Abstract
Tracheal intubation disrupts physiological homeostasis of secretion production and clearance, resulting in secretion accumulation within endotracheal tubes (ETTs). Novel in vitro and in vivo models were developed to specifically recapitulate the clinical manifestations of ETT occlusion. The novel Sharklet™ micropatterned ETT was evaluated, using these models, for the ability to reduce the accumulation of both bacterial biofilm and airway mucus compared to a standard care ETT. Novel ETTs with micropattern on the inner and outer surfaces were placed adjacent to standard care ETTs in in vitro biofilm and airway patency (AP) models. The primary outcome for the biofilm model was to compare commercially-available ETTs (standard care and silver-coated) to micropatterned for quantity of biofilm accumulation. The AP model’s primary outcome was to evaluate accumulation of artificial airway mucus. A 24-h ovine mechanical ventilation model evaluated the primary outcome of relative quantity of airway secretion accumulation in the ETTs tested. The secondary outcome was measuring the effect of secretion accumulation in the ETTs on airway resistance. Micropatterned ETTs significantly reduced biofilm by 71% (p = 0.016) compared to smooth ETTs. Moreover, micropatterned ETTs reduced lumen occlusion, in the AP model, as measured by cross-sectional area, in distal (85%, p = 0.005), middle (84%, p = 0.001) and proximal (81%, p = 0.002) sections compared to standard care ETTs. Micropatterned ETTs reduced the volume of secretion accumulation in a sheep model of occlusion by 61% (p < 0.001) after 24 h of mechanical ventilation. Importantly, micropatterned ETTs reduced the rise in ventilation peak inspiratory pressures over time by as much as 49% (p = 0.005) compared to standard care ETTs. Micropatterned ETTs, demonstrated here to reduce bacterial contamination and mucus occlusion, will have the capacity to limit complications occurring during mechanical ventilation and ultimately improve patient care.
Similar content being viewed by others
Introduction
Mechanical ventilation is often essential for critically ill patients and for patients undergoing surgical procedures under general anesthesia. However, mechanical ventilation has associated risks7,43 including occlusion of endotracheal tubes (ETTs) with airway secretions and bacterial biofilm-related infections which can result in ventilator-associated conditions, such as ventilator-associated pneumonia (VAP). VAP affects as many as 28% of mechanically ventilated intensive care patents,9 with a mortality rate between 20 and 30%.45 Secretion buildup within tube lumens occurs universally for all intubated patients in varying degrees, beginning within hours of intubation,5 and can potentiate biofilm-related infection.30 While both complications result in increased patient morbidity and healthcare costs,12,30 an initial step to resolving the related adverse events is to reduce secretion accumulation on the lumen surface. This reduction eliminates the hospitable environment for biofilm buildup, while also improving efficiency of gas exchange and avoiding the need for aggressive ventilation settings. Reduction of secretion accumulation is thus important to reducing complications associated with mechanical ventilation.
Although the impact of partial ETT occlusion on duration of ventilation and weaning success may be underestimated due to a lack of specialized monitoring strategies,40,47 it has been demonstrated that clinically significant tube occlusion occurs as early as 24 h following intubation.5 Airway secretions during tracheal intubation accumulate in the lumen of the ETT, which may eventually lead to complete occlusion.5,18,31,49,51 Luminal narrowing due to secretion buildup correlates with increased airflow resistance that leads to increased work of breathing for the patient.32,51 Physicians commonly evaluate suitability for extubation by conducting spontaneous breathing trials where the patient must breathe through the ETT. Reduction in ETT internal diameter caused by secretion accumulation results in significant increases in diaphragmatic effort, decreases in tidal volume and disruption in breathing patterns during weaning procedures.16,43,48 Consequently, patients often fatigue prematurely and fail to wean due to ETT occlusion alone.19,20,37,51 Timely ETT removal, i.e., weaning of patients from respiratory support, will allow for shorter hospital stays and reduced healthcare costs.12,30
Complete occlusion of the ETT can occur abruptly after secretion accumulation resulting in a life-threatening lack of airflow and requiring emergency intervention.18,49 Frequent ETT suction cleaning is standard of care for patients on mechanical ventilation with the goal to clear secretions from the ETT.6 However, studies have shown that suctioning alone is not sufficient to preserve airway patency5,10,31 and may increase the risk for serious complications such as pneumothorax, hypoxia and hemodynamic instability.17,34,42 Thus, it is crucial to preserve ETT patency by specifically developing devices to reduce or remove secretion accumulation. There are currently no solutions approved for use in clinical practice, however several suctioning devices designed to remove mucus buildup are being trialed.3,29
To complement this strategy and eliminate reliance on suction cleaning, we have developed and manufactured a Sharklet™-micropatterned ETT. Sharklet –a micropattern bio-inspired by the textured surface of sharkskin- consists of 2-μm-wide ribs of various lengths that are combined to form a diamond-shaped micropattern that repeats to create a texture that is similar to the skin of a shark.2 This micropattern has been shown to increase surface energy and consequently reduce the accumulation of biological substances on a variety of substrates.8,13,24 – 28,39 To evaluate the efficacy of Sharklet micropatterned ETTs to limit lumen occlusion and bacterial biofilm, we developed in vitro biofilm and airway patency (AP) models and an in vivo model of mechanical ventilation in sheep.
Methods
Endotracheal Tube Test Articles
Sharklet™ micropatterned ETTs were manufactured via injection molding Pellethane 2363-90AE thermoplastic polyurethane (TPU; Lubrizol) by 10 × Microstructures (Wheeling, IL) and assembled by Bates Industries (South Glens Falls, NY). Fully assembled first generation Sharklet™ ETTs (Fig. 1) were tested and compared to standard care control polyvinyl chloride (PVC) ETTs made by Medline (Medline Industries, Inc., Mundelein, IL) for AP testing or Mallinckrodt™ ETT (Medtronic, Minneapolis, MN) for preclinical testing. Additionally, silver-coated PVC (Agento™, Bard, Covington, GA) ETTs were compared to Sharklet micropatterned ETTs for biofilm control given the proposed antimicrobial attributes of silver. All ETTs were size-matched for initial internal diameter (ID = 7.0 mm).
Micropattern incorporated on an endotracheal tube. These first-generation devices were injection-molded to imprint the micropattern on the ETT lumen and outer surface. Confocal microscopy demonstrates that the micropattern is oriented such that the long axis of individual features aligns with the longitudinal direction of the tube, i.e., along the direction of secretion flow. Scale bar, 20 μm.
In Vitro Drip-flow Biofilm Model
Drip Flow Biofilm Model and Bacterial Strains Tested
Biofilm-proficient bacterial strains Pseudomonas aeruginosa (PA14 bifA null) and methicillin-resistant Staphylococcus aureus (MRSA: ATCC 700698)21 were struck from freezer stocks onto fresh tryptic soy broth (TSB) agar into individual colonies that were grown at 37 °C overnight and stored at 4 °C for inoculation of overnight cultures. Overnight cultures were initiated by inoculating 5 ml of fresh TSB in a test tube with a single bacterial colony and allowing it to grow with shaking at approximately 200 RPM overnight. Drip flow reactors were set up according to the ASTM E2647-13 with slight modifications.14 Briefly, the reactor was positioned at 25° rather than 10°. P. aeruginosa was inoculated into 200 ml of TSB using a 1:100 dilution from the overnight culture and the inoculated media was continuously recirculated and dripped through the reactor onto the test surfaces. A minimum of three experiments were completed for each strain and condition. Micropatterned, standard care, and silver-coated ETTs were processed into 80 mm long segments and sliced in half longitudinally to expose the luminal surface for biofilm challenge.
Quantification
After the biofilm culture period was complete, the flow was terminated and the reactors were opened to move each test surface to individual Petri dishes. For the quantification of biofilm, the samples were placed in Dey-Engley buffer, vortexed for 10 min, sonicated for 10 min, then placed in a 37 °C water bath for 30 min to allow for biofilm separation. The samples were then vortexed for 10 min and sonicated for 10 min. The resulting Dey-Engley buffer was serial dilution-plated onto tryptic soy agar plates and incubated overnight at 37 °C. Colony forming units growing on tryptic soy agar plates were enumerated and recorded along with the associated dilution range.
In Vitro Airway Patency Model
The airway patency (AP) model was developed to facilitate in vitro assessment of secretion accumulation on ETT luminal surfaces (Fig. 2). A fixture was designed as part of the model to hold and test up to four ETTs simultaneously. Adjustable, hinged platforms were incorporated to provide the ability to mimic anatomical tracheal bending and head-of-bed position. The head-of-bed angle was set to 30° for all experiments to recapitulate current clinical practices.1,50 Tubes were connected through an air splitter and a breathing-circuit (CareFusion, Chicago, IL) to a ventilator (Servo SV900C, Siemens-Elema AB, Solna, Sweden) and placed inside a reservoir that was filled with artificial mucus. A test lung (Adult Test Lung 190, MAQUET Critical Care AB, Solna, Sweden) connected to the reservoir returned air to the ventilator simulating expiration. The apparatus was warmed to approximately 37 °C for the duration of the study. To account for the four-channel design of the test fixture and the large amount of liquid artificial mucus placed in the reservoir, the ventilator was set to a pressure-controlled mode with settings of respiratory rate 10 breaths/min, peak inspiratory pressure 10 cmH20, positive end expiratory pressure of 4 cmH20 and inspiratory time of 0.6 s. The ventilator settings differ slightly from those used in an intensive care unit because these settings were adjusted to generate consistent aspiration of artificial mucus simultaneously into the four ETTs. Through the model development process similarity in consistent aspiration was assessed visually by verifying that artificial mucus was aspirated into each tube to a specific height marked on the test fixture. Using mechanical ventilation, simulated airway secretions were pulled into ETTs to recapitulate the interaction of respiratory secretions with the luminal surface of the ETT.
Airway patency model using artificial mucus. The adjustable supports allowed investigators to bend ETTs to match tracheal anatomy and head-of-bed position. Four ETTs were simultaneously connected to an air splitter and a breathing circuit that ultimately attached to a ventilator. The distal ends of ETTs were placed inside the breathing reservoir filled with artificial mucus. A test lung connected to the reservoir returned air to the ventilator simulating expiration. A liquid level sensor, peristaltic pump, and mucus supply reservoir provided a constant supply of artificial mucus to counteract evaporation over long experimental durations. As breathing proceeded through the AP model, simulated airway secretions were pulled into tubes to mimic the interaction of respiratory secretions with airway devices.
To evaluate the potential for Sharklet micropatterned ETTs to reduce luminal occlusion, micropatterned ETTs were tested against standard care ETT controls in the AP model. Four tubes, two micropatterned and two standard care controls, were tested in each of three experiments. Endotracheal tubes were exposed to artificial mucus for approximately 48 h at 37 °C. Artificial mucus was composed of 4% weight/volume mucin from porcine stomach, Type II (Sigma-Aldrich, St. Louis, MO), 2% weight/volume lecithin (Alfa Aesar, War Hill, MA), 40 mM potassium hydroxide, dibasic, 20 mM potassium hydroxide, monobasic, 50 mM ammonium sulfate and 1 mM magnesium sulfate (Sigma-Aldrich, St. Louis, MO), 50 U/mL each penicillin/streptomycin, 1 μg/mL Fungizone® Antimycotic (Life Technologies, Carlsbad, CA).22,33,38,41 Following mucus exposure, ETTs were cut into proximal, middle and distal sections for both weight measurements and cross-sectional imaging. The tube sections designated for weight measurements were subsequently weighed, cleaned, dried and re-weighed. The weight of accumulated mucus was calculated by subtracting the clean tube weight from the occluded tube weight.
Two 2-mm wide samples from each of the proximal, middle, and distal sections were imaged using brightfield microscopy (BX63, Olympus, Center Valley, PA) with the 2× objective. The digital pixels were categorized as belonging to luminal or mucus area, and ETT lumens were isolated using vector drawing software (Illustrator CC, Adobe Systems Incorporated, San Jose, CA). The images were further processed using ImageJ software (ImageJ, U.S. National Institutes of Health, Bethesda, MD)—images were converted to 8-bit binary and the “analyze particles” function was used to measure the luminal area. The calculated intraluminal cross-sectional area of occlusion was compared to the total cross-sectional luminal area for each sample to determine overall reductions in cross-sectional area.
In Vivo Airway Patency Model
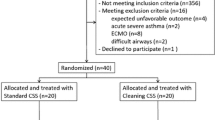
In accordance with Wake Forest Baptist Health Institutional Animal Use and Care Committee, five female Dorset sheep greater than 24 kg were fasted 48 h from hay and 16 h from grain prior to receiving general anesthesia. Six sheep were prepared; three in the treatment group and three in the control group. One animal from the control group was excluded due to an adverse reaction to anesthesia and mechanical ventilation. On the day of the procedure, sheep were given intravenous anesthetic and analgesic medications: 0.02 mg/kg glycopyrrolate and 0.01 mg/kg buprenorphine followed by 0.01 mg/kg dexmedetomidine and 10 mg/kg ketamine. Sevoflurane was delivered by facemask to supplement the intravenous anesthetic medications. Once unconscious, the animal was intubated with either a micropatterned ETT or a standard care ETT and maintained under general anesthesia with 0.5–8.0% sevoflurane or 0.5–5% isoflurane gas delivered in oxygen. Ophthalmic ointment was placed in each eye and a rumen tube was placed to control regurgitation and gaseous accumulation in the rumen. The sheep was placed in a horizontal supine position and standard monitoring equipment was attached for the duration of the study period. Hourly bronchoscopies were done to observe buildup of respiratory secretions and ensure the ETT was not completely occluded. Eight hours into the study, the sheep was tilted with the head raised vertically to 12° (±1.5°) by adjusting the angle of the surgical table. The animal was mechanically ventilated using a volume-regulated veterinary anesthesia ventilator (Hallowell EMC Model 2000, Hallowell Engineering & Manufacturing Corp., Pittsfield, MA) attached to a heated humidification system (Fisher-Paykel MR730 kit, Fisher-Paykel, Auckland, New Zealand) for 24 h. Tidal volume was maintained between 15 and 25 mL/kg. Animal vitals (tidal volume, blood oxygen, blood CO2, blood pressure, heart rate, mean arterial pressure, and respiratory rate) were continuously monitored. Peak inspiratory pressures were regularly monitored (approximately every 5 min) and recorded from the ventilator during inspiration cycles. Fluid management and medications were standard care for all animals throughout the study.
After the 24 h study period, the sheep were euthanized with intravenous administration of the barbiturate Euthasol using at least 100 mg/kg in accordance with American Veterinary Medical Association (AVMA) guidelines. Following euthanasia the ETT was removed, the exterior was wiped clean, the ETT was weighed, and a computerized axial tomography (CT) image of the ETT was then obtained using an Aquilion 32 CT research scanner (Toshiba, Tustin, CA).
Statistical Analysis
Statistical significance was assessed at a 5% significance level using 1-sided p values derived from the reduction of control mean to micropatterned surface, thereby justifying the evaluation of significant reduction. All ANOVA models were performed using MiniTab 17 statistical software (MiniTab, Inc. Fort Worth, TX).
In Vitro Drip-Flow Biofilm Model
The log reduction (LR) was calculated by subtracting the average biofilm log density for the test surfaces from the average log density for the smooth control surfaces. Normality of the LRs was assessed by residual and normal probability plots. For ease of interpretation, the mean LR was converted to a median percent reduction with the equation: percent reduction = 1–10(−Log Reduction).
In Vitro Airway Patency Model
Accumulated mucus weight and occluded cross-sectional area were measured in each experiment. The standard care ETT and micropatterned ETT samples were compared with respect to each measure by an ANOVA with a random effect for experiment and a fixed effect for device type.
In Vivo Airway Patency Model
Accumulated mucus weight and volume were measured for the entire length of the devices. Area restriction at the narrowest point was also measured for each device. Statistical significance for each of these three measures was assessed using an ANOVA to the individual responses for each animal with a random effect for Date (because two animals, one from each group, were processed on each of 3 days) and a fixed effect for treatment group.
For each of the two time periods (the first 8 h while the animals were horizontal, and then the last 16 h when the animals were inclined), statistical significance of peak inspiratory pressure’s (PIP) increase over time was assessed by a linear mixed effect model fit to the PIP response. An individual animal identifier was included as a random effect, treatment group was a fixed effect, and the 2-way interaction of surface and tidal volume with treatment group were covariates. This model was fit using the statistical software R,44 package nlme.35
Results
In Vitro Drip-Flow Biofilm Model
Micropatterned ETTs reduced P. aeruginosa biofilm accumulation by 71% (p = 0.016) compared to the commercially-available standard care ETT (Fig. S1). The commercially-available silver-coated ETT reduced biofilm by 65% (p = 0.064) (Fig. S1).
In Vitro Airway Patency Model
The comparison of in vitro mucus weight in micropatterned ETTs vs. standard care ETTs yielded significant reductions in each measured section. Distal sections exhibited a reduction of 86% (p = 0.001), middle sections a reduction of 72% (p = 0.006), and proximal sections a reduction of 69% (p = 0.005) of Sharklet™ ETTs compared to standard care ETTs (Fig. 3).
The micropattern reduces artificial mucus accumulation. Artificial mucus weight (g) in the ETTs grouped by section along the tube length. Micropatterned ETTs significantly reduced weight of accumulated material in every section compared to standard care ETTs. Error bars indicate standard error of the mean of three individual experiments.
Cross-sectional imaging also revealed a statistically significant reduction in lumen occlusion for micropatterned ETT lumens compared to standard care ETTs (Fig. 4a). Imaging demonstrated decreased lumen occlusion of 85% (p = 0.005) in distal sections, 84% (p = 0.001) in middle sections and 81% (p = 0.002) in proximal sections (Fig. 4b).
The micropattern prevents airway narrowing. (a) Representative images of reductions in cross-sectional area due to secretion accumulation in standard care ETTs (top) and micropatterned ETTs (bottom). Standard care ETTs show an increase in accumulated material compared to the micropatterned ETTs in all sections. The black areas inside the luminal portion of each tube are accumulated artificial mucus. (b) The graph shows that micropatterned ETTs have significantly less reduction in cross-sectional area compared to standard care ETTs in all three sections along the tubes. Error bars represent standard of the mean from three individual experiments.
In Vivo Airway Patency Model
Shortly after ETT placement the animals had frothy and wet respiratory secretions in the ETT. Approximately one-third of the way through the study the animals’ respiratory secretions thickened while retaining moisture. Mucus accumulation in tracheal tubes following 24 h of intubation was reduced 45% (p = 0.103) by total weight in micropatterned ETTs compared to standard care ETTs (Fig. 5a). Volume of total mucus, as measured using computed tomography (CT), was reduced 61% (p < 0.0005) in micropatterned ETTs compared to standard care ETTs (Fig. 5b).
Preclinical sheep model of ETT occlusion. (a) Volume of accumulated airway secretions was reduced by 61% (p < 0.001, *) in micropatterned ETTs compared to standard care ETTs. (b) Micropatterned ETTs had 45% (p = 0.103) less mucus weight compared to standard care ETTs. (c) Representative images of mucus in cross-sectioned ETTs following extubation.
Lumen occlusion was expected to impact pressure required to deliver fixed volume during mechanical ventilation. Requisite pressure increased during the course of ventilation in both animals. However, consistent with the loss of lumen volume, the peak inspiratory pressure increase over time between 8 and 24 h, after the head of the animal was raised to a 12° (±1.5°) angle, was 49% (p = 0.005) greater with standard care ETTs compared to micropatterned ETTs (Fig. 6).
In vivo Airway Patency Model. Five sheep (2 with standard care and 3 with micropatterned ETTs) were evaluated. Total mechanical ventilation time was divided into two intervals: 0–8 and 8–24 h (indicated in the graph). Data were collected continually during each interval for each device type to produce a linear regression determination of average peak inspiratory pressure over time. Standard care and micropatterned regression graphs are presented independent from each other for clarity. The solid lines in the graphs represent the average peak inspiratory pressure over time for each ETT type while the broken lines represent the 95% prediction intervals for each surface type. The change in peak inspiratory pressure over time for each surface is indicated in the table along with the percent reduction comparing micropatterned to standard care ETTs. A 49% (p = 0.005) reduction in peak inspiratory pressure increase over time was measured on micropatterned ETTs after raising the animal head between 8 and 24 h of ventilation compared to standard care ETTs. (nd refers to no difference).
Discussion
Luminal narrowing of ETTs due to the rapid accumulation of respiratory secretions has significant clinical implications including increased ventilation pressures, difficulty in weaning patients from mechanical ventilation31 and emergence of biofilm-related infections.11 Similar to previous studies,28 the micropatterned surface was capable of limiting biofilm accumulation compared to a standard care device surface (Fig. S1). Surprisingly, the sliver-coated ETT was much less effective at reducing biofilm accumulation compared to planktonic in vitro cultures.36 This is likely due to the lack of antifouling capacity of the silver-coated device. Antifouling was evaluated further as this study examines the efficacy of a novel micropatterned ETT primarily designed to prevent occlusion via newly developed in vitro and in vivo models for demonstrating reduced occlusion. The in vitro AP model described here recapitulates the interactions between airway management devices and mucus. Artificial mucus occluded standard care ETTs tested in the in vitro AP model resulting in a decrease in cross sectional area similar to clinical investigations in patients. Standard care ETT lumen occlusion ranged from 12.5 to 39.5% (Fig. 4b) in the in vitro AP model and from 6.8 to 28.4% in ETTs obtained from patients in a clinical study.31 The loss of cross-sectional area available for ventilation due to mucus accumulation leads to increased resistance to airflow that, according to the Blasius equation, is inversely proportional to the radius raised to the fifth power.4,31 Consequently, even small reductions in lumen diameter due to secretion accumulation significantly impact respiratory mechanics. The most occluded standard care ETTs in these experiments, 39.5% occlusion, compared to 12.3% occlusion in the most occluded micropatterned ETTs, resulted in a 6.4-fold theoretical increase in airway resistance as calculated by the Blasius equation.
The impact of ETT occlusion was further evaluated using a preclinical sheep model of mechanical ventilation. Previous studies have used similar methods to evaluate biofilm formation or suctioning methods.23,46 Sheep were chosen for the model due to their copious mucus production, which allows for consistent mucus aspiration among individual sheep. Sheep were held flat for 8 h, and then the table was maximally tilted to mimic the 30° elevated head-of-bed used in intensive care units. Along with multiple ventilator readings and animal vital signs, peak inspiratory pressure was monitored throughout the study. Tidal volume was expected to be a significant covariant (p ≤ 0.040) affecting peak inspiratory pressure over time among animals. Therefore, tidal volume was incorporated in the analysis of significant peak inspiratory pressure change over time. Peak inspiratory pressure increased over the 24 h study in both standard care and micropatterned ETTs, indicative of changes in respiratory mechanics from endotracheal tube lumen narrowing and changes in lung compliance. The supine sheep positioning likely contributed to poor lung compliance over time, but sheep positioning was consistent regardless of the ETT used. While the sheep were horizontal, prior to 8 h, there was no difference in peak inspiratory pressure between standard care and micropatterned ETTs (Fig. 6). After the animal head was raised, the increase in peak inspiratory pressure over time was significantly greater for sheep with standard care ETTs compared to micropatterned ETTs (Fig. 6). The reduced occlusion in micropatterned ETTs resulted in lower peak inspiratory pressures during set tidal volume ventilation compared to standard care ETTs. The micropatterned ETTs prevented respiratory secretions from fouling the ETT lumen; instead the secretions were more easily drained from the ETT. This passive antifouling mechanism ultimately produced a 49% (p = 0.005) percent reduction in peak inspiratory pressure increase after raising the animal head between 8 and 24 h of ventilation. Importantly, the 24 h sheep intubation model accurately simulated clinical scenarios of ventilation and clinically relevant amount of mucus accumulation that result in occlusion.
Similar to the results seen in vitro, the micropatterned tubes had 45% (p = 0.103) less mucus by weight compared to the standard care ETTs. Furthermore, the micropattern resulted in 61% (p < 0.0005) less mucus volume as measured by CT following extubation. The amount of mucus observed in the standard care ETTs was sufficient to generate restricted and more turbulent airflow capable of requiring greater pressures to deliver a fixed tidal volume to the animals.15,18 Together these data justify the further development and testing of the micropatterned ETT to reduce luminal occlusion and the associated ventilation complications.
Airway management devices that reduce accumulation of secretions without reliance on suction are crucial to mitigate patient complications such as increased work of breathing,5 abrupt airway obstruction,6 prolonged ventilation due to failure to wean18 and disrupted ventilation due to suction cleaning.19 Collectively, results presented here indicate that micropatterned ETTs may lead to improved airway patency during intubation by reducing accumulation of secretions within an ETT.
References
Balonov, K., A. D. Miller, A. Lisbon, and A. M. Kaynar. A novel method of continuous measurement of head of bed elevation in ventilated patients. Intensiv. Care Med. 33:1050–1054, 2007.
Bechert, W. D., M. Bruse, and W. Hage. Experiments with three-dimensional riblets as an idealized model of shark skin. Exp. Fluids 28:403–412, 2000.
Berra, L., A. Coppadoro, E. A. Bittner, T. Kolobow, P. Laquerriere, J. R. Pohlmann, S. Bramati, J. Moss, and A. Pesenti. A clinical assessment of the Mucus Shaver: A device to keep the endotracheal tube free from secretions. Crit. Care Med. 40:119–124, 2012.
Bock, K. R., P. Silver, M. Rom, and M. Sagy. Reduction in tracheal lumen due to endotracheal intubation and its calculated clinical significance. CHEST J. 118:468–472, 2000.
Boqué, M. C., B. Gualis, A. Sandiumenge, and J. Rello. Endotracheal tube intraluminal diameter narrowing after mechanical ventilation: Use of acoustic reflectometry. Intensiv. Care Med. 30:2204–2209, 2004.
Branson, R. D. Secretion management in the mechanically ventilated patient. Respir. Care 52:1328–1347, 2007.
Branson, R. D., D. Gomaa, and D. Rodriquez. Management of the Artificial airway. Respir. Care 59:974–990, 2014.
Carman, M. L., T. G. Estes, A. W. Feinberg, J. F. Schumacher, W. Wilkerson, L. H. Wilson, M. E. Callow, J. A. Callow, and A. B. Brennan. Engineered antifouling microtopgraphies—correlating wettability with cell attachment. Biofouling 22:11–21, 2006.
Chastre, J., and J. Y. Fagon. Ventilator-associated pneumonia. Am. J. Respir. Crit. Care Med. 165:867–903, 2002.
Coppadoro, A., G. Bellani, A. Bronco, R. Borsa, A. Lucchini, S. Bramati, L. Avalli, R. Marcolin, and A. Pesenti. Measurement of endotracheal tube secretions volume by micro computed tomography (MicroCT) scan: An experimental and clinical study. BMC Anesthesiol. 14:22, 2014.
Danin, P. E., E. Girou, P. Legrand, B. Louis, R. Fodil, C. Christov, J. Devaquet, D. Isabey, and L. Brochard. Description and microbiology of endotracheal tube biofilm in mechanically ventilated subjects. Respir. Care 60:21–29, 2015.
Dasta, J. F., T. P. McLaughlin, S. H. Mody, and C. T. Piech. Daily cost of an intensive care unit day: The contribution of mechanical ventilation. Crit. Care Med. 33:1266–1271, 2005.
Decker, J. T., J. T. Sheats, and A. B. Brennan. Engineered antifouling microtopographies: Surface pattern effects on cell distribution. Langmuir 30:15212–15218, 2014.
E2647-13 A. Standard test method for quantification of Pseudomonas aeruginosa biofilm growth using drip flow biofilm reactor with low shear and continuous flow, 2013.
El-Khatib, M. F., A. Husari, G. W. Jamaleddine, C. M. Ayoub, and P. Bou-Khalil. Changes in resistances of endotracheal tubes with reductions in the cross-sectional area. Eur. J. Anaesthesiol. 25:275–279, 2008.
Ezingeard, E., E. Diconne, S. Guyomarc’h, C. Venet, D. Page, P. Gery, R. Vermesch, M. Bertrand, J. Pingat, B. Tardy, J.-C. Bertrand, and F. Zeni. Weaning from mechanical ventilation with pressure support in patients failing a T-tube trial of spontaneous breathing. Intensiv. Care Med. 32:165–169, 2006.
Frengley, R. W., D. N. Closey, J. W. Sleigh, and J. M. Torrance. The effect of closed system suction on airway pressures when using the Servo 300 ventilator. Crit. Care Resusc. 3:230–235, 2001.
Kawati, R., M. Lattuada, U. Sjöstrand, J. Guttmann, G. Hedenstierna, A. Helmer, and M. Lichtwarck-Aschoff. Peak airway pressure increase is a late warning sign of partial endotracheal tube obstruction whereas change in expiratory flow is an early warning sign. Anesth. Analg. 100:889–893, 2005.
Kirton, O. C., M. J. Banner, A. Axelrad, and G. Drugas. Detection of unsuspected imposed work of breathing: Case reports. Crit. Care Med. 21:790–795, 1993.
Kirton, O. C., C. B. DeHaven, J. P. Morgan, J. Windsor, and J. M. Civetta. ELevated imposed work of breathing masquerading as ventilator weaning intolerance. Chest 108:1021–1025, 1995.
Kuchma, S. L., K. M. Brothers, J. H. Merritt, N. T. Liberati, F. M. Ausubel, and G. A. O’Toole. BifA, a cyclic-Di-GMP phosphodiesterase, inversely regulates biofilm formation and swarming motility by Pseudomonas aeruginosa PA14. J Bacteriol. 189:8165–8178, 2007.
Lai, S. K., Y.-Y. Wang, D. Wirtz, and J. Hanes. Micro- and macrorheology of mucus. Adv. Drug Deliv. Rev. 61:86–100, 2009.
Li, Bassi G., F. Curto, A. Zanella, M. Stylianou, and T. Kolobow. A 72-hour study to test the efficacy and safety of the “Mucus Slurper” in mechanically ventilated sheep. Crit. Care Med. 35:906–911, 2007.
Long, C. J., J. A. Finlay, M. E. Callow, J. A. Callow, and A. B. Brennan. Engineered antifouling microtopographies: Mapping preferential and inhibitory microenvironments for zoospore attachment. Biofouling 26:941–952, 2010.
Long, C. J., J. F. Schumacher, P. Robinson, II, J. A. Finaly, M. E. Callow, J. A. Callow, and A. B. Brennan. A model that predicts the attachment behavior of Ulva linza zoospores on surface topography. Biofouling 26:411–419, 2010.
Magin, C. M., J. A. Finlay, G. Clay, M. E. Callow, J. A. Callow, and A. B. Brennan. Antifouling performance of cross-linked hydrogels: Refinement of an attachment model. Biomacromolecules 12:915–922, 2011.
Magin, C. M., C. J. Long, S. P. Cooper, L. K. Ista, G. P. Lopez, and A. B. Brennan. Engineered antifouling microtopographies: The role of Reynolds number in a model that predicts attachment of zoospores of Ulva and cells of Cobetia marina. Biofouling 26:719–727, 2010.
May, R., M. Hoffman, M. Sogo, A. Parker, G. O’Toole, A. Brennan, and S. Reddy. Micro-patterned surfaces reduce bacterial colonization and biofilm formation in vitro: Potential for enhancing endotracheal tube designs. Clin. Transl. Med. 3:8, 2014.
Mietto, C., K. Foley, L. Salerno, J. Oleksak, R. Pinciroli, J. Goverman, and L. Berra. Removal of endotracheal tube obstruction with a secretion clearance device. Respir. Care 59:e122–e126, 2014.
Mietto, C., R. Pinciroli, N. Patel, and L. Berra. Ventilator associated pneumonia: Evolving definitions and preventive strategies. Respir. Care 58:990–1007, 2013.
Mietto, C., R. Pinciroli, A. Piriyapatsom, J. G. Thomas, L. Bry, M. L. Delaney, A. Du Bois, J. Truelove, J. B. Ackman, G. R. Wojtkiewicz, M. Nahrendorf, R. M. Kacmarek, and L. Berra. Tracheal tube obstruction in mechanically ventilated patients assessed by high-resolution computed tomography. Anesthesiology 121:1226–1235, 2014.
Oto, J., H. Imanaka, E. Nakataki, R. Ono, and M. Nishimura. Potential inadequacy of automatic tube compensation to decrease inspiratory work load after at least 48 hours of endotracheal tube use in the clinical setting. Respir. Care 57:697–703, 2012.
Pardee, A. B., F. Jacob, and J. Monod. The genetic control and cytoplasmic expression of “inducibility” in the synthesis of β-galactosidase by E. coli. J. Mol. Biol. 1:165–178, 1959.
Pedersen, C. M., M. Rosendahl-Nielsen, J. Hjermind, and I. Egerod. Endotracheal suctioning of the adult intubated patient—What is the evidence? Intensiv. Crit. Care Nurs. 25:21–30, 2009.
Pinheiro, J., D. Bates, S. DebRoy, D. Sarkar, and R-Core-Team. nlme: Linear and Nonlinear Mixed Effects Models. Vienna: Springer, 2013.
Rello, J., B. Afessa, A. Anzueto, A. C. Arroliga, M. E. Olson, M. I. Restrepo, S. S. Talsma, R. L. Bracken, and M. H. Kollef. Activity of a silver-coated endotracheal tube in preclinical models of ventilator-associated pneumonia and a study after extubation. Crit. Care Med. 38:1135–1140, 2010.
Rumbak, M. J., F. W. Walsh, W. M. Anderson, M. W. Rolfe, and D. A. Solomon. Significant tracheal obstruction causing failure to wean in patients requiring prolonged mechanical ventilation: A forgotten complication of long-term mechanical ventilation. Chest 115:1092–1095, 1999.
Samet, J. M., and P.-W. Cheng. The role of airway Mucus in pulmonary toxicoloy. Environ. Health Perspect. 102:89–103, 1994.
Schumacher, J. F., M. L. Carman, T. G. Estes, A. W. Feinberg, L. H. Wilson, M. E. Callow, J. A. Callow, J. A. Finlay, and A. B. Brennan. Engineered antifouling microtopographies—effect of feature size, geometry, and roughness on settlement of zoospores of the green alga Ulva. Biofouling 23:55–62, 2007.
Schumann, S., M. Lichtwarck-Aschoff, C. Haberthür, C. A. Stahl, K. Möller, and J. Guttmann. Detection of partial endotracheal tube obstruction by forced pressure oscillations. Respir. Physiol. Neurobiol. 155:227–233, 2007.
Sriramulu, D. D., H. Lünsdorf, J. S. Lam, and U. Römling. Microcolony formation: a novel biofilm model of Pseudomonas aeruginosa for the cystic fibrosis lung. J. Med. Microbiol. 54:667–676, 2005.
Stenqvist, O., S. Lindgren, S. Kárason, S. Söndergaard, and S. Lundin. Warning! suctioning. A lung model evaluation of closed suctioning systems. Acta Anaesthesiol. Scand. 45:167–172, 2001.
Tanios, M. A., M. L. Nevins, K. P. Hendra, P. Cardinal, J. E. Allan, E. N. Naumova, and S. K. Epstein. A randomized, controlled trial of the role of weaning predictors in clinical decision making. Crit. Care Med. 34:2530–2535, 2006.
Team R. C. R: A Language and Environment for Statistical Computing. Vienna: Springer, 2013.
Thomas, J. The Role of Biofilms in Device-Related Infections: Biofilms and Ventilation. New York: Springer, 2009.
Trawoger, R., T. Kolobow, M. Cereda, and M. E. Sparacino. Tracheal mucus velocity remains normal in healthy sheep intubated with a new endotracheal tube with a novel laryngeal seal. Anesthesiology 86:1140–1144, 1997.
Tung, A., and S. E. Morgan. Modeling the effect of progressive endotracheal tube occlusion on tidal volume in pressure-control mode. Anesth. Analg 95:192–197, 2002.
Valentini, I., E. Tonveronachi, C. Gregoretti, C. Mega, L. Fasano, L. Pisani, and S. Nava. Different tracheotomy tube diameters influence diaphragmatic effort and indices of weanability in difficult to wean patients. Respir. Care 57:2012–2018, 2012.
Villafane, M., G. Cinnella, F. Lofaso, D. Isabey, A. Harf, F. Lemaire, and L. Brochard. Gradual reduction of endotracheal tube diameter during mechanical ventilation via different humidification devices. Anesthesiology 85:1341–1349, 1996.
Williams, Z., R. Chan, and E. Kelly. A simple device to increase rates of compliance in maintaining 30-degree head-of-bed elevation in ventilated patients. Crit. Care Med. 36:1155–1157, 2008.
Wilson, A. M., D. M. Gray, and J. G. Thomas. Increases in endotracheal tube resistance are unpredictable relative to duration of intubation. CHEST J. 136:1006–1013, 2009.
Acknowledgments
The authors thank veterinary technicians at Wake Forest, Andrew Douglas, Magan Lane, Eric McCloud, and Tonya Calhoun, for assistance with completing the animal studies. B. C. Stevenson for imaging and characterization of micropatterned samples as well as J. Page for machining and assembling the airway patency model test fixture.
Conflict of Interest
EMM, CMM, MRM, RMM, MMH and STR are all employees of Sharklet Technologies, Inc. ABB is a paid consultant of Sharklet Technologies, Inc.
Financial Support
National Institutes of Health National Heart, Lung and Blood Institute (2R44HL110444-02).
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor John H. Linehan oversaw the review of this article.
Ethan E. Mann and Chelsea M. Magin have contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mann, E.E., Magin, C.M., Mettetal, M.R. et al. Micropatterned Endotracheal Tubes Reduce Secretion-Related Lumen Occlusion. Ann Biomed Eng 44, 3645–3654 (2016). https://doi.org/10.1007/s10439-016-1698-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-016-1698-z