Abstract
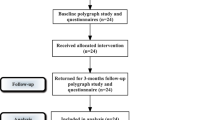
Laser-assisted uvulopalatoplasty (LAUP) reduces the need for general anesthesia, bleeding and the operation time compared with uvulopalatopharyngoplasty (UPPP), but the postoperative pain is more severe due to the thermal damage to tissues, and the procedure often causes serious scar contracture of the soft palate, with foreign body sensation also occurring occasionally. Radiofrequency-assisted uvulopalatoplasty (RAUP) uses the same surgical method as LAUP, but employs RF instead of laser. RF surgery induces temperatures of 70–85°C, and causes less damage to the surrounding tissues. Thus, on the assumption that it may reduce problems in LAUP, we applied LAUP and RAUP at random to patients with primary snoring, and compared the results of the two types of operation and both their advantages and disadvantages. Forty-four patients with primary snoring but without apnea were prospectively evaluated with a follow-up period of 6 months: 20 patients received LAUP and 24 patients received RAUP. Postoperative changes in the subjective degree of snoring, the Epworth sleepiness scale score, and the operation time, postoperative pain, episodes of delayed bleeding, globus sensation and scar contracture were compared between the two surgical methods. Snoring symptoms, ESS scores and episodes of delayed bleeding did not differ significantly between the two groups. The operation time was shorter in the LAUP group, and the postoperative pain and postoperative complications (globus sensation and scar contracture) were less in the RAUP group. RAUP results in significantly lower postoperative pain, complications and other problems experienced in LAUP, while maintaining the advantages of LAUP.






Similar content being viewed by others
References
Hoffstein V, Mateika JH, Mateika S (1991) Snoring and sleep architecture. Am Rev Respir Dis 143:92–96
Fujita S, Conway WA, Zorick FJ, Roth T (1981) Surgical correction of anatomic abnormalities in obstructive sleep apnea syndrome: Uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg 89:923–934
Kamami YV (1990) Laser CO2 for snoring: preliminary results. Acta Otorhinolaryngol Belg 44:451–456
Powell NB, Riley RW, Troell RJ, Li K, Blumen MB, Guilleminault C (1998) Radiofrequency volumetric tissue reduction of the palate in subject with sleep-disordered breathing. Chest 113:1163–1174
Wedman J, Miljeteig H (2002) Treatment of simple snoring using radio waves for ablation of uvula and soft palate: a day surgery procedure. Laryngocope 112:1256–1259
Hong SK, Shin HJ, Chung SM, Byun SW, Shin YR, Kim JK (2002) Conventional, laser-assisted and coblation-assisted uvulopalatopharyngoplasty/uvulopalatoplasty: their advantages and disadvantages. Korean J Otolaryngol 45:395–365
Lugaresi E, Cirignotta F, Coccagna G, Baruzzi A (1982) Snoring and the obstructive apnea syndrome. Electroencephalogr Clin a pilot study(Suppl) 35:421–430
Koskenvuo M, Kaprio J, Partinen M, Langinvainio H, Sarna S, Heikkila K (1985) Snoring as a risk factor for hypertension and angina pectoris. Lancet 1(8434):893–896
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235
Osman EZ, Osborne J, Hill PD, Lee BWV (1999) The Epworth sleepiness scale: can it be used for sleep apnoea screening among snorers? Clin Otolaryngol Allied Sci 24(3):239–241
Miletin MS, Hanly PJ (2003) Measurement properties of the Epworth sleepiness scale. Sleep Med 4(3):195–199
Maurer JT, Hein G, Verse T, Hormann K, Stuck BA (2005) Long-term results of palatal implants for primary snoring. Otolaryngol Head Neck Surg 133(4):573–578
Cincik H, Cekin E, Cetin B, Gungor A, Poyrazoglu E (2006) Comparison of uvulopalatopharyngoplasty, laser-assisted uvulopalatoplasty and cautery-assisted uvulopalatoplasty in the treatment of primary snoring. ORL J Otorhinolaryngol Relat Spec 68(3):149–155
Croft CB, Golding-Wood DG (1990) Uses and complications of uvulopalatopharyngoplasty. J Laryngol Otol 104:871–875
Finkelstein Y, Shapiro-Feinberg M, Stein G, Ophir D (1997) Uvulopalatopharyngoplasty vs laser-assisted uvulopalatoplasty. Anatomical considerations. Arch Otolaryngol Head Neck Surg 123(3):265–276
Ryan C, Love L (2000) Unpredictable results of laser-assisted uvulopalatoplasty in the treatment of obstructive sleep apnea. Thorax 55:399–404
Kim JH, Lee YS, Park HW, Nam SY, Kim YJ, Lee BJ (2000) Laser-assisted uvuloplalatoplasty and laser uvulopalatopharyngoplasty for snoring and obstructive sleep apnea: long-term postoperative patients’ satisfaction. Korean J Otolaryngol 43:173–178
Kamami YV (1994) Outpatient treatment of sleep apnea syndrome with CO2 laser: laser-assisted UPPP. J Otolaryngol 23:395–398
Walker RP, Grigg-Damberger MM, Goplasami C, Totten MC (1995) Laser-assisted uvulopalatoplasty for snoring and obstructive sleep apnea: Results in 170 patients. Laryngoscope 105:938–943
Littner M, Kushida CA, Hartse K, Anderson WM, Davila D, Johnson SF et al (2001) Practice parameters for the use of laser-assisted uvulopalatoplasty: an update for 2000. Sleep 24(5):603–619
Powell NB, Riley RW, Troell RJ, Blumen MB, Guilleminault C (1997) Radiofrequency volumetric tissue reduction of the tongue: a porcine pilot study for the treatment of obstructive sleep apnea syndrome. Chest 111:1348–1355
Kim JH (2002) Radiofrequency surgery. Korean J Otolaryngol 45:531–537
Hong SK, Yoon SO, Park SK, Son JY, Kim EA, Cho YH et al (2002) Laser-assisted versus coblation-assisted partial turbinoplasty: comparison by their postoperative outcome. Korean J Otolaryngol 45:589–593
Nelson LM (2000) Radiofrequency treatment for obstructive tonsillar hypertrophy. Arch Otolaryngol Head Neck Surg 126:736–740
Emery BE, Flexon PB (2000) Radiofrequency volumetric tissue reduction of the soft palate: a new treatment for snoring. Laryngoscope 110:1092–1098
Powell NB, Riley RW, Guilleminault C (1999) Radiofrequency tongue base reduction in sleep-disordered breathing: a pilot study. Otolaryngol Head Neck Surg 120:656–664
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lim, D.J., Kang, S.H., Kim, B.H. et al. Treatment of primary snoring using radiofrequency-assisted uvulopalatoplasty. Eur Arch Otorhinolaryngol 264, 761–767 (2007). https://doi.org/10.1007/s00405-007-0252-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-007-0252-x