Abstract
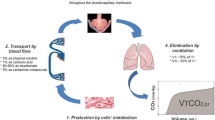
The aim of this study was to determine typical values for non-invasive volumetric capnography (VCap) parameters for healthy volunteers and anesthetized individuals. VCap was obtained by a capnograph connected to the airway opening. We prospectively studied 33 healthy volunteers 32 ± 6 years of age weighing 70 ± 13 kg at a height of 171 ± 11 cm in the supine position. Data from these volunteers were compared with a cohort of similar healthy anesthetized patients ventilated with the following settings: tidal volume (VT) of 6–8 mL/kg, respiratory rate 10-15 bpm, PEEP of 5–6 cmH2O and FiO2 of 0.5. Volunteers showed better clearance of CO2 compared to anesthetized patients as indicated by (median and interquartile range): (1) an increased elimination of CO2 per mL of VT of 0.028 (0.005) in volunteers versus 0.023 (0.003) in anesthetized patients, p < 0.05; (2) a lower normalized slope of phase III of 0.26 (0.17) in volunteers versus 0.39 (0.38) in anesthetized patients, p < 0.05; and (3) a lower Bohr dead space ratio of 0.23 (0.05) in volunteers versus 0.28 (0.05) in anesthetized patients, p < 0.05. This study presents reference values for non-invasive volumetric capnography-derived parameters in healthy individuals. Mechanical ventilation and anesthesia altered these values significantly.



Similar content being viewed by others
References
Bartels J, Severinghaus JW, Forster RE, Briscoe WA, Bates DV. The respiratory dead space measured by single breath analysis of oxygen, carbon dioxide, nitrogen or helium. J Clin Invest. 1954;33:41–8.
Fletcher R, Jonson B. The concept of deadspace with special reference to the single breath test for carbon dioxide. Br J Anaesth. 1981;53:77–88.
Breen PH, Isserles SA, Harrison BA, Roizen MF. Simple computer measurement of pulmonary VCO2 per breath. J Appl Physiol. 1992;72:2029–35.
Bohr C. Über die Lungeatmung. Skand Arch Physiol. 1891;2:236–8.
Tusman G, Suarez Sipmann F, Bohm SH. Rationale of dead space measurement by volumetric capnography. Anesth Analg. 2012;114:866–74.
Tusman G, Suarez Sipmann F, Bohm SH, Borges JB, Hedenstierna G. Capnography reflects ventilation/perfusion distribution in a model of acute lung injury. Acta Anaesthesiol Scand. 2011;55:597–606.
Tusman G, Bohm SH, Suarez Sipmann F, Scandurra A, Hedenstierna G. Lung recruitment and positive end-expiratory pressure have different effects on CO2 elimination in healthy and sick lungs. Anesth Analg. 2010;111:968–77.
Enghoff H. Volumen inefficax. Bemerkungen zur Frage des schädlichen Raumes. Uppsala Läkareforen Forhandl. 1938;44:191–218.
Fletcher R. Deadspace, invasive and non-invasive. Br J Anaesth. 1985;57:245–9.
Wagner P. Causes of high physiological dead space in critically ill patients. Crit Care. 2008;12:148–9.
Wolff G, Brunner JX, Weibel W, Bowes CL, Muchenberger R, Bertschmann W. Anatomical and series dead space volume: concept and measurement in clinical praxis. ACP Applied Cardiopulmonary Pathophysiology. 1989;2:299–307.
Tang Y, Turner MJ, Baker AB. Systematic errors and susceptibility to noise of four methods for calculating anatomical dead space from the CO2 expirogram. Br J Anaesth. 2007;98:828–34.
Tusman G, Scandurra A, Bohm SH, Suarez Sipmann F, Clara F. Model fitting of volumetric capnograms improves calculations of airway dead space and slope of phase III. J Clin Monitor Computing. 2009;23:197–206.
Tusman G, Suarez Sipmann F, Borges JB, Hedenstierna G, Bohm SH. Validation of Bohr dead space measured by volumetric capnography. Intensive Care Med. 2011;37:870–4.
Scherer PW, Gobran SJ, Baumgardner JE, Bartkowski R, Neufeld GR. Numerical and experimental study of steady-state CO2 and inert gas washout. J Appl Physiol. 1988;64:1022–9.
Kallet RH, Daniel BM, Garcia O, Matthay MA. Accuracy of physiological dead space measurements in patients with ARDS using volumetric capnography: comparison with the metabolic monitor method. Respir Care. 2005;50:462–7.
Fowler WS. Lung function studies II. The respiratory dead space. Am J Physiol. 1948;154:405–16.
Hlastala MP, Wranne B, Lenfant CJ. Cyclical variations in FRC and other respiratory variables in resting man. J Appl Physiol. 1973;34:670–6.
Verschuren F, Heinonen E, Clause D, Zech F, Reynaert MS, Liistro G. Volumetric capnography: reliability and reproducibility in spontaneously breathing patients. Clin Physiol Funct Imaging. 2005;25:275–80.
Breen PH, Isserles SA, Taitelman UZ. Non-steady state monitoring by respiratory gas exchange. J Clin Monit. 2000;16:351–60.
Hedenstierna G, Strandberg Å, Brismar B, Lundquist H, Svensson L, Tokics L. Functional Residual Capacity, Thoracoabdominal Dimensions, and Central Blood Volume during General Anesthesia with Muscle Paralysis and Mechanical Ventilation. Anesthesiology. 1985;62:247–54.
Hedenstierna G. Ventilation-perfusion relationships during anaesthesia. Thorax. 1995;50:85–91.
Brismar B, Hedenstierna G, Lundquist H, Strandberg Å, Svensson L, Tokics L. Pulmonary densities during anaesthesia with muscular relaxation - A proposal of atelectasis. Anesthesiology. 1985;62:422–8.
Terragni PP, Rosboch G, Tealdi A, Corno E, Menaldo E, Davini O. Tidal hyperinflation during low tidal volume ventilation in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2007;175:160–6.
Hofbrand BI. The expiratory capnogram: a measure of ventilation-perfusion inequalities. Thorax. 1966;21:518–24.
Blanch LL, Fernandez R, Saura P, Baigorri F, Artigas A. Relationship between expired capnogram and respiratory system resistance in critically ill patients during total ventilatory support. Eur Respir J. 1999;13:1048–54.
Schwardt JF, Gobran SR, Neufeld GR, Auk burg SJ, Scherer PW. Sensitivity of CO2 washout to changes in acinar structure in a single-path model of lung airways. Ann Biomed Eng. 1991;19:679–97.
Downie SR, Salome CM, Verbank S, Thompson B, Berend N, King GG. Ventilation heterogeneity is a major determinant of airway hyperresponsiveness in asthma, independent of airway inflammation. Thorax. 2007;62:684–9.
Tusman G, Böhm SH, Suárez Sipmann F, Turchetto E. Alveolar recruitment improves ventilatory efficiency of the lungs during anesthesia. Can J Anesth. 2004;51:723–7.
Åström E, Niklason L, Drefeldt B, Bajc M, Jonson B. Partitioning of dead space – a method and reference values in the awake human. Eur Respir J. 2000;16:659–64.
Fletcher R, Jonson B. Deadspace and the single breath test for carbon dioxide during anaesthesia and artificial ventilation. Effects of tidal volume and frequency of respiration. Br J Anaesth. 1984;56:109–19.
Ream RS, Schreiner MS, Neff JD, McRae KM, Jawad AF, Scherer PW, Neufeld GR. Volumetric capnography in children. Influence of growth on alveolar plateau slope. Anesthesiology. 1985;82:64–73.
Larson CP, Severinghaus JW. Postural variations in dead space and CO2gradients breathing air and O2. J Appl Physiol. 1962;17:417–20.
Severinhaus JW, Stupfel M. Alveolar deadspace as an index of distribution of blood flow in pulmonary capillaries. J Appl Physiol. 1957;10:335–48.
Schulz A, Schlz H, Heilmann P, Brand P, Heyder J. Pulmonary dead space and airway dimensions in dogs at different levels of lung inflation. J Appl Physiol. 1994;76:1896–902.
Hedenstierna G, McCarthy G. The effect of anaesthesia and intermittent positive pressure ventilation with different frequencies on the anatomical and alveolar deadspace. Br J Anaesth. 1975;47:847–52.
Nunn JF, Hill DW. Respiratory dead space and arterial to end-tidal CO2 difference in anesthetized man. J Appl Physiol. 1960;15:383–9.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was performed at Hospital Privado de Comunidad, Mar del Plata, Argentina and Hospital Italiano, Buenos Aires, Argentina.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tusman, G., Gogniat, E., Bohm, S.H. et al. Reference values for volumetric capnography-derived non-invasive parameters in healthy individuals. J Clin Monit Comput 27, 281–288 (2013). https://doi.org/10.1007/s10877-013-9433-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-013-9433-x