Abstract
OBJECTIVE: To compare the outcome of infants with respiratory distress syndrome (RDS) in the neonatal intensive care unit (NICU) who were extubated to synchronized nasal intermittent positive pressure ventilation (SNIPPV) or continued on conventional ventilation (CV), immediately postsurfactant.
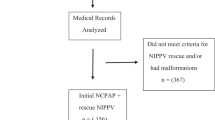
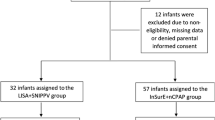
STUDY DESIGN: Prospective observational study of postsurfactant ventilatory management of consecutive infants (born between 10/99 and 12/02) of 28 to 34 weeks gestation. Extubation to SNIPPV was at the attending neonatologists' discretion. Babies in the CV group remained intubated, postsurfactant.
RESULTS: There were no significant differences in the maternal demographics, antenatal steroid use, mode of delivery, birth weight (BW), gestational age (GA), gender, Apgar at 5 minutes, age at surfactant instillation, or oxygenation index (OI) prior to surfactant administration, between infants continued on CV (n=35) and those extubated to SNIPPV (n=24). The total duration of endotracheal intubation (mean±SEM; CV versus SNIPPV; 2.4±0.4 versus 0.3±0.0 days, p=0.001) and duration of supplemental oxygen exposure (15±3.2 versus 8.2±3.3 days, p=0.04) were significantly shorter in the SNIPPV group. Furthermore, the duration of parenteral nutrition (12.1±1.6 versus 8.4±0.8 days, p=0.02) and length of stay (37.5±3.0 versus 29.1±3.3 days, p=0.04) were also significantly shorter in the SNIPPV group. There were no differences between the two groups in blood gas or OI values postsurfactant (up to 48 hours). There was no statistical difference in the incidence of intraventricular hemorrhage grade I (three (9%) in the CV group and two infants (8%) in the SNIPPV group). No infant died in either group or had patent ductus arteriosus, air leaks, necrotizing enterocolitis, periventricular leukomalacia, retinopathy of prematurity or bronchopulmonary dysplasia.
CONCLUSIONS: Infants of 28 to 34 weeks GA with RDS requiring surfactant with early extubation to SNIPPV had a shorter duration of intubation, and decreased need for oxygen as compared to CV. There was also a significant decrease in the duration of parenteral nutrition and hospitalization. SNIPPV is a safe and effective primary mode of ventilation in larger premature infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Mathews TJ, Menacker F, MacDorman MF . Infant mortality statistics from the 2000 period linked birth/infant death data set. Natl Vital Stat Rep 2002;50:1–28.
Northway Jr WH . Bronchopulmonary dysplasia: thirty–three years later. Pediatr Pulmonol 2001;23(Suppl):5–7.
Bhandari A, Bhandari V . Pathogenesis, pathology, and pathophysiology of pulmonary sequelae of bronchopulmonary dysplasia in premature infants. Front Biosci 2003;8:e370–90.
Bhandari V . High frequency ventilation in premature neonates with respiratory distress syndrome: does it make a difference?. In: Singhi S, editor. Current Concepts in Pediatric Intensive Care. Chandigarh: Relume Printec; 2000 p. 54–63.
Johnson AH, Peacock JL, Greenough A, et al. United Kingdom Oscillation Study Group. High-frequency oscillatory ventilation for the prevention of chronic lung disease of prematurity. N Engl J Med 2002;347:633–642.
Courtney SE, Durand DJ, Asselin JM, et al. Neonatal Ventilation Study Group. High-frequency oscillatory ventilation versus conventional mechanical ventilation for very-low-birth-weight infants. N Engl J Med 2002;347:643–652.
Craft AP, Bhandari V, Finer NN . The sy-fi study: a randomized prospective trial of synchronized intermittent mandatory ventilation versus a high-frequency flow interrupter in infants less than 1000 g. J Perinatol 2003;23:14–19.
Khalaf MN, Brodsky N, Hurley J, Bhandari V . A prospective randomized, controlled trial comparing synchronized nasal intermittent positive pressure ventilation versus nasal continuous positive airway pressure as modes of extubation. Pediatrics 2001;108:13–17.
Verder H, Robertson B, Greisen G, et al. Surfactant therapy and nasal continuous positive airway pressure for newborns with respiratory distress syndrome. N Engl J Med 1994;331:1051–1055.
Gittermann M, Fusch C, Gittermann A, Regazzoni B, Moessinger A . Early nasal continuous positive airway pressure treatment reduces the need for intubation in very low birthweight infants. Eur J Pediatr 1997;156:384–388.
Verder H, Albertsen P, Ebbesen F, et al. Nasal continuous positive airway pressure and early surfactant therapy for respiratory distress syndrome in newborns less than 30 weeks gestation. Pediatrics 1998;103:e24 http://www.pediatrics.org/cgi/content/full/103/2/e24.
Kamper J, Wulff K, Larsen C, Lindequist S . Early treatment with nasal continuous positive airway pressure in very low-birth-weight infants. Acta Paediatr 1993;82:193–197.
Friedlich P, Lecart C, Posen R, Ramicone E, Chan L, Ramanathan R . A randomized trial of nasopharyngeal-synchronized intermittent mandatory ventilation versus nasopharyngeal continuous positive airway pressure in very low birth weight infants after extubation. J Perinatol 1999;19:413–418.
Barrington KJ, Bull D, Finer NN . Randomized trial of nasal synchronized intermittent mandatory ventilation compared with continuous positive airway pressure after extubation of very low birth weight infants. Pediatrics 2001;107:638–641.
Papile LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with weight less than 1500 grams. J Pediatr 1978;92:529–534.
Volpe JJ . Hypoxic–ischemic encephalopathy: neuropathology and pathogenesis. In: Neurology of the Newborn. 3rd ed. Philadelphia, PA: WB Saunders; 1987 p. 291–299.
Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM . Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in neonatal period. Pediatrics 1988;82:527–532.
Bell MJ . Neonatal necrotizing enterocolitis therapeutic decisions based on clinical staging. Ann Surg 1978;187:1–7.
Anonymous. An international classification for retinopathy of prematurity. The Committee for the Classification of Retinopathy of Prematurity. Arch Ophthalmol 1984;102:1130–1134.
Santin R, Brodsky N, Bhandari V . A comparison of synchronized nasal intermittent positive pressure ventilation (SNIPPV) versus conventional ventilation (CV) immediately after surfactant instillation in infants with RDS. Pediatr Res 2002;51:337A (Abstract No. 1959).
Heimler R, Hoffmann RG, Starshak RJ, Sasidharan P, Grausz JP . Chronic lung disease in premature infants: a retrospective evaluation of underlying factors. Crit Care Med 1988;12:1213–12177.
Stoll BJ, Gordon T, Korones SB, et al. Late-onset sepsis in very low birth weight neonates: a report from the National Institute of Child Health and Human Development Neonatal Research Network. J Pediatr 1996;129:63–71.
De Paoli AG, Davis PG, Lemyre B . Nasal continuous positive airway pressure versus nasal intermittent positive pressure ventilation for preterm neonates: a systematic review and meta-analysis. Acta Paediatr 2003;92:70–75.
Jackson JK, Vellucci J, Johnson P, Kilbride HW . Evidence-based approach to change in clinical practice: introduction of expanded nasal continuous positive airway pressure use in an intensive care nursery. Pediatrics 2003;111:e542–e547. URL: http://www.pediatrics.org/cgi/content/full/111/4/e542.
Kiciman NM, Andreasson B, Bernstein G, et al. Thoracoabdominal motion in newborns during ventilation delivered by endotracheal tube or nasal prongs. Pediatr Pulmonol 1998;25:175–181.
Moretti C, Gizzi C, Papoff P, et al. Comparing the effects of nasal synchronized intermittent positive pressure ventilation (nSIPPV) and nasal continuous positive airway pressure (nCPAP) after extubation in very low birth weight infants. Early Hum Dev 1999;56:167–177.
Acknowledgements
We thank the other attending neonatologists at the Albert Einstein Medical Center NICU (Drs. Hallam Hurt, Rachel Porat, Mohammed Riaz, Agnes Salvador, Michael Szatkowski) for their support of the study. We also thank Drs. Richard Ehrenkranz and Anita Bhandari for their review of the manuscript.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Santin, R., Brodsky, N. & Bhandari, V. A Prospective Observational Pilot Study of Synchronized Nasal Intermittent Positive Pressure Ventilation (SNIPPV) as a Primary Mode of Ventilation in Infants ≥ 28 Weeks with Respiratory Distress Syndrome (RDS). J Perinatol 24, 487–493 (2004). https://doi.org/10.1038/sj.jp.7211131
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211131
This article is cited by
-
Nasal intermittent positive pressure ventilation versus nasal continuous positive airway pressure in neonates: A systematic review and meta-analysis
Indian Pediatrics (2013)
-
SNIPPV vs NIPPV: does synchronization matter?
Journal of Perinatology (2012)
-
Nasal intermittent positive pressure ventilation in the newborn: review of literature and evidence-based guidelines
Journal of Perinatology (2010)
-
Lung protective ventilatory strategies in very low birth weight infants
Journal of Perinatology (2008)
-
A randomized controlled trial of synchronized nasal intermittent positive pressure ventilation in RDS
Journal of Perinatology (2007)