Abstract
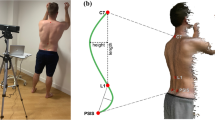
There is an increasing awareness of the risks and dangers of exposure to radiation associated with repeated radiographic assessment of spinal curvature and spinal movements. As such, attempts are continuously being made to develop skin-surface devices for use in examining the progression and response to treatment of various spinal disorders. However, the reliability and validity of measurements recorded with such devices must be established before they can be recommended for use in the research or clinical environment. The aim of this study was to examine the reliability of measurements using a newly developed skin-surface device, the Spinal Mouse. Twenty healthy volunteers (mean age 41±12 years, nine males, 11 females) took part. On 2 separate days, spinal curvature was measured with the Spinal Mouse during standing, full flexion, and full extension (each three times by each of two examiners). Paired t-tests, intraclass correlation coefficients (ICC), and standard errors of measurement (SEM) with 95% confidence intervals were used to characterise between-day and interexaminer reliability for: standing sacral angle, lumbar lordosis, thoracic kyphosis, and ranges of motion (flexion, extension) of the thoracic spine, lumbar spine, hips, and trunk. The between-day reliability for segmental ranges of flexion was also determined for each motion segment from T1-2 to L5-S1. The majority of parameters measured for the ‘global regions’ (thoracic, lumbar, or hips) showed good between-day reliability. Depending on the parameter of interest, between-day ICCs ranged from 0.67 to 0.92 for examiner 1 (average 0.82) and 0.57 to 0.95 for examiner 2 (average 0.83); for 70% of the parameters measured, the ICCs were greater than 0.8 and generally highest for the lumbar spine and whole trunk measures. For lumbar spine range of flexion, the SEM was approximately 3°. The ICCs were also good for the interexaminer comparisons, ranging from 0.62 to 0.93 on day 1 (average 0.81) and 0.70 to 0.94 on day 2 (average 0.86), although small systematic differences were sometimes observed in their mean values. The latter were still evident even if both examiners used the same skin markings. For segmental ranges of flexion, the ICCs varied between vertebral levels but overall were lower than for the global measures (average for all levels in all analyses, ICC 0.6). For each examiner, the average between-day SEM over all vertebral levels was approximately 2°. For ‘global’ regions of the spine, the Spinal Mouse delivered consistently reliable values for standing curvatures and ranges of motion which compared well with those reported in the literature. This suggests that the device can be reliably implemented for in vivo studies of the sagittal profile and range of motion of the spine. As might be expected for the smaller angles being measured, the segmental ranges of flexion showed lower reliability. Their usefulness with regard to the interpretation of individual results and the detection of ‘real change’ on an individual basis thus remains questionable. Nonetheless, the group mean values showed few between-day differences, suggesting that the device may still be of use in providing clinically interesting data on segmental motion when examining groups of individuals with a given spinal pathology or undergoing some type of intervention.




Similar content being viewed by others
References
Adams MA, Dolan P (1991) A technique for quantifying the bending moment acting on the lumbar spine in vivo. J Biomech 24:117–126
American Medical Association (2000) The spine. In: Cocchiarella L, Andersson GBJ (eds) Guides to the evaluation of permanent impairment. Fifth edn. AMA, Chicago
Beaton DE (2000) Understanding the relevance of measured change through studies of responsiveness. Spine 25:3192–3199
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet, Feb 8:307–310
Burton AK (1986) Regional lumbar sagittal mobility; measurement by flexicurves. Clin Biomech 1:20–26
Chinn S (1991). Repeatability and method comparison. Thorax 46:454–456
Currier DP (1990) Elements of research in physical therapy. Third edn. Williams and Wilkins, Baltimore
Dolan P, Adams MA (1993) Influence of lumbar and hip mobility on the bending stresses acting on the lumbar spine. Clin Biomech 8:185–192
Dolan P, Earley M, Adams MA (1994) Bending and compressive stresses acting on the lumbar spine during lifting activities. J Biomech 27:1237–1248
Dolan P, Greenfield K, Nelson RJ, Nelson IW (2000) Can exercise therapy improve the outcome of microdiscectomy? Spine 25:1523–1532
Dopf CA, Mandel SS, Geiger DF, Mayer PJ (1994) Analysis of spine motion variability using a computerized goniometer compared to physical examination. A prospective clinical study. Spine 19:586–595
Dvorak J, Panjabi MM, Chang DG, Theiler R, Grob D (1991) Functional radiographic diagnosis of the lumbar spine. Flexion-extension and lateral bending. Spine 16:562–571
Dvorak J, Vajda EG, Grob D, Panjabi MM (1995) Normal motion of the lumbar spine as related to age and gender. Eur Spine J 4:18–23
Essendrop M, Maul I, Laubli T, Riihimaki H, Schibye B (2002) Measures of low back function: a review of reproducibility studies. Clin Biomech 17:235–249
Frobin W, Brinckmann P, Leivseth G, Biggemann M, Reikeras O (1996) Precision measurement of segmental motion from flexion-extension radiographs of the lumbar spine. Clin Biomech 11:457–465
Gelb DE, Lenke LG, Bridwell KH, Blanke K, McEnery KW (1995) An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine 20:1351–1358
Gill K, Krag MH, Johnson GB, Haugh LD, Pope MH. (1988) Repeatability of four clinical methods for assessment of lumbar spinal motion. Spine 13:50–53
Harrison DE, Cailliet R, Harrison DD, Janik TJ (2002) How do anterior/posterior translations of the thoracic cage affect the sagittal lumbar spine, pelvic tilt, and thoracic kyphosis? Eur Spine J 11:287–293
Harrison DE, Harrison DD, Cailiet R, Janik TJ, Holland B (2001) Radiographic analysis of lumbar lordosis: centroid, Cobb, Trall, and Harrison posterior tangent methods. Spine 26:235–242
Hayes MA, Howard TC, Gruel CR, Kopta JA (1989) Roentgenographic evaluation of lumbar spine flexion-extension in asymptomatic individuals. Spine 14:327–331
Hopkins WG (2000). Measures of reliability in sports medicine and science. Sports Med 30:1–15
Jackson RP, McManus AC (1994) Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. Spine 19:1611–1618
Kanayama M, Abumi K, Kaneda K, Tadano S, Ukai T (1996) Phase lag of the intersegmental motion in flexion-extension of the lumbar and lumbosacral spine. An in vivo study. Spine 21:1416–1422
Louis R (1983) Chirurgie du rachis. Springer, Berlin Heidelberg New York, pp 64–74
Mannion AF, Dolan P, Dumas GA, Stevenson J, Cooper RG, Wood K, Adams MA (unpublished data) pooled results from 3 previously published studies, in which part of the investigation also required measurements of spinal mobility with the Fastrak system.
Mannion AF, Dvorak J, Müntener M, Grob D (2003). Prospective study of changes in self-rated disability and range of motion of the lumbar spine in patients with disc herniation undergoing decompression surgery. Presented at the Annual Meeting of the International Society for the Study of the Lumbar Spine, Vancouver
Mannion AF, Troke M (1999) A comparison of two motion analysis devices used in the measurement of lumbar spinal mobility. Clin Biomech 14:612–619
Mayer RS, Chen IH, Lavender SA, Trafimow JH, Andersson GBJ (1995) Variance in the measurement of sagittal lumbar spine range of motion among examiners, subjects, and instruments. Spine 20:1489–1493
McGregor AH, McCarthy ID, Hughes SP (1995) Motion characteristics of the lumbar spine in the normal population. Spine 20:2421–2428
Miyasaka K, Ohmori K, Suzuki K (2000) Radiographic analysis of lumbar motion in relation to lumbosacral stability. Spine 25:732–737
Morin Doody M, Lonstein JE, Stovall M, Hacker DG, Luckyanov N, Land CE (2000) Breast cancer mortality after diagnostic radiography: findings from the U.S. Scoliosis Cohort Study. Spine 25:2052–2063
Ng K-F, Kippers V, Richardson CA, Parnianpour M (2001) Range of motion and lordosis of the lumbar spine. Reliability of measurement and normative values. Spine 26:53–60
Panjabi M, Chang D, Dvorak J (1992) An analysis of errors in kinematic parameters associated with in vivo functional radiographs. Spine 17:200–205
Pearcy M, Portek I, Shephard J (1984). Three dimensional X-ray analysis of normal movement in the lumbar spine. Spine 9:294–297
Pearcy MJ, Hindle RJ (1989) New method for the non-invasive three-dimensional measurement of human back movement. Clinical Biomechanics 4:73–79
Perneger TV (1998) What’s wrong with Bonferroni adjustments? BMJ 316:1236–1238
Peterson CM, Johnson RD, Schuit D, Hayes KW (1994) Intraobserver and interobserver reliability of asymptomatic subjects thoracolumbar range of motion using the OSI CA6000 spine motion analyser. J Orthop Sports Phys Ther 20:207–212
Plamondon A, Gagnon M, Maurais G (1988) Application of a stereoradiographic method for the study of intervertebral motion. Spine 13:1027–1032
Polly DW Jr, Kilkelly FX, McHale KA, Asplund LM, Mulligan M, Chang AS (1996) Measurement of lumbar lordosis. Evaluation of intraobserver, interobserver, and technique variability. Spine 21:1530–1535
Salisbury PJ, Porter RW (1986) Measurement of lumbar sagittal mobility. A comparison of methods. Spine 12:190–193
Schuit D, Petersen C, Johnson R, Levine P, Knecht H, Goldberg D (1997) Validity and reliability of measures obtained from the OSI CA-6000 Spine Motion Analyzer for lumbar spinal motion. Manual Therapy 2:206–215
Seichert N, Baumann M, Senn E, Zuckriegl H (1994) Die Rückenmaus—ein analog-digitales Messgerät zur Erfassung der sagittalen Rückenkontur. Phys Rehab Kur Med 4:34–43
Stokes IAF, Bevins TM, Lunn RA (1987) Back surface curvature and measurement of lumbar spinal motion. Spine 12:355–361
Tallroth K, Ylikoski M, Landtman M, Santavirta S (1994) Reliability of radiographical measurements of spondylolisthesis and extension-flexion radiographs of the lumbar spine. Eur J Radiol 18:227–231
Tillotson KM, Burton AK (1991) Noninvasive measurement of lumbar sagittal mobility. An assessment of the flexicurve technique. Spine 16:29–33
Troke M, Moore AP, Maillardet FJ, Hough A, Cheek E (2001) A new, comprehensive normative database of lumbar spine ranges of motion. Clin Rehabil 15:371–379
Troyanovich SJ, Cailliet R, Janik TJ, Harrison DD, Harrison DE (1997) Radiographic mensuration characteristics of the sagittal lumbar spine from a normal population with a method to synthesize prior studies of lordosis. J Spinal Disord 10:380–386
Van Herp G, Rowe P, Salter P, Paul JP (2000) Three-dimensional lumbar spinal kinematics: a study of range of movement in 100 healthy subjects aged 20 to 60+ years. Rheumatology (Oxford) 39:1337–1340
Vaz G, Roussouly P, Berthonnaud E, Dimnet J (2002) Sagittal morphology and equilibrium of pelvis and spine. Spine 11:80–87
Vedantam R, Lenke L, Keeney J, Bridwell K (1998) Comparison of standing sagittal spinal alignment in asymptomatic adolescents and adults. Spine 23:211–215
Vogt L, Pfeifer K, Portscher M, Banzer W (2001) Influences of nonspecific low back pain on three-dimensional lumbar spine kinematics in locomotion. Spine 26:1910–1919
Voutsinas SA, MacEwen GD (1986) Sagittal profiles of the spine. Clin Orthop 210:235–242
Zuberbier OA, Kozlowski AJ, Hunt DG, Berkowitz J, Schultz IZ, Crook JM, Milner RA (2001) Analysis of the convergent and discriminant validity of published lumbar flexion, extension, and lateral flexion scores. Spine 26:472–478
Acknowledgements
This study was funded by the Swiss National Science Foundation (grant 32-57123.99) and the Schulthess Klinik Research Funds.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mannion, A.F., Knecht, K., Balaban, G. et al. A new skin-surface device for measuring the curvature and global and segmental ranges of motion of the spine: reliability of measurements and comparison with data reviewed from the literature. Eur Spine J 13, 122–136 (2004). https://doi.org/10.1007/s00586-003-0618-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-003-0618-8