1a), with PEEP increased in 5 cmH2O increments to a maximum of 25 cmH2O, and then gradually returned to zero. Each PEEP level was held for around 15 s, and tidal ventilation continued throughout with an inflating pressure (∆P, equal to peak pressure minus PEEP) of 10 cmH2O, inspiratory time of 0.65 s, respiratory rate of 20/min and FiO2 of 1.0. Signals from the airway opening and EIT device were recorded throughout. In each animal, the vital capacity manoeuvre was performed in (a) the normal lung, (b) 1 h after saline lavage and (c) 1 h after surfactant treatment (100 mg/kg Curosurf; Nycomed, Munich, Germany). Surfactant was administered with or without applied PEEP, and followed by ventilation with or without recruitment, in accordance with the protocol of a parallel study focussing on the spatial distribution of ventilation after surfactant treatment [19]. Further description of the lavage procedure, ventilation between manoeuvres and details of the surfactant and post-surfactant randomisation groups can be found in the Electronic Supplementary Material (ESM). Ventilatory management was identical before each manoeuvre, with a period of pressure control ventilation, followed by disconnection to ambient pressure immediately before commencing the manoeuvre.
Experimental and analytical methods. a Airway pressure manipulation over time during the stepwise vital capacity manoeuvre. Each PEEP increment was held for ~15 s, and included at least four tidal breaths. b Example of cross-sectional image obtained using EIT, including a grid indicating the division of the L and R lung into three regions in the anteroposterior axis (V ventral, M medial, D dorsal). c Tracing of regional lung volume change during the entire manoeuvre, derived from EIT impedance change expressed relative to the manoeuvre onset (rel. ∆Z, dimensionless units). Animal 16, surfactant-treated lung, R ventral region. d Pressure–volume curve (grey line) derived from tracings in a and c, with the final breath at each PEEP level indicated (black lines). VC vital capacity, defined as the total change in rel. ∆Z seen to occur with PEEP increments after initial disconnection to ambient pressure
During offline processing, in the cross-sectional EIT images the lung was divided into ventral, medial and dorsal regions with equidistant gridlines (Fig. 1b). For each region a tracing of lung volume for the entire manoeuvre was made from the EIT impedance change relative to the manoeuvre onset (rel. ∆Z, dimensionless units [22]) (Fig. 1c). A P–V curve was thus derived, and vital capacity was measured (Fig. 1d). The final tidal breath at each PEEP level was selected (Fig. 1d), and further analysis of tidal ventilation and compliance trends performed on this subset of ventilator breaths. Global tidal ventilation loops were derived from the airway opening data, zeroed at breath onset, and also normalised to the maximum global V T observed in the final breath subset. Global C RS was calculated from the airway opening pressure, flow and integrated volume signals using multiple linear regression [23], referenced to body weight.
Regional tidal ventilation loops were derived for the final breath subset, with volume expressed as rel. ∆Z, zeroed at loop onset and normalised to the maximum tidal rel. ∆Z observed in that region. For each animal, the degree of uniformity of regional ventilation was expressed as the coefficient of variation (CV = SD/mean) amongst the six normalised V T(reg) values at each PEEP level. The PEEP level at which the CV was minimised was considered the optimum PEEP for equalising distribution of ventilation; the regional and global tidal volumes associated with this PEEP were noted. The PEEP level at which V T(reg) (mean of six values) and global V T were maximised was also determined. C RS(reg) for the final breath at each PEEP level was calculated, where C RS(reg) = [V T(reg)/VC(reg)/∆P], with units of cmH2O−1. VC(reg) was defined as the total change in impedance seen to occur within the region throughout the manoeuvre (Fig. 1d). Finally, EELV(reg), the rel. ∆Z value at end-expiration in the final breath at each PEEP step, was determined. EELV(reg) values were normalised to VC(reg) to allow meaningful intergroup comparisons, and were plotted as a regional P–V curve. Hysteresis was defined as the area enclosed by the inflation and deflation limbs of this curve.
Statistical methods
Data are presented as mean and standard deviation unless otherwise stated. One-way ANOVA with Duncan’s post hoc testing was used for comparison of V T, C RS and hysteresis area, both between lung regions and between different lung states (normal, lavaged, surfactant-treated) during the experimental protocol. EELV(reg) data at sequential PEEP levels during inflation and deflation were similarly compared using two-way ANOVA for repeated measures. P values <0.05 were considered significant.
Results
Sixteen newborn piglets (2.3 ± 0.28 kg, mean ± SD) were studied, with induction of lung injury requiring 8.6 ± 1.9 episodes of saline lavage. PaO2 values prior to the vital capacity manoeuvre were 500 ± 69, 66 ± 33 and 160 ± 77 mmHg in the normal, lavaged and surfactant-treated lung, respectively. Corresponding values for PaCO2 were 47 ± 8.0, 62 ± 11 and 73 ± 17 mmHg. During the manoeuvre, oxygenation was noted to be stable in the normal lung, whereas in both the lavaged and surfactant-treated lung PaO2 rose as the lung was inflated, but with a delay of around 60 s, making any correlations with lung volume changes unreliable. During the inflation sequence, mean blood pressure decreased to 61 ± 10, 65 ± 20 and 60 ± 12 mmHg in the normal, lavaged and surfactant-treated lung, respectively, with the greatest fall in the normal lung (15 ± 9.0 mmHg below baseline). There was return to baseline blood pressure values by the end of the manoeuvre in all cases.
Representative global and regional tidal ventilation P–V loops from the final breath at each PEEP level in the lavaged lung are shown in Fig. 2. The normalised V T(reg) plots (Fig. 2b, c) demonstrate: (a) the paucity of ventilation in the dorsal lung regions with initial PEEP increments, (b) the diminution of tidal ventilation to the ventral then medial and finally dorsal regions as inflation nears maximum, (c) the augmentation of V T(reg) in all regions with PEEP decrements and finally (d) the reduction of V T(reg) in all regions as PEEP reaches zero. Distribution of V T(reg) is most uniform at a decremental PEEP of 5 cmH2O (Fig. 2), with considerable heterogeneity of regional tidal ventilation at other PEEP levels.
Normalised tidal ventilation loops. Representative global and regional tidal ventilation pressure–volume loops from the final breath at each PEEP level in the lavaged lung (animal 11), normalised to the maximum V T noted throughout the manoeuvre, and zeroed at loop onset. Raw data from which these normalised loops are derived are shown in Fig. E1 (ESM). a Normalised global tidal ventilation measured at the airway opening (% maximum V T). b R lung regional ventilation (light grey ventral, dark grey medial, black dorsal). c L lung regional ventilation (same colour scheme). Near-complete uniformity of regional ventilation is seen at a decremental PEEP of 5 cmH2O (CV = 0.55%), at which both V T(reg) and global V T are at their peak
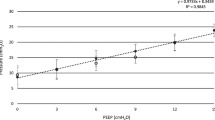
The decremental PEEP associated with most uniform distribution of tidal ventilation is plotted for each animal in Fig. 3. In the lavaged and surfactant-treated lung, PEEP levels at which ventilation distribution, mean V T(reg) and global V T were optimised were very similar (Fig. 3), with concordance for all three indices in 11 and 15 of the 16 animals, respectively. In the lavaged lung, mean V T(reg) was 95 ± 9.3% of maximum and global V T was 96 ± 10% at PEEP optimal for ventilation distribution. Corresponding values in the surfactant-treated lung were 92 ± 17% and 96 ± 15%. Data in the 16 surfactant-treated animals were pooled for this and subsequent analyses, as no systematic differences between surfactant administration groups or post-surfactant recruitment groups were found. The only difference noted was a higher normalised V T(reg) in the three lung regions at an incremental PEEP of 10 cmH2O in the post-surfactant recruitment group (P < 0.05, t-test).
Optimal PEEP levels during PEEP decrements. Plot of PEEP level identified to be optimal for three lung indices measured in the final breath during PEEP decrements. Individual data points (number of multiple observations indicated where applicable). NL normal lung, LL lavaged lung, ST surfactant-treated lung. Diamonds PEEP at which distribution of tidal ventilation most uniform [i.e. lowest CV for six normalised V T(reg) values]. Triangles PEEP associated with highest mean V T(reg), using the mean of the six normalised V T(reg) values from each of the lung regions. Circles PEEP associated with highest global V T
Global C RS plots show a peak during PEEP decrements, with its position shifting toward higher PEEP levels after lung injury (Fig. E2, ESM). Compared with the normal lung, peak global C RS was substantially reduced after lung lavage, as expected, with 60% improvement after surfactant treatment (Table 1). Regional compliance plots (Fig. 4 and Fig. E3, ESM) highlight the complexity of lung mechanical behaviour during the manoeuvre, with, in the lavaged and surfactant-treated lung, evidence of co-existing ventral overdistension and dorsal recruitment during PEEP increments to maximal inflation (Fig. 4). With PEEP decrements, C RS(reg) rose to a peak, followed by variable degrees of derecruitment, especially dorsally, as PEEP reached zero. In all cases there was a significant reduction in peak C RS(reg) after lung lavage, but only for the right medial and dorsal regions was there a significant improvement in C RS(reg) after surfactant treatment (Table 1). Whereas in the normal lung peak C RS(reg) values were higher in the ventral regions, in both the lavaged and the surfactant-treated lung peak C RS(reg) was very similar across the anteroposterior axis (Table 1), pointing once again to the relative uniformity of regional mechanical behaviour during PEEP decrements in the injured lung.
Regional compliance, for the final breath at each PEEP level. Mean and SD for all animals, R lung data only [L lung C RS(reg) values shown in Fig. E3, ESM]. a Normal lung, b lavaged lung, c surfactant-treated lung. Note different Y-axis scales. Open bars ventral, grey bars medial, black bars dorsal. See text for further details of the calculation of regional compliance. Ventral overdistension and dorsal recruitment are seen to co-exist during PEEP increments. In the surfactant-treated lung (c), from PEEP 0 cmH2O to PEEP 15 cmH2O there is a 48% reduction in ventral C RS(reg) (indicating overdistension) accompanied by a 46% increase in dorsal C RS(reg) (indicating recruitment). Global C RS altered minimally in this pressure window (Fig. E2c, ESM), emphasising the limitation of this parameter in detection of regional alterations in lung mechanics
P–V graphs derived from final-breath EELV(reg) values indicate both the shape of the entire P–V curve for each lung region and also the position on the curve at which regional tidal ventilation is occurring at each PEEP level (Fig. 5 and Fig. E4, ESM). Hysteresis as defined by the area within the P–V envelope was least prominent in the normal lung, increased significantly after lung lavage and decreased after surfactant treatment in all regions other than the left ventral region (P < 0.05, ANOVA with Duncan’s post hoc test). Hysteresis was significantly different between each lung region in all lung states, almost entirely due to disparity in the shape of the inflation limb. The shape of the deflation limb of the regional P–V relationship did not differ between lung states, with normalised EELV(reg) values at sequential PEEP levels being near identical (P > 0.05 for all comparisons, two-way ANOVA for repeated measures). Additionally, in both the lavaged and surfactant-treated lung, deflation-limb EELV(reg) values were consistent between lung regions (P > 0.05, all comparisons), re-emphasising the relative uniformity of regional P–V behaviour with PEEP decrements.
End-expiratory lung volume [EELV(reg)] from the final breath at each PEEP level during the vital capacity manoeuvre, normalised to VC (reg). Mean and SD for all animals, R lung data only (L lung data shown in Fig. E4, ESM). L column normal lung (NL), middle column lavaged lung (LL), R column surfactant-treated lung (ST). V ventral, M medial, D dorsal
Discussion
This study examined regional tidal ventilation, lung mechanics and P–V behaviour in the normal, lavaged and surfactant-treated neonatal lung during a stepwise vital capacity manoeuvre. We found that, after lung recruitment, with PEEP decrements a PEEP level could be identified at which there was relatively uniform distribution of regional tidal ventilation, associated with remarkable concordance of C RS(reg) values and topography of the deflation limb of the regional P–V curves.
There was good evidence that the vital capacity manoeuvre used in this study resulted in near-complete recruitment at the end of the PEEP increments. The parabolic C RS(reg) curves obtained with PEEP decrements, particularly in the lavaged and surfactant-treated lung, can only be expected with tidal ventilation occurring in an open lung, as has been predicted mathematically [24] and elegantly shown experimentally [25].
Our study assessed distribution of tidal ventilation by quantifying the coefficient of variation for regional V T values measured by EIT, and is the first study to our knowledge to examine ventilation distribution in this way. Given the evidence in support of volutrauma as a key factor in the pathogenesis of ventilator-induced lung injury [26], we consider that finding a point of relative uniformity of ventilation distribution may be critical for optimal ventilation, as it implies even distribution of tidal gas to open lung regions, with minimisation of alveolar stretch. Using a gas washout technique in ventilated children, Schibler and Henning [27] have noted the beneficial effects of PEEP in improving ventilation distribution, even without preceding recruitment.
Other investigators have detected imbalances in regional ventilation using EIT. Using a slower vital capacity manoeuvre in the lavaged pig lung, Meier et al. [5] showed a pattern very similar to ours in four antero-posterior lung regions, with tidal impedance change (“tidal variation”) rising to a peak at the lowest PEEP decrement of 10 cmH2O during deflation. The degree of uniformity of V T(reg), and regional values for C RS were not reported. Using a similar animal model, Odenstedt et al. [4] noted significant improvement in proportional regional ventilation after recruitment followed by ventilation at a single PEEP level of 10 cmH2O, with a return to pre-injury values.
Underlying the uniformity of distribution of V T(reg) at a decremental PEEP level was a concordance of regional compliance values. As with V T(reg), peak C RS(reg) values were very similar between lung regions during PEEP decrements (Table 1), highlighting the potential to achieve relative regional uniformity of mechanical behaviour, a logical aim of lung-protective ventilation [28]. Only one previous experimental study has reported direct measurements of regional C RS after full lung recruitment (i.e. deflation values), with the finding of a near concordance of C RS(reg) values within the mid-ventral and mid-dorsal of the four vertical regions [4]. A recent clinical study has highlighted the potential for measurements of C RS to guide PEEP titration. In two ventilated humans, measurement of regional collapse and hyperdistension using EIT were seen to correlate with similar measurements obtained by computed tomography during PEEP decrements after lung recruitment [21].
The regional P–V curves plotted from EELV(reg) values show variable degrees of hysteresis, clearly related to variation in the shape and position of the inflation limb [29–31]. The concordance of peak C RS(reg) values found during PEEP decrements is mirrored by the considerable overlap of the regional P–V curve deflation limbs in the lavaged and surfactant-treated lung.
Several limitations of our study are evident. We used a surfactant-depletion model of lung injury, which is known to be highly and uniformly recruitable [32]. Our experimental model was similar in size to a term newborn, with, compared with larger subjects, a smaller antero-posterior chest dimension and thus less superimposed pressure acting on the dependent regions [33]. Even so, significant gravity-related lung inhomogeneities were evident. For reasons of physiological instability at low PEEP, our vital capacity manoeuvre was completed relatively quickly, with a relatively short time at each PEEP level. This may have resulted in incomplete equilibration of tidal ventilation and compliance with each PEEP step. We also were constrained to a limited number of PEEP levels with a 5 cmH2O gap in between—clearly smaller steps are required for accurate PEEP titration at the bedside of the ventilated patient. Further experimental studies using smaller decrements and a longer time at each PEEP level will be important to delineate the role of regional tidal ventilation distribution and compliance measurements in finding optimal PEEP after full lung recruitment in the diseased lung.
The high-fidelity recordings of tidal ventilation, and the regional indices of lung function and lung volume that can be derived from them, show that EIT has much to recommend it as a bedside monitor of regional lung function and a possible guide to PEEP titration [22, 34, 35]. Preliminary data suggest that EIT estimates of V T(reg) correlate well with those measured by computed tomography [36, 37], although the V T(reg) values derived from rel. ΔZ measurement may not necessarily be comparable from one region to another. To overcome this, in the present study we referenced tidal regional rel. ΔZ to the maximal tidal impedance change noted in the same region [i.e. V T(reg) expressed as a proportion of maximum V T(reg)]. Similarly, C RS(reg) values were normalised to the maximum rel. ΔZ seen in the region during the entire manoeuvre, i.e. the VC(reg) [38]. These normalisation techniques, and the indices derived using them, will need further validation in experimental studies before such measures can be used for PEEP titration in the clinical setting.
Conclusions
After lung recruitment, a decremental PEEP level can be identified at which tidal ventilation is relatively uniformly distributed, with associated concordance in compliance between lung regions. Bedside monitoring of regional tidal ventilation and compliance using EIT may thus aid in PEEP selection.
References
Rimensberger PC (2002) Neonatal respiratory failure. Curr Opin Pediatr 14:315–321
Lachmann B (1992) Open up the lung and keep the lung open. Intensive Care Med 18:319–321
Rimensberger PC, Cox PN, Frndova H, Bryan AC (1999) The open lung during small tidal volume ventilation: concepts of recruitment and “optimal” positive end-expiratory pressure. Crit Care Med 27:1946–1952
Odenstedt H, Lindgren S, Olegard C, Erlandsson K, Lethvall S, Aneman A, Stenqvist O, Lundin S (2005) Slow moderate pressure recruitment maneuver minimizes negative circulatory and lung mechanic side effects: evaluation of recruitment maneuvers using electric impedance tomography. Intensive Care Med 31:1706–1714
Meier T, Luepschen H, Karsten J, Leibecke T, Grossherr M, Gehring H, Leonhardt S (2008) Assessment of regional lung recruitment and derecruitment during a PEEP trial based on electrical impedance tomography. Intensive Care Med 34:543–550
Halter JM, Steinberg JM, Schiller HJ, Dasilva M, Gatto LA, Landas S, Nieman GF (2003) Positive end-expiratory pressure after a recruitment maneuver prevents both alveolar collapse and recruitment/derecruitment. Am J Respir Crit Care Med 167:1620–1626
Takeuchi M, Goddon S, Dolhnikoff M, Shimaoka M, Hess D, Amato MB, Kacmarek RM (2002) Set positive end-expiratory pressure during protective ventilation affects lung injury. Anesthesiology 97:682–692
Gothberg S, Parker TA, Griebel J, Abman SH, Kinsella JP (2001) Lung volume recruitment in lambs during high-frequency oscillatory ventilation using respiratory inductive plethysmography. Pediatr Res 49:38–44
Amato MB, Barbas CS, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi-Filho G, Kairalla RA, Deheinzelin D, Munoz C, Oliveira R, Takagaki TY, Carvalho CR (1998) Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 338:347–354
Gattinoni L, Vagginelli F, Chiumello D, Taccone P, Carlesso E (2003) Physiologic rationale for ventilator setting in acute lung injury/acute respiratory distress syndrome patients. Crit Care Med 31:S300–S304
Borges JB, Okamoto VN, Matos GF, Caramez MP, Arantes PR, Barros F, Souza CE, Victorino JA, Kacmarek RM, Barbas CS, Carvalho CR, Amato MB (2006) Reversibility of lung collapse and hypoxemia in early acute respiratory distress syndrome. Am J Respir Crit Care Med 174:268–278
Puybasset L, Gusman P, Muller JC, Cluzel P, Coriat P, Rouby JJ (2000) Regional distribution of gas and tissue in acute respiratory distress syndrome. III. Consequences for the effects of positive end-expiratory pressure. CT Scan ARDS Study Group. Adult Respiratory Distress Syndrome. Intensive Care Med 26:1215–1227
Pelosi P, Goldner M, McKibben A, Adams A, Eccher G, Caironi P, Losappio S, Gattinoni L, Marini JJ (2001) Recruitment and derecruitment during acute respiratory failure: an experimental study. Am J Respir Crit Care Med 164:122–130
Terragni PP, Rosboch G, Tealdi A, Corno E, Menaldo E, Davini O, Gandini G, Herrmann P, Mascia L, Quintel M, Slutsky AS, Gattinoni L, Ranieri VM (2007) Tidal hyperinflation during low tidal volume ventilation in acute respiratory distress syndrome. Am J Respir Crit Care Med 175:160–166
Suter PM, Fairley B, Isenberg MD (1975) Optimum end-expiratory airway pressure in patients with acute pulmonary failure. N Engl J Med 292:284–289
Caironi P, Gattinoni L (2007) How to monitor lung recruitment in patients with acute lung injury. Curr Opin Crit Care 13:338–343
Hinz J, Gehoff A, Moerer O, Frerichs I, Hahn G, Hellige G, Quintel M (2007) Regional filling characteristics of the lungs in mechanically ventilated patients with acute lung injury. Eur J Anaesthesiol 24:414–424
Kunst PW, Vazquez dA, Bohm SH, Faes TJ, Lachmann B, Postmus PE, de Vries PM (2000) Monitoring of recruitment and derecruitment by electrical impedance tomography in a model of acute lung injury. Crit Care Med 28:3891–3895
Frerichs I, Dargaville PA, van Genderingen H, Morel DR, Rimensberger PC (2006) Lung volume recruitment after surfactant administration modifies spatial distribution of ventilation. Am J Respir Crit Care Med 174:772–779
Wolf GK, Grychtol B, Frerichs I, van Genderingen HR, Zurakowski D, Thompson JE, Arnold JH (2007) Regional lung volume changes in children with acute respiratory distress syndrome during a derecruitment maneuver. Crit Care Med 35:1972–1978
Costa EL, Borges JB, Melo A, Suarez-Sipmann F, Toufen C Jr, Bohm SH, Amato MB (2009) Bedside estimation of recruitable alveolar collapse and hyperdistension by electrical impedance tomography. Intensive Care Med 35:1132–1137
Frerichs I, Dargaville PA, Dudykevych T, Rimensberger PC (2003) Electrical impedance tomography: a method for monitoring regional lung aeration and tidal volume distribution? Intensive Care Med 29:2312–2316
Bhutani VK, Sivieri EM, Abbasi S, Shaffer TH (1988) Evaluation of neonatal pulmonary mechanics and energetics: a two factor least mean square analysis. Pediatr Pulmonol 4:150–158
Hickling KG (2001) Best compliance during a decremental, but not incremental, positive end-expiratory pressure trial is related to open-lung positive end-expiratory pressure: a mathematical model of acute respiratory distress syndrome lungs. Am J Respir Crit Care Med 163:69–78
Downie JM, Nam AJ, Simon BA (2004) Pressure-volume curve does not predict steady-state lung volume in canine lavage lung injury. Am J Respir Crit Care Med 169:957–962
Dreyfuss D, Saumon G (1998) Ventilator-induced lung injury: lessons from experimental studies. Am J Respir Crit Care Med 157:294–323
Schibler A, Henning R (2002) Positive end-expiratory pressure and ventilation inhomogeneity in mechanically ventilated children. Pediatr Crit Care Med 3:124–128
Rouby JJ, Ferrari F, Bouhemad B, Lu Q (2007) Positive end-expiratory pressure in acute respiratory distress syndrome: should the ‘open lung strategy’ be replaced by a ‘protective lung strategy’? Crit Care 11:180
van Genderingen HR, van Vught AJ, Jansen JR (2003) Estimation of regional lung volume changes by electrical impedance pressures tomography during a pressure–volume maneuver. Intensive Care Med 29:233–240
Kunst PW, Bohm SH, Vazquez dA, Amato MB, Lachmann B, Postmus PE, de Vries PM (2000) Regional pressure volume curves by electrical impedance tomography in a model of acute lung injury. Crit Care Med 28:178–183
Hinz J, Moerer O, Neumann P, Dudykevych T, Frerichs I, Hellige G, Quintel M (2006) Regional pulmonary pressure volume curves in mechanically ventilated patients with acute respiratory failure measured by electrical impedance tomography. Acta Anaesthesiol Scand 50:331–339
Kloot TE, Blanch L, Melynne YA, Weinert C, Adams AB, Marini JJ, Shapiro RS, Nahum A (2000) Recruitment maneuvers in three experimental models of acute lung injury. Effect on lung volume and gas exchange. Am J Respir Crit Care Med 161:1485–1494
Pelosi P, D’Andrea L, Vitale G, Pesenti A, Gattinoni L (1994) Vertical gradient of regional lung inflation in adult respiratory distress syndrome. Am J Respir Crit Care Med 149:8–13
Hedenstierna G (2004) Using electric impedance tomography to assess regional ventilation at the bedside. Am J Respir Crit Care Med 169:777–778
Wolf GK, Arnold JH (2005) Noninvasive assessment of lung volume: respiratory inductance plethysmography and electrical impedance tomography. Crit Care Med 33:S163–S169
Victorino JA, Borges JB, Okamoto VN, Matos GF, Tucci MR, Caramez MP, Tanaka H, Sipmann FS, Santos DC, Barbas CS, Carvalho CR, Amato MB (2004) Imbalances in regional lung ventilation: a validation study on electrical impedance tomography. Am J Respir Crit Care Med 169:791–800
Wrigge H, Zinserling J, Muders T, Varelmann D, Gunther U, von der GC, Magnusson A, Hedenstierna G, Putensen C (2008) Electrical impedance tomography compared with thoracic computed tomography during a slow inflation maneuver in experimental models of lung injury. Crit Care Med 36:903–909
Tingay DG, Copnell B, Grant CA, Dargaville PA, Dunster KR, Schibler A (2010) The effect of endotracheal suction on regional tidal ventilation and end-expiratory lung volume. Intensive Care Med 36:888–896
Acknowledgments
We thank Dr. Denis Morel, Anesthesiological Investigation Unit, University Hospital of Geneva for his contribution to these studies. This work was supported by a restricted research grant by Viasys Healthcare, and the surfactant (Curosurf) was generously provided by Nycomed.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dargaville, P.A., Rimensberger, P.C. & Frerichs, I. Regional tidal ventilation and compliance during a stepwise vital capacity manoeuvre. Intensive Care Med 36, 1953–1961 (2010). https://doi.org/10.1007/s00134-010-1995-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-1995-1