Abstract
The cardiorenal syndrome is a clinical manifestation of the bidirectional interaction between the heart and kidneys. Evaluating renal function is an essential part of the assessment of every cardiac patient. It has become clear that serum creatinine is not an accurate enough marker of glomerular filtration rate (GFR) and should not be used to evaluate kidney dysfunction. Creatinine-based estimates of GFR are preferred, but require renal function to be stable and are not suitable when changes in kidney function occur. Cystatin C (CysC) has been the target of much interest in the search for an alternative measure of GFR. As an endogenous biomarker, CysC possesses many of the properties required of a good marker of renal function. Compared with that of creatinine, plasma concentrations of CysC are less influenced by factors other than GFR. Consequently, CysC correlates with true GFR more accurately than creatinine. Equations for estimating GFR from CysC values have also been developed, which makes values easier to interpret and facilitates the clinical use of this new marker. The use of CysC in acute kidney injury has also shown promising results. CysC has been studied as a risk marker for prognosis in cardiovascular disease. This effect is attributed to the strong impact of renal dysfunction on progressive cardiovascular disease and impaired survival. Higher levels of CysC have consistently been predictive of incident or recurrent cardiovascular events and adverse outcomes. CysC is a predictor of the development of heart failure and increased levels of CysC have an independent association with higher mortality in both chronic and acute heart failure. In conclusion, CysC appears to be an interesting marker of renal function and is useful for risk stratification in heart failure.
Similar content being viewed by others
Introduction
The recognition of the importance of the cardiorenal syndrome has brought about the need for accurate and timely assessment of renal function in patients with cardiovascular disease [1]. The term renal function being synonymous with glomerular filtration rate (GFR) in this setting. Creatinine has served as a marker of renal function for several decades. However, this marker has several well-known limitations and creatinine-based equations for estimation of GFR (eGFR) were developed to overcome some of these inadequacies [2]. Unfortunately, the use of these equations for estimation of renal function emerged rather slowly outside the field of nephrology. In addition, estimation equations are reliable only in stable conditions and should not be used when rapid changes of renal function occur. The lack of alternative measures for easy assessment of renal function has to date forced clinicians to put their trust in creatinine.
Ideally, a marker of renal function is an easily measured endogenous substance with constant production, which is freely filtrated in the glomeruli of the kidneys. It should not be secreted or reabsorbed in the renal tubules, nor should any extrarenal degradation (liver, intestine) occur since all these mechanisms would affect urine or plasma concentrations through pathways not related to GFR. The marker should be independent of age, gender, race, diet, body composition, disease states, and medications. Thus, the concentration of the marker in plasma would be directly and inversely related to GFR. Measured levels in urine would also reflect the filtration at the glomerular level.
Cystatin C (CysC) is a small 13-kDa protein with properties making it a candidate for a good marker of GFR. Indeed, CysC possesses many of the characteristics required of an ideal marker of GFR. It is an endogenous substance with constant production, freely filtrated in the glomerulus. There is no tubular secretion or reabsorption, and CysC can nowadays be easily measured [3]. In the last decade, research on the use of CysC as a replacement for creatinine as a marker of renal function has been rapidly growing. Furthermore, several studies have shown CysC to be a strong risk marker for adverse cardiovascular prognosis in various populations. This paper considers whether CysC could be used to improve assessment of renal function both in the acute and in the chronic setting and reviews the literature on CysC as a prognostic risk marker in patients with the cardiorenal syndrome.
Cystatin C as a marker of glomerular filtration rate
CysC was first discovered as an protein in an electrophoretic band in the 1960s and subsequently became characterized as a member of the human cystatin superfamily [4–6]. CysC, a 122 amino acid cysteine protease inhibitor, is produced at a constant rate by all nucleated cells in the body. This is a consequence of CysC being a product of a “housekeeping” gene with stable and continuous expression [3, 4]. As a small-sized protein, CysC is filtrated freely in the glomerulus, with no known extrarenal excretion or degradation. The association of CysC with glomerular filtration rate was described already 25 years ago [7]. In the proximal tubule of the nephron, there is a reuptake and complete degradation of CysC but without any reabsorption into the bloodstream. Normally, only small amounts of CysC are excreted into the urine. Therefore, while plasma levels of CysC have an inverse relationship to kidney function, measurement of urinary CysC cannot be used to assess GFR. The use of urinary CysC as a marker of tubular injury is not discussed here.
In contrast to creatinine, factors like age, gender, diet, and body composition have no or little effect on levels of CysC [3, 4, 8]. Different medical conditions (infection, inflammation, or malignancy) do not appear to alter the levels of CysC with the possible exception of thyroid illness [4]. Although not all studies have found this association, [9, 10] it seems that CysC levels are lower in hypothyroid and higher in hyperthyroid patients and increase and decrease, respectively, when patients are treated to the euthyroid state [11–13]. Data from one in vitro study and one study in patients with renal transplants have suggested that glucocorticoids in high doses affect CysC levels [14, 15], but again not all studies have confirmed that steroids interfere with the relation between CysC and GFR [16]. The association of CysC with inflammatory markers described by some authors [8, 17, 18] is expected, as inflammation is activated in renal insufficiency [19, 20]. The only study adjusting for measured GFR still found a weak relationship between C-reactive protein (CRP) and CysC [21].
Since the development of rapid automated assays for measurement of CysC, many studies have assessed the relationship of CysC with GFR and compared it with creatinine [4, 22–24]. Several authors have found that CysC is a better marker of GFR than creatinine, creatinine clearance, or eGFR, especially in patients with mild impairment of renal function [3, 16, 22, 25–28]. Although not all studies have seen advantages with CysC over creatinine or creatinine-based equations [29, 30], two meta-analyses consistently showed CysC to be superior to creatinine as a marker of GFR [31, 32]. In patients with type 1 diabetes mellitus, CysC was more accurate than creatinine for assessing high levels of GFR and hyperfiltration states [33–35].
Lately, reports on an association between CysC and factors unrelated to GFR have been published [8, 9, 21, 36]. A correlation between CysC and age is to be expected, as GFR declines with age [37]. Conflicting data exist about whether CysC levels vary with gender, but after the age of 60, no difference between men and women is seen [4, 22, 38]. Rule et al. used iothalamate clearance to establish the relationship between CysC and GFR in healthy adults (n = 50), patients with chronic kidney disease (CKD) (n = 204) and transplant recipients (n = 206) and found that CysC reflected GFR better than creatinine in all three groups. Some papers examining the association of CysC levels with other factors lacked direct GFR measurements [8, 36] and have compared CysC with creatinine or adjusted for urinary creatinine clearance or eGFR, which diminish the strength of these observations.
Attempts to convert CysC values (mg/l) to corresponding GFR (ml/min) have resulted in multiple equations in the literature [29, 39–44]. The largest study so far comparing measured GFR with GFR estimates from CysC and creatinine was carried out as pooled analysis of cohorts with CKD [41]. CysC was indeed less influenced than creatinine by non-renal factors, but a small variability (<10%) in CysC according to age, gender, and race was still observed. The authors found that although GFR estimated from CysC alone performed nearly as well as eGFR from the MDRD equation, incorporating age, gender, and race or even creatinine with CysC reduced bias in the GFR estimate. As acknowledged also in the paper, this comparison was made in CKD patients for whom the MDRD equation was developed and therefore has optimal performance. A very recent analysis on the performance of CysC-based estimates of GFR found no advantage over the MDRD equation in a large population survey [45]. As this was not a CKD cohort, there is accumulating evidence suggesting that even though CysC outperforms creatinine as a marker for GFR, the current equations for estimating GFR from CysC values may not necessarily be superior to the MDRD equation, at least in CKD patients and in the general population. Nevertheless, it is possible that CysC-based estimates of GFR still perform better in populations where the MDRD equation lacks accuracy. CysC has not been evaluated against measured GFR in subjects with heart failure.
The influence of body composition or other non-renal factors on CysC levels is much smaller than on creatinine, and CysC has true potential for easy and reliable estimation of renal function. The use of CysC for assessing kidney function could be advocated in populations where the disadvantages of creatinine might be particularly evident (elderly populations with many comorbidities, hospitalized, cachectic or amputated patients) or where early detection of mild impairment of renal function (transplant recipients, diabetics, cardiovascular disease) is of clinical importance [6, 28, 46–50]. Compared with creatinine or creatinine-based equations, CysC would allow better and more accurate assessment of renal function in clinical practice without affecting simplicity or availability. The characteristics of CysC and creatinine are compared in Table 1.
Cystatin C in acute kidney injury
Diagnosis of acute kidney injury (AKI), i.e., a rapid decline in GFR, has been challenging. For half a century, creatinine and urea were the only markers available to assess changes in renal function occurring within hours or days. The dilemma of creatinine being a slow and insensitive marker for change in GFR is not discussed further here, but detection of AKI with creatinine will inevitably be late and any interventions to prevent kidney injury usually futile. Since creatinine-based eGFR-equations apply only when renal function is stable, as in CKD populations used for their development, they are not suitable in the setting of AKI. The novel markers of tubular injury have the potential of early detection of kidney damage (see also paper by K. Damman [97]). Assuming that tubular injury precedes a decrease in GFR and that therapeutic interventions can be instituted to prevent or alleviate this decline, the tubular markers have a prospective role in clinical practice. Nevertheless, a reliable and rapid marker for the detection of GFR decline should also be available. As discussed previously, CysC has the potential to fulfill these requirements as a better marker of GFR than creatinine and being less affected by non-renal factors [31, 32].
There are a few studies that have investigated the use of CysC as an alternative to creatinine as a marker of GFR in AKI, mostly in the intensive care setting or after cardiac surgery. Studies assessing CysC in AKI have mainly focused on two aspects: whether CysC rises earlier than creatinine or whether CysC is able to predict a secondary outcome (need for renal replacement therapy, length of stay or in-hospital mortality) better than creatinine [39, 51–54]. The performance of CysC for diagnosis of AKI has been evaluated against creatinine-based AKI-criteria (RIFLE or AKIN) [55, 56] as reference.
Most studies using serial sampling of renal markers show CysC to be an earlier marker of AKI [39, 51, 52]. CysC had better correlation with urinary creatinine clearance, superior sensitivity to detect renal dysfunction than creatinine, and high CysC levels predicted mortality in ICU patients with AKI [54, 57]. One study assessed the ability of a single CysC measurement to predict the requirement of dialysis or in-hospital death in AKI and compared its predictive performance with creatinine, serum urea nitrogen levels, and urine output. All measures of renal function were independent predictors of the combined end point with similar odds ratio. However, adding renal function to a model with general clinical measures did not improve the area under the curve (AUC) of the receiver operating characteristics (ROC) for the prediction of the combined end point [58].
Three studies have assessed CysC as a marker of AKI after cardiac surgery [51, 53, 59]. In the first one, CysC and serum neutrophil gelatinase–associated lipocalin (NGAL), a novel marker of kidney injury, were compared with creatinine and urea for prediction of AKI in 100 patients who underwent cardiac surgery [51]. As baseline renal insufficiency is a known risk factor for AKI, it is interesting to note that while preoperative values of the other markers did not differ, CysC levels were higher in the group which subsequently developed AKI (23%) postoperatively. NGAL and CysC levels measured on arrival in ICU were found to be superior to creatinine for the prediction of AKI. At 24 h, all markers showed similar performance statistics as assessed by the ROC curve. Wald et al. also found that levels of CysC, but not creatinine, were higher in the group with subsequent AKI, but the ability of CysC measured 2 h after surgery to predict AKI was only modest [59]. The authors did not extend their analysis of CysC to later time-points. The third study carried out on elderly patients undergoing cardiac surgery showed no statistically significant difference in the performance to detect AKI between CysC (AUC 0.71) and creatinine (AUC 0.66; P = 0.11 for difference) measured on the first postoperative day [53]. In this study, the majority of patients had increases >50% from preoperative levels on day 2 for CysC (9/17) compared with day 3 for creatinine (15/30). Although serial measurements were available in these studies, single values and not changes in CysC were used for prediction of AKI.
Two very recent studies have examined CysC as a marker of AKI outside the cardiac surgery and intensive care unit setting. Soto et al. examined consecutive patients admitted to the emergency department and measured both serum and urinary CysC [60]. While urinary CysC was useful only in differentiating patients with AKI (21%) from those with normal renal function (51%), serum CysC had excellent early discriminative properties for AKI, both compared with normal renal function and adjudicated prerenal azotemia (26%). Creatinine was not able to differentiate between AKI and prerenal azotemia, but performed well in prediction of AKI. In a cohort hospitalized for acute heart failure (AHF), CysC increased by 0.3 mg/l (AKICysC) in 16% of patients, a higher incidence than observed with the common definition of AKI (rise >0.3 mg/dl) with creatinine (9%) [61]. AKICysC was associated with increased length of hospital stay and was an independent predictor of mortality up to 90 days. Interesting, the patients identified as having AKI by the two markers were not quite the same. This observation was also made in another study where both creatinine and CysC rose above a predefined cutoff at the same time-point in only 20–25% experiencing AKI. In over half of the subjects with AKI, CysC not only preceded creatinine in time, but although a clear rise in CysC was observed, creatinine levels remained below the diagnostic threshold in many patients [52].
There are important differences between populations experiencing AKI in the ICU [39, 52], after cardiac surgery [51, 53, 59] or contrast induced nephropathy [62, 63] and other cohorts. First, the incidence of AKI in the ICU is much higher than in other hospitalized patients. Second, timing the injury in patients with contrast nephropathy and cardiac surgery is more straightforward, and the disturbances associated with contrast administration or surgical trauma can be regarded as a “one-hit” injury. While AKI after cardiac surgery resulted in a significant rise in creatinine (111%), the peak creatinine value was observed only on the third day after surgery [51]. As serum CysC is not a marker of injury, changes in CysC levels may not be immediate, but occur within hours as GFR declines. CysC can detect a decline in GFR within the first 24 h. In severe AKI, there may be less advantages compared with creatinine if assessed beyond the first postoperative day [51, 53]. If AKI ensues more gradually, with a minor and subsequently progressive decline in GFR, CysC could (a) detect minor changes in GFR and (b) at an earlier time-point compared with creatinine.
All these studies defined AKI by creatinine, which certainly is a methodological dilemma that should be acknowledged [64]. In two small studies on diabetics evaluating slower changes in GFR over time, changes in levels of CysC correlated well with the decline in measured GFR, and CysC was a better marker of decline in renal function than creatinine [49, 65]. CysC is also an accurate measure of acute changes in GFR [34]. The independence from height, gender, age and muscle mass is advantageous. In particular, patients with changes in muscle metabolism or mass (elderly, hospitalized or heart failure patients with edema), could benefit from estimating renal function with CysC both in the stable setting and as an alternative to creatinine for detection of AKI.
Adopting novel and better renal markers, both injury and functional, into clinical practice is to be expected and long waited for. The clinical uptake of CysC has been rather slow. CysC has been regarded a promising novel marker of renal function for long, but only recently has the data from different clinical populations and settings been accumulating. Although not all studies find clear advantage with the use of CysC, there is evidence for a potential improvement in diagnostic and prognostic performance. Concerns about costs have been raised but CysC is not more expensive than troponin T (TnT), the use of which is highly established in acute coronary syndromes (ACS). Moreover, the cost of CysC is far less than NT-proBNP, a biomarker recommended for diagnostic purposes by the guidelines, but for which the use in prognostication or guiding treatment in heart failure is less clear.
Equations for transforming CysC values to GFR estimates have been developed, but not widely validated. Differences in laboratory assays with different reference values makes comparison of studies and use of equations very difficult [66]. The International Federation for Clinical Chemistry and Laboratory Medicine published the first certified reference material for standardization of CysC laboratory platforms in the second half of 2010 [67]. Hopefully, this will help to calibrate different CysC assays, validate the GFR equations and subsequently improve the availability and interpretation of CysC values.
Cystatin C for prediction of cardiovascular events
The emergence of renal function as strong prognostic factor in patients with cardiovascular disease in combination with the search for new biomarkers for risk prediction has been the driving force in assessing the utility and prognostic impact of CysC on cardiovascular outcomes. CysC has been studied intensively as a risk marker for poor prognosis or cardiovascular disease in various populations at risk.
Elderly populations
A landmark paper examining how CysC influences cardiovascular outcomes in a broad population was published in 2005 [68]. Levels of CysC were measured from over four thousand elderly ambulatory persons without previous history of cerebrovascular or coronary heart disease in the Cardiovascular Health Study. During a median of 7.4-years follow-up, higher baseline CysC levels were significantly associated with increasing all-cause and cardiovascular mortality. Moreover, higher rates of myocardial infarction and stroke were also observed in the top quintile of CysC [68]. Similar effects of CysC on mortality, but without predicting incident myocardial infarction or stroke during follow-up, were found in a slightly older cohort [69, 70]. A secondary analysis of patients without renal insufficiency (eGFR ≥60 ml/min) at baseline in the Cardiovascular Health Study cohort showed that CysC levels had a significant effect on all-cause, cardiovascular and non-cardiovascular mortality, incident myocardial infarction, stroke, and heart failure, while creatinine was not associated with adverse outcomes [71]. CysC was a better predictor of death and cardiovascular events than creatinine in these studies.
Coronary artery disease
CysC has been a consistent marker of poor prognosis in patients with coronary artery disease (CAD). In stable CAD patients, high CysC levels have been associated with 2–3-fold risk of death, cardiovascular event or heart failure hospitalization during 3 years of follow-up [72, 73]. Again this risk increase was present both in patients with and without renal insufficiency defined as eGFR <60 ml/min at baseline [72]. In patients with CAD and eGFR >60 ml/min, CysC was a strong predictor of cardiovascular death [74]. Compared with the patients in the first quartile, patients in the top CysC quartile had a five times higher adjusted risk of cardiovascular death. Data from a large population in the United States also showed that in patients without CKD (eGFR ≥60 ml/min and without albuminuria) higher CysC levels were associated with increased prevalence of myocardial infarction, angina pectoris symptoms, and stroke [75].
In patients with ACS including both ST-elevation and non-ST-elevation myocardial infarction, CysC has been an independent predictor of death or death and myocardial infarction during follow-up [10, 76, 77].
Heart failure
Given the association with mortality and various cardiovascular events described earlier, it is not surprising that higher levels of CysC also predict the incidence of heart failure (Table 2). For each quartile of CysC, there was a stepwise increase in the risk of developing heart failure independently of other risk factors [71, 78]. This relation was not seen with creatinine. One study reported that the association between CysC and heart failure was present only in hypertensive patients, although mean measured blood pressure was similar between CysC categories [79].
CysC increases the risk of both systolic and diastolic heart failure, though the risk of developing diastolic heart failure was evident mostly in patients with the highest CysC concentrations [80]. Cross-sectional studies report that levels of CysC relate to disturbances in diastolic function, but not measures of systolic function. In patients without a history of heart failure, elevated CysC is associated with left ventricular hypertrophy (increased wall thickness and higher left ventricular mass) and diastolic dysfunction but not with left ventricular ejection fraction (LVEF) [81–83]. In clinical heart failure, CysC levels are not correlated with LVEF but with other indices of cardiac dysfunction [84].
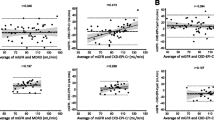
CysC increases with severity of heart failure as measured by NYHA functional class [84, 85]. Patients in the Cardiovascular Health Study with heart failure at the baseline visit and who subsequently died during follow-up had higher CysC levels compared with patients who survived [86]. CysC has been an independent predictor of mortality in heart failure even after adjustment for baseline creatinine/eGFR or after stratification by eGFR (Fig. 1) [85–87].
Association of CysC levels with mortality in elderly persons with heart failure, stratified by creatinine, and eGFR levels. The figure displays the annual mortality risk for participants with cystatin-C levels above (high) or below (low) the median of 1.26 mg/l. The adjusted hazard ratios (HR) compare high and low cystatin-C levels between subgroups of participants with high creatinine (above median value of 1.05 mg/dl) or low creatinine (<1.05 mg/dl), as well as by high eGFR (>61 ml/min/1.73 m2) or low eGFR (<61 ml/min/1.73 m2). Reproduced from [86] with permission from Elsevier
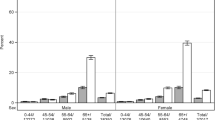
The FINN-AKVA study was the first study to show the effect of CysC on prognosis for patients hospitalized for AHF [88]. There was a stepwise increase in mortality with each tertile of CysC (Fig. 2). CysC levels above median were independently associated with mortality during 12 months of follow-up. Other publications have confirmed that higher levels of CysC are associated with increased mortality in AHF including cohorts with non-Caucasian ethnicities [89–91]. The effect of CysC on mortality in these studies was robust even after adjustment for possible confounders and other factors associated with increased mortality.
Risk stratification in AHF by combining tertiles of cystatin C and NT-proBNP. Increase in mortality at 1 year from 5.2% in patients in the first tertile of both biomarkers (n = 77) to 48.7% in patients in the third tertile (n = 76) of cystatin C and NT-proBNP. Reproduced from [88] with permission by Oxford University press
The finding in some studies that CysC was a predictor of outcome after adjustment for creatinine or creatinine clearance has raised the question about effects not related to renal function [73, 92]. The available data cannot give a definite answer because creatinine clearance or eGFR is not able to fully adjust for true renal function, and large studies with direct measurement of GFR are not likely to be carried out with current methods. Given the documented strong effect of renal dysfunction on outcomes in AHF and the notion that CysC is a better marker of GFR than creatinine, it seems plausible that the superiority of CysC for predicting outcome is directly related to its properties as a marker of kidney function. We have previously reported that an elevated CysC in patients with normal creatinine has a remarkable effect on mortality (Fig. 3) [88]. Studies on other populations with normal or near normal kidney function assessed by creatinine have also documented an increase in incidence of cardiovascular disease and adverse events related to higher CysC levels [71, 74, 75, 93]. In all the studies in ACS, median CysC levels were ≤1.0 mg/l and the negative effect on cardiovascular outcomes was mostly visible in the highest quartile of CysC [10, 76, 77]. Thus, it is most probable that elevated CysC reflects a minor to moderate decline in renal function not detected by creatinine and that this has a substantial effect on prognosis.
Effect on survival of elevated cystatin C in patients with normal creatinine. Kaplan–Meier curves for patients with normal creatinine and normal cystatin C level (upper line) and patients with normal creatinine but elevated cystatin C level (lower line). Mortality at 1 year 12.6 versus 40.4%. Log rank P < 0.0001. Reproduced from [88] with permission by Oxford University press
Cystatin C in chronic kidney disease
For patients with established CKD, a retrospective analysis in the MDRD cohort showed that higher CysC level was a significant predictor of mortality (all-cause and cardiovascular) and progression to kidney failure (dialysis or transplant) during 10 years of follow-up. The risk ratio per standard deviation CysC was similar to that of measured GFR (and creatinine), although CysC showed slightly higher increase in risk of the mortality outcomes [94]. In elderly patients with eGFR ≥60 ml/min, CysC concentration above normal was a strong predictor of CKD, with a four times increased risk of developing eGFR <60 ml/min during 4 years of follow-up [71].
Shlipak and colleagues elegantly compared rates of decline in kidney function assessed by creatinine and CysC in 4,380 elderly persons followed for 7 years.[95] CysC and creatinine values were converted to eGFRCysC and eGFRMDRD, respectively. The authors showed that with eGFRMDRD, mean decline in renal function was 0.4 ml/min/year, and 16% of the population had a rapid decrease (>3 ml/min/year). Surprisingly, 39% were found by eGFRMDRD to have a mean improvement in renal function during follow-up. Overall, the change in eGFRMDRD was rather small in the population, from 79 ml/min at baseline to 78 ml/min at study end. In addition, changes in renal function detected with eGFRMDRD differed significantly by gender and race [95]. For CysC estimates, renal function change was not different in men and women or by race. The mean annual decline for eGFRCysC was 1.8 ml/min and mean eGFRCysC changed from 79 ml/min at baseline to 70 ml/min at final follow-up. Twenty-five percent of patients were categorized as having rapid kidney function decline, and fewer were found to have a positive trend in the annual eGFRCysC [95]. The study also pointed out age as a significant predictor of rapid kidney function decline and found that eGFRCysC identified twice as many patients reaching the end point of CKD (eGFR <60 ml/min) compared with eGFRMDRD. Furthermore, separate analysis of the same cohort showed that this rapid decline in kidney function, measured with either eGFRCysC or eGFRMDRD was associated with 50% increased risk of all-cause or cardiovascular death, irrespective of age, gender, or baseline renal function [96].
Efforts to standardize CysC measurements and validation of eGFRCysC equations give an opportunity for reliable and more accurate evaluation of kidney function in patients with cardiovascular disease. CysC can be considered an easily available marker of cardiovascular risk and with the possibility of identifying high-risk individuals through population- or disease-specific cutoffs. Defining these cutoffs from available and upcoming data still needs to be done, but improved awareness about better ways to assess kidney function is already a step forward. Alongside increasing clinical use of CysC as a measure of kidney function, further studies will be necessary to evaluate whether therapeutic interventions aiming at preserving or improving renal function also can improve prognosis.
Conclusions
CysC is an interesting marker of renal function that accurately reflects GFR. The properties of CysC make it an excellent candidate for assessing renal function in a variety of populations and disease states, both in patients with renal insufficiency and in patients with more preserved renal function. A clear advantage is that levels of CysC are less dependent on non-renal factors than on creatinine. CysC seems to be superior to creatinine and at least equal to creatinine-based estimations of GFR in stable patients. Moreover, CysC shows reliable performance also when changes occur, either rapid or slower deterioration of kidney function during follow-up.
CysC is a strong predictor of outcomes and has been a consistent marker of increased risk for adverse events and death in various cohorts. CysC also predicts cardiovascular events and disease progression of heart failure and renal insufficiency in elderly patients at risk. In particular, CysC has the potential to detect the effect of mild kidney dysfunction on outcome. All this reflects the strong impact on prognosis of the cardiorenal syndrome in cardiovascular disease and in heart failure patients above all. As a potent risk marker in the cardiorenal syndrome, CysC could clearly be a step forward for the assessment of renal function and risk stratification in patients with cardiovascular disease and heart failure.
References
Ronco C, McCullough P, Anker SD et al (2010) Cardio-renal syndromes: report from the consensus conference of the acute dialysis quality initiative. Eur Heart J 31(6):703–711
Levey AS, Coresh J, Greene T et al (2006) Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med 145(4):247–254
Laterza OF, Price CP, Cystatin ScottMG (2002) Cystatin C: an improved estimator of glomerular filtration rate? Clin Chem 48(5):699–707
Seronie-Vivien S, Delanaye P, Pieroni L et al (2008) Cystatin C: current position and future prospects. Clin Chem Lab Med 46(12):1664–1686
Newman DJ (2002) Cystatin C. Ann Clin Biochem 39(Pt 2): 89–104
Filler G, Bokenkamp A, Hofmann W, Le Bricon T, Martinez-Bru C, Grubb A (2005) Cystatin C as a marker of GFR—history, indications, and future research. Clin Biochem 38(1):1–8
Simonsen O, Grubb A, Thysell H (1985) The blood serum concentration of cystatin C (gamma-trace) as a measure of the glomerular filtration rate. Scand J Clin Lab Invest 45(2):97–101
Knight EL, Verhave JC, Spiegelman D et al (2004) Factors influencing serum cystatin C levels other than renal function and the impact on renal function measurement. Kidney Int 65(4):1416–1421
Kottgen A, Selvin E, Stevens LA, Levey AS, Van Lente F, Coresh J (2008) Serum cystatin C in the United States: the Third National Health and Nutrition Examination Survey (NHANES III). Am J Kidney Dis 51(3):385–394
Kilic T, Oner G, Ural E et al (2009) Comparison of the long-term prognostic value of cystatin C to other indicators of renal function, markers of inflammation and systolic dysfunction among patients with acute coronary syndrome. Atherosclerosis 207(2):552–558
Fricker M, Wiesli P, Brandle M, Schwegler B, Schmid C (2003) Impact of thyroid dysfunction on serum cystatin C. Kidney Int 63(5):1944–1947
Jayagopal V, Keevil BG, Atkin SL, Jennings PE, Kilpatrick ES (2003) Paradoxical changes in cystatin C and serum creatinine in patients with hypo- and hyperthyroidism. Clin Chem 49(4):680–681
den Hollander JG, Wulkan RW, Mantel MJ, Berghout A (2003) Is cystatin C a marker of glomerular filtration rate in thyroid dysfunction? Clin Chem 49(9):1558–1559
Risch L, Herklotz R, Blumberg A, Huber AR (2001) Effects of glucocorticoid immunosuppression on serum cystatin C concentrations in renal transplant patients. Clin Chem 47(11):2055–2059
Bjarnadottir M, Grubb A, Olafsson I (1995) Promoter-mediated, dexamethasone-induced increase in cystatin C production by HeLa cells. Scand J Clin Lab Invest 55(7):617–623
Kazama JJ, Kutsuwada K, Ataka K, Maruyama H, Gejyo F (2002) Serum cystatin C reliably detects renal dysfunction in patients with various renal diseases. Nephron 91(1):13–20
Keller CR, Odden MC, Fried LF et al (2007) Kidney function and markers of inflammation in elderly persons without chronic kidney disease: the health, aging, and body composition study. Kidney Int 71(3):239–244
Singh D, Whooley MA, Ix JH, Ali S, Shlipak MG (2007) Association of cystatin C and estimated GFR with inflammatory biomarkers: the Heart and Soul Study. Nephrol Dial Transplant 22(4):1087–1092
Stenvinkel P, Ketteler M, Johnson RJ et al (2005) IL-10, IL-6, and TNF-alpha: central factors in the altered cytokine network of uremia—the good, the bad, and the ugly. Kidney Int 67(4):1216–1233
Cachofeiro V, Goicochea M, de Vinuesa SG, Oubina P, Lahera V, Luno J (2008) Oxidative stress and inflammation, a link between chronic kidney disease and cardiovascular disease. Kidney Int Suppl 74(111):S4–S9
Stevens LA, Schmid CH, Greene T et al (2009) Factors other than glomerular filtration rate affect serum cystatin C levels. Kidney Int 75(6):652–660
Rule AD, Bergstralh EJ, Slezak JM, Bergert J, Larson TS (2006) Glomerular filtration rate estimated by cystatin C among different clinical presentations. Kidney Int 69(2):399–405
Newman DJ, Thakkar H, Edwards RG et al (1995) Serum cystatin C measured by automated immunoassay: a more sensitive marker of changes in GFR than serum creatinine. Kidney Int 47(1):312–318
Kyhse-Andersen J, Schmidt C, Nordin G et al (1994) Serum cystatin C, determined by a rapid, automated particle-enhanced turbidimetric method, is a better marker than serum creatinine for glomerular filtration rate. Clin Chem 40(10):1921–1926
Hoek FJ, Kemperman FA, Krediet RT (2003) A comparison between cystatin C, plasma creatinine and the Cockcroft and Gault formula for the estimation of glomerular filtration rate. Nephrol Dial Transplant 18(10):2024–2031
Harmoinen A, Lehtimaki T, Korpela M, Turjanmaa V, Saha H (2003) Diagnostic accuracies of plasma creatinine, cystatin C, and glomerular filtration rate calculated by the Cockcroft-Gault and Levey (MDRD) formulas. Clin Chem 49(7):1223–1225
Coll E, Botey A, Alvarez L et al (2000) Serum cystatin C as a new marker for noninvasive estimation of glomerular filtration rate and as a marker for early renal impairment. Am J Kidney Dis 36(1):29–34
Pucci L, Triscornia S, Lucchesi D et al (2007) Cystatin C and estimates of renal function: searching for a better measure of kidney function in diabetic patients. Clin Chem 53(3):480–488
Macisaac RJ, Tsalamandris C, Thomas MC et al (2006) Estimating glomerular filtration rate in diabetes: a comparison of cystatin-C- and creatinine-based methods. Diabetologia 49(7):1686–1689
Spanaus KS, Kollerits B, Ritz E et al (2010) Serum creatinine, cystatin C, and beta-trace protein in diagnostic staging and predicting progression of primary nondiabetic chronic kidney disease. Clin Chem 56(5):740–749
Dharnidharka VR, Kwon C, Stevens G (2002) Serum cystatin C is superior to serum creatinine as a marker of kidney function: a meta-analysis. Am J Kidney Dis 40(2):221–226
Roos JF, Doust J, Tett SE, Kirkpatrick CM (2007) Diagnostic accuracy of cystatin C compared to serum creatinine for the estimation of renal dysfunction in adults and children—a meta-analysis. Clin Biochem 40(5–6):383–391
Tan GD, Lewis AV, James TJ, Altmann P, Taylor RP, Levy JC (2002) Clinical usefulness of cystatin C for the estimation of glomerular filtration rate in type 1 diabetes: reproducibility and accuracy compared with standard measures and iohexol clearance. Diabetes Care 25(11):2004–2009
Cherney DZ, Sochett EB, Dekker MG, Perkins BA (2010) Ability of cystatin C to detect acute changes in glomerular filtration rate provoked by hyperglycaemia in uncomplicated Type 1 diabetes. Diabet Med 27(12):1358–1365
Huang SH, Sharma AP, Yasin A, Lindsay RM, Clark WF, Filler G (2011) Hyperfiltration affects accuracy of creatinine eGFR measurement. Clin J Am Soc Nephrol 6(2):274–280
Ognibene A, Mannucci E, Caldini A et al (2006) Cystatin C reference values and aging. Clin Biochem 39(6):658–661
Odden MC, Tager IB, Gansevoort RT et al (2010) Age and cystatin C in healthy adults: a collaborative study. Nephrol Dial Transplant 25(2):463–469
Weinert LS, Prates AB, do Amaral FB, Vaccaro MZ, Camargo JL, Silveiro SP (2010) Gender does not influence cystatin C concentrations in healthy volunteers. Clin Chem Lab Med 48(3):405–408
Herget-Rosenthal S, Marggraf G, Husing J et al (2004) Early detection of acute renal failure by serum cystatin C. Kidney Int 66(3):1115–1122
Grubb A, Nyman U, Bjork J et al (2005) Simple cystatin C-based prediction equations for glomerular filtration rate compared with the modification of diet in renal disease prediction equation for adults and the Schwartz and the Counahan-Barratt prediction equations for children. Clin Chem 51(8):1420–1431
Stevens LA, Coresh J, Schmid CH et al (2008) Estimating GFR using serum cystatin C alone and in combination with serum creatinine: a pooled analysis of 3, 418 individuals with CKD. Am J Kidney Dis 51(3):395–406
Macdonald J, Marcora S, Jibani M et al (2006) GFR estimation using cystatin C is not independent of body composition. Am J Kidney Dis 48(5):712–719
Ma YC, Zuo L, Chen JH et al (2007) Improved GFR estimation by combined creatinine and cystatin C measurements. Kidney Int 72(12):1535–1542
Madero M, Sarnak MJ, Stevens LA (2006) Serum cystatin C as a marker of glomerular filtration rate. Curr Opin Nephrol Hypertens 15(6):610–616
Eriksen BO, Mathisen UD, Melsom T et al (2010) Cystatin C is not a better estimator of GFR than plasma creatinine in the general population. Kidney Int 78(12):1305–1311
Wasen E, Isoaho R, Mattila K, Vahlberg T, Kivela SL, Irjala K (2004) Estimation of glomerular filtration rate in the elderly: a comparison of creatinine-based formulae with serum cystatin C. J Intern Med 256(1):70–78
O’Riordan SE, Webb MC, Stowe HJ et al (2003) Cystatin C improves the detection of mild renal dysfunction in older patients. Ann Clin Biochem 40(Pt 6):648–655
Fliser D, Ritz E (2001) Serum cystatin C concentration as a marker of renal dysfunction in the elderly. Am J Kidney Dis 37(1):79–83
Perkins BA, Nelson RG, Ostrander BE et al (2005) Detection of renal function decline in patients with diabetes and normal or elevated GFR by serial measurements of serum cystatin C concentration: results of a 4-year follow-up study. J Am Soc Nephrol 16(5):1404–1412
Shlipak MG, Praught ML, Sarnak MJ (2006) Update on cystatin C: new insights into the importance of mild kidney dysfunction. Curr Opin Nephrol Hypertens 15(3):270–275
Haase-Fielitz A, Bellomo R, Devarajan P et al (2009) Novel and conventional serum biomarkers predicting acute kidney injury in adult cardiac surgery—a prospective cohort study. Crit Care Med 37(2):553–560
Nejat M, Pickering JW, Walker RJ, Endre ZH (2010) Rapid detection of acute kidney injury by plasma cystatin C in the intensive care unit. Nephrol Dial Transplant 25(10):3283–3289
Ristikankare A, Poyhia R, Kuitunen A et al (2010) Serum cystatin C in elderly cardiac surgery patients. Ann Thorac Surg 89(3):689–694
Bell M, Granath F, Martensson J et al (2009) Cystatin C is correlated with mortality in patients with and without acute kidney injury. Nephrol Dial Transplant 24(10):3096–3102
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P (2004) Acute dialysis quality initiative workgroup. Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) group. Crit Care 8(4):R204–R212
Mehta RL, Kellum JA, Shah SV et al (2007) Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 11(2):R31
Villa P, Jimenez M, Soriano MC, Manzanares J, Casasnovas P (2005) Serum cystatin C concentration as a marker of acute renal dysfunction in critically ill patients. Crit Care 9(2):R139–R143
Perianayagam MC, Seabra VF, Tighiouart H, Liangos O, Jaber BL (2009) Serum cystatin C for prediction of dialysis requirement or death in acute kidney injury: a comparative study. Am J Kidney Dis 54(6):1025–1033
Wald R, Liangos O, Perianayagam MC et al (2010) Plasma cystatin C and acute kidney injury after cardiopulmonary bypass. Clin J Am Soc Nephrol 5(8):1373–1379
Soto K, Coelho S, Rodrigues B et al (2010) Cystatin C as a marker of acute kidney injury in the emergency department. Clin J Am Soc Nephrol 5(10):1745–1754
Lassus JP, Nieminen MS, Peuhkurinen K et al (2010) Markers of renal function and acute kidney injury in acute heart failure: definitions and impact on outcomes of the cardiorenal syndrome. Eur Heart J 31(22):2791–2798
Briguori C, Visconti G, Rivera NV et al (2010) Cystatin C and contrast-induced acute kidney injury. Circulation 121(19):2117–2122
Malyszko J, Bachorzewska-Gajewska H, Poniatowski B, Malyszko JS, Dobrzycki S (2009) Urinary and serum biomarkers after cardiac catheterization in diabetic patients with stable angina and without severe chronic kidney disease. Ren Fail 31(10):910–919
Waikar SS, Betensky RA, Bonventre JV (2009) Creatinine as the gold standard for kidney injury biomarker studies? Nephrol Dial Transplant 24(11):3263–3265
Premaratne E, MacIsaac RJ, Finch S, Panagiotopoulos S, Ekinci E, Jerums G (2008) Serial measurements of cystatin C are more accurate than creatinine-based methods in detecting declining renal function in type 1 diabetes. Diabetes Care 31(5):971–973
Hossain MA, Emara M, El Moselhi H, Shoker A (2009) Comparing measures of cystatin C in human sera by three methods. Am J Nephrol 29(5):381–391
Grubb A, Blirup-Jensen S, Lindstrom V et al (2010) First certified reference material for cystatin C in human serum ERM-DA471/IFCC. Clin Chem Lab Med 48(11):1619–1621
Shlipak MG, Sarnak MJ, Katz R et al (2005) Cystatin C and the risk of death and cardiovascular events among elderly persons. N Engl J Med 352(20):2049–2060
Shlipak MG, Wassel Fyr CL, Chertow GM et al (2006) Cystatin C and mortality risk in the elderly: the health, aging, and body composition study. J Am Soc Nephrol 17(1):254–261
Deo R, Fyr CL, Fried LF et al (2008) Kidney dysfunction and fatal cardiovascular disease—an association independent of atherosclerotic events: results from the Health, Aging, and Body Composition (Health ABC) study. Am Heart J 155(1):62–68
Shlipak MG, Katz R, Sarnak MJ et al (2006) Cystatin C and prognosis for cardiovascular and kidney outcomes in elderly persons without chronic kidney disease. Ann Intern Med 145(4):237–246
Ix JH, Shlipak MG, Chertow GM, Whooley MA (2007) Association of cystatin C with mortality, cardiovascular events, and incident heart failure among persons with coronary heart disease: data from the heart and soul study. Circulation 115(2):173–179
Koenig W, Twardella D, Brenner H, Rothenbacher D (2005) Plasma concentrations of cystatin C in patients with coronary heart disease and risk for secondary cardiovascular events: more than simply a marker of glomerular filtration rate. Clin Chem 51(2):321–327
Keller T, Messow CM, Lubos E et al (2009) Cystatin C and cardiovascular mortality in patients with coronary artery disease and normal or mildly reduced kidney function: results from the AtheroGene study. Eur Heart J 30(3):314–320
Muntner P, Mann D, Winston J, Bansilal S, Farkouh ME (2008) Serum cystatin C and increased coronary heart disease prevalence in US adults without chronic kidney disease. Am J Cardiol 102(1):54–57
Jernberg T, Lindahl B, James S, Larsson A, Hansson LO, Wallentin L (2004) Cystatin C: a novel predictor of outcome in suspected or confirmed non-ST-elevation acute coronary syndrome. Circulation 110(16):2342–2348
Windhausen F, Hirsch A, Fischer J et al (2009) Cystatin C for enhancement of risk stratification in non-ST elevation acute coronary syndrome patients with an increased troponin T. Clin Chem 55(6):1118–1125
Sarnak MJ, Katz R, Stehman-Breen CO et al (2005) Cystatin C concentration as a risk factor for heart failure in older adults. Ann Intern Med 142(7):497–505
Djousse L, Kurth T, Gaziano JM (2008) Cystatin C and risk of heart failure in the Physicians’ Health Study (PHS). Am Heart J 155(1):82–86
Moran A, Katz R, Smith NL et al (2008) Cystatin C concentration as a predictor of systolic and diastolic heart failure. J Card Fail 14(1):19–26
Ix JH, Shlipak MG, Chertow GM, Ali S, Schiller NB, Whooley MA (2006) Cystatin C, left ventricular hypertrophy, and diastolic dysfunction: data from the Heart and Soul Study. J Card Fail 12(8):601–607
Moran A, Katz R, Jenny NS et al (2008) Left ventricular hypertrophy in mild and moderate reduction in kidney function determined using cardiac magnetic resonance imaging and cystatin C: the multi-ethnic study of atherosclerosis (MESA). Am J Kidney Dis 52(5):839–848
Patel PC, Ayers CR, Murphy SA et al (2009) Association of cystatin C with left ventricular structure and function: the Dallas heart study. Circ Heart Fail 2(2):98–104
Tang WH, Van Lente F, Shrestha K et al (2008) Impact of myocardial function on cystatin C measurements in chronic systolic heart failure. J Card Fail 14(5):394–399
Arimoto T, Takeishi Y, Niizeki T et al (2005) Cystatin C, a novel measure of renal function, is an independent predictor of cardiac events in patients with heart failure. J Card Fail 11(8):595–601
Shlipak MG, Katz R, Fried LF et al (2005) Cystatin-C and mortality in elderly persons with heart failure. J Am Coll Cardiol 45(2):268–271
Alehagen U, Dahlstrom U, Lindahl TL (2009) Cystatin C and NT-proBNP, a powerful combination of biomarkers for predicting cardiovascular mortality in elderly patients with heart failure: results from a 10-year study in primary care. Eur J Heart Fail 11(4):354–360
Lassus J, Harjola VP, Sund R et al (2007) Prognostic value of cystatin C in acute heart failure in relation to other markers of renal function and NT-proBNP. Eur Heart J 28(15):1841–1847
Campbell CY, Clarke W, Park H, Haq N, Barone BB, Brotman DJ (2009) Usefulness of cystatin C and prognosis following admission for acute heart failure. Am J Cardiol 104(3):389–392
Manzano-Fernandez S, Boronat-Garcia M, Albaladejo-Oton MD et al (2009) Complementary prognostic value of cystatin C, N-terminal pro-B-type natriuretic peptide and cardiac troponin T in patients with acute heart failure. Am J Cardiol 103(12):1753–1759
Naruse H, Ishii J, Kawai T et al (2009) Cystatin C in acute heart failure without advanced renal impairment. Am J Med 122(6):566–573
Luc G, Bard JM, Lesueur C et al (2006) Plasma cystatin-C and development of coronary heart disease: the PRIME study. Atherosclerosis 185(2):375–380
Wu CK, Lin JW, Caffrey JL, Chang MH, Hwang JJ, Lin YS (2010) Cystatin C and long-term mortality among subjects with normal creatinine-based estimated glomerular filtration rates: NHANES III (Third National Health and Nutrition Examination Survey). J Am Coll Cardiol 56(23):1930–1936
Menon V, Shlipak MG, Wang X et al (2007) Cystatin C as a risk factor for outcomes in chronic kidney disease. Ann Intern Med 147(1):19–27
Shlipak MG, Katz R, Kestenbaum B et al (2009) Rate of kidney function decline in older adults: a comparison using creatinine and cystatin C. Am J Nephrol 30(3):171–178
Rifkin DE, Shlipak MG, Katz R et al (2008) Rapid kidney function decline and mortality risk in older adults. Arch Intern Med 168(20):2212–2218
Damman K, Voors AA, Navis G, van Veldhuisen DJ, Hillege HL Current and novel renal biomarkers in heart failure (under review)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lassus, J., Harjola, VP. Cystatin C: a step forward in assessing kidney function and cardiovascular risk. Heart Fail Rev 17, 251–261 (2012). https://doi.org/10.1007/s10741-011-9242-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-011-9242-6